As I wrote previously, there are three important questions when discussing COVID-19 Vaccine-Associated Myocarditis (C-VAM):
- How frequently does it occur?
- What are the clinical outcomes?
- How does this risk compare to that of the virus?
A recent pre-print by Dr. Tracy Hoeg et al. sought to answer some of these questions. Drs. Daniel Freedman and David Gorski recently discussed the problems with using Vaccine Adverse Event Reporting System (VAERS) to determine the rate of C-VAM. Please read their articles if you have not done so already. I was pleased to see in the comments section of these articles and on social media that Dr. Hoeg and her co-authors are taking these criticisms seriously. In this spirit, I would like to offer several additional critiques.
COVID-19 vaccine-associated myocarditis: The frequency
In addition to the criticisms of Drs. Freedman and Gorski, I would add that Dr. Hoeg’s paper does not mention any of the studies using the Vaccine Safety Datalink (VSD). The VSD is an active monitoring system that is directly linked to patients’ medical records. As such, it is not subject to the same limitations as VAERS, a passive monitoring system that contains unverified and possibly duplicate cases. As such, I feel their paper would be strengthened if it mentioned two studies that made use of this database.
- The CDC’s VSD report found the rate of myocarditis/pericarditis was 1 in 27,000 for children ages 12-17 years. If we assume that all cases occurred in boys, this yields a rate of 1 in 13,500.
- A study of 6.2 million individuals using safety surveillance data from VSD found a rate of 6.3 additional myocarditis cases per million doses during the first week after vaccination in people age 12-39 years old. Since almost all cases were in males, this translates to a rate of 1 in 79,000 for males in this age group.
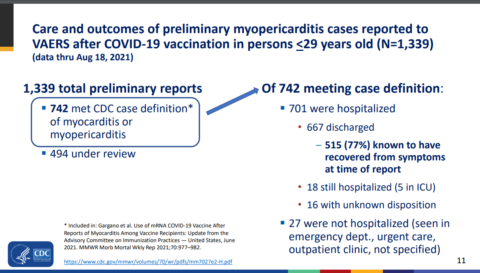
COVID-19 vaccine-associated myocarditis: Clinical outcomes
While the precise frequency of C-VAM in adolescents remains unclear, there is universal agreement from multiple sources that the clinical course is very favorable in the short-term. Dr. Hoeg’s paper states “the clinical course was reported to be relatively benign” and several case series are used to support this claim. I’m glad Dr. Hoeg included this information. I would add that the CDC has provided updated information from VAERS to the data presented in Dr. Hoeg’s paper, and this data continues to be generally reassuring. Unlike Dr. Hoeg’s team, the CDC reviewed the medical record of cases submitted to VAERS. In their most recent report, 701 out of 742 cases were admitted to the hospital. At the time of their report, all but 18 had been discharged home and 5 of these were in the ICU. Typically affected individuals are placed in the ICU for monitoring, and no affected adolescents have needed life support as far as I know. 77% had no symptoms at the time of the report.
Beyond this, multiple other sources, provided below, support the claim that C-VAM has a favorable short-term prognosis. I suggest that Dr. Hoeg include these in the references.
- The CDC’s VSD report gave information on 56 individuals, and all had been discharged home from the hospital, most after 1-2 days. 24 individuals were followed at least 7 days after discharge, and of these 6 still had at least one symptom.
- In the study of 6.2 million individuals using safety surveillance data from VSD, “82% were hospitalized (median length of stay, 1 day), and nearly all were recovered at record review”.
- “Patients resolved their symptoms rapidly”. (Marshall et al.)
- “Hospital course is mild with quick clinical recovery and excellent short-term outcomes”. (Jain et al.)
- The clinical course of vaccine-associated myocarditis-like illness appears favorable, with resolution of symptoms in all patients”. (Rosner et al.)
- “The clinical course was mild in all six patients”. (Mouch et al.)
- “All patients in our series remained clinically stable during a relatively short inpatient hospital stay”. (Patel et al.)
- “All patients had resolution of their chest pain, were discharged from the hospital in stable condition, and were alive with preserved left ventricular ejection fraction at last contact”. (Larson et al.)
- According to reports from Israel, “Most cases have been in the hospital for up to 4 days, and 95% are considered to be mild cases”.
- According to reports from Ontario, “Most cases appear to be mild and respond well to conservative treatment (e.g. non-steroidal anti-inflammatory drugs) and rest”.
Pediatricians who have treated these patients voice similar sentiments. Dr. Grace Lee, a pediatrician at Stanford, said, “This is not like any myocarditis I’m used to seeing”. Dr. Sallie Permar, the chair of pediatrics at Weill Cornell Medicine and New York–Presbyterian Komansky Children’s Hospital, said children are being hospitalized “because we wanted to monitor them, out of an abundance of caution…Even the kids are asking, ‘Why am I going to the hospital?'” Dr. James de Lemos, a professor of medicine, said, “They’ve all done well” and all recovered clinically after spending “just a couple of days” in the hospital. Dr. Pei-Ni Jone, a pediatric cardiologist, said, “The good news is, all these children recovered”.
Despite these positive reports, affected individuals felt unwell, with chest pain and often shortness of breath. To varying degrees, they have all had markers of cardiac injury. They will have to be monitored over the long-term for myocardial scarring, as this may pose a risk for future cardiac dysfunction. Additionally, they are advised to avoid physical activity for several months. As such, the condition should not be minimized.
The virus: Clinical outcomes, hospitalization rates
I found Dr. Hoeg’s discussion of the COVID-19’s harms particularly lacking. I suspect no one will be surprised to learn that I feel the paper understated both the harm of the virus and the efficacy of the vaccine. Several of authors have a history of applying different standards to the virus and the vaccine, in my opinion. One of the authors said that the “young have almost no risk” from the virus, and then later said myocarditis from the vaccine should never be called “mild“. Another suggested that RSV was being misdiagnosed as COVID-19 in hospitalized children, meaning COVID-19 wasn’t really that bad. I’ve written about this several times before. Another of the authors, Josh Stevenson, “is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates”. The pre-print did not make this fact known. So let me make my bias clear: I expected this paper to understate both the harm of the virus and the efficacy of the vaccine. I feel my expectations were met. Read my criticisms with this in mind.
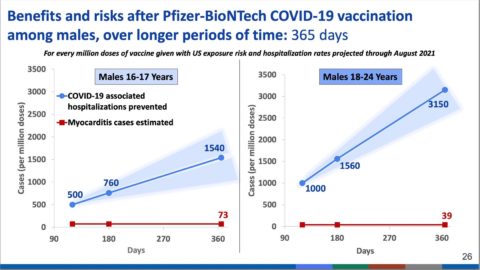
Dr. Hoeg’s paper compares those hospitalized from the vaccine with those hospitalized from the virus. Following a model used by the CDC, Dr. Hoeg compares hospitalization rates over a 120-day period. But there is nothing magical about 120-days, and zooming out over a longer time frame a bit brings more clarity. As of August 14th, 2021, 1 in 2,000 children in the US had been hospitalized according to the CDC. This means tens of thousands of American children have been hospitalized. Even if 40% of these were due to incidental COVID-19 cases (a complicated topic I discussed here), this rate still exceeds the highest rate of C-VAM in Dr. Hoeg’s study, which was about 1 in 6,200 boys age 12-15 years after the second vaccine dose. At present, an average of 344 children are hospitalized every day with COVID-19 in the US. While the number is decreasing slightly for the first time in a month, this is still well above the previous peak during January 2021.
Moreover, as one critic noted, “the study does not take into account differences in treatment practices when comparing hospitalisation rates between covid-19 infections and myocarditis and pericarditis presenting post-vaccination”. In other words, pediatricians may have different standards when deciding whether to admit a child with COVID-19 compared to a child with C-VAM. It’s conceivable that as pediatricians grow more familiar with C-VAM, they’ll decide that not all children need to be hospitalized.
Importantly, the benefits of the vaccine accrue over time, while its risks are contained within the first week. For this reason, the CDC also calculated the vaccine’s benefit at one-year, not just after 120 days. Unless the vaccine stops being effective at 120-days, a longer time frame provides a more realistic sense of the vaccine’s benefits. I believe Dr. Hoeg’s paper should discuss this further rather than simply note this as a limitation of its methods.
The virus: Clinical outcomes, hospitalization severity
Perhaps most glaringly, Dr. Hoeg’s paper provides no information on the clinical course of children and adolescents hospitalized with COVID-19. As with C-VAM, many children go home after a couple of days, seemingly on the way to full recovery. However, a significant minority are very sick. A CDC report found that:
Among 3,116 hospitalized children and adolescents with COVID-19 during March 1, 2020–June 19, 2021, for whom complete clinical data were available, 827 (26.5%) were admitted to an ICU, 190 (6.1%) required invasive mechanical ventilation, and 21 (0.7%) died. Among 164 hospitalized children and adolescents with COVID-19 during June 20–July 31, 2021, for whom complete clinical data were available, 38 (23.2%) were admitted to an ICU, 16 (9.8%) required invasive mechanical ventilation, and three (1.8%) died.
This just does not happen with the vaccine, though readers of Dr. Hoeg’s paper will remain largely ignorant of this fact. As one pediatric cardiologist said on Twitter,
I have yet to witness (and have asked my colleagues too) one post-vaccine myocarditis child go on life support. Have I heard of post-#COVID19 disease children get on life support, and MISC kids go on life support? Absolutely.
— Frank Han MD 🇺🇦Pediatric/ACHD/GUCH Cardiologist (@han_francis) September 10, 2021
The vaccine can keep children out of the hospital. In the clinical trials of adolescents (here and here) twenty subjects contracted COVID-19, all of them in the placebo group. Dr. Hoeg’s paper should report this. The vaccine is working in the real world. A study by the CDC found that unvaccinated adolescents are hospitalized 10 times more often than vaccinated ones. Dr. Hoeg’s paper should report this finding, which was published after the pre-print was written.
The virus: Clinical outcomes, MIS-C, and myocarditis
Dr. Hoeg’s paper states that in “the US, there have been 4404 multisystem-inflammatory syndrome in children (MIS-C) cases in a population of 74 million”. The current number is 4,661 cases, and this may be a substantial undercount. As Dr. Hoeg showed when calculating the rate of C-VAM, using a denominator other than the entire pediatric population of the US, gives a clearer view of the condition. One study calculated that MIS-C occurs in about 1 in 3,200 children infected with the virus. Again, this is a higher rate than the rate of C-VAM found in Dr. Hoeg’s paper.
Dr. Hoeg’s paper did not mention myocarditis as a complication of MIS-C. However, as I discussed previously, the cardiac complications of MIS-C are frequent and can be severe, including “shock, cardiac arrhythmias, pericardial effusion, and coronary artery dilatation”. Dr. Gautam Singh, chief of pediatric cardiology at Children’s Hospital of Michigan, who authored a study on cardiac dysfunction in children with MIS-C, said, “Almost invariably, half of them required going on mechanical ventilation or a breathing machine, heart-supporting medications.” He added that “When we studied these children and followed them about five to six months (later), we found about 19% to 20% have some involvement of their heart function that was not clinically obvious, but by echocardiographic measurements”. One review found that 6%-14% of children had persistent ventricular dysfunction when they left the hospital. Though more recent studies show that children with MIS-C do well in the long-run, 41 children have died of MIS-C in the US.
The virus can cause myocarditis in children independent of MIS-C. A study by CDC found that 1 in 754 children younger than 16 years with COVID-19 developed myocarditis, while the rate for their uninfected peers was 1 in 28,000. The risk of myocarditis for children under 16 years was therefore 37 times higher for children infected with COVID-19. Dr. Hoeg’s paper does not reference this study. However, it seems reasonable to me that long-term concerns about myocarditis due to the vaccine should also apply to myocarditis due to the virus.
The virus: Clinical outcomes, long-COVID
Dr. Hoeg discusses long-COVID in children by referencing a study that find “1.8% of children with symptomatic COVID-19 experiencing at least one symptom two months after infection compared with 0.9% of negatively”. Other, studies have found a higher rate of prolonged symptoms. One recent study from England found a much higher rate. It also found that infected children were twice as likely as uninfected children to report multiple symptoms such as headache and “unusual tiredness” 15 weeks later. While the exact rate of long-COVID is unknown, given that millions of children have contracted the virus in the US, I can safely say a large number of children felt really sick for several weeks. This is a new virus, and we have to be humble about its potential long-term sequelae.
The virus: Clinical outcomes, deaths
Dr. Hoeg’s paper reports a pediatric mortality rate from England of six per million infections, though no explanation is given as to why this one country is considered an appropriate standard for reference. After all, in less-resource rich countries, children have died in much greater numbers (e.g. Indonesia and Brazil). In the US, where all of the paper’s authors are based, roughly 1 in 50,000 children who contracted COVID-19 have died from it, though the exact fatality rate is unknown. Children clearly die at a very low rate, but given the large number of children who contracted the virus, this translates to a significant number of dead children in my opinion. Around 500 American children have died thus far, and the American Academy of Pediatrics added 102 deaths to their tally since July 29th 2021. I suggest that Dr. Hoeg report these numbers, not just the fatality rate from another country.
About 25% of young people who die have no underlying medical condition (and common conditions such as obesity and asthma are the most common underlying conditions in those who die of COVID-19). As such, most deceased children, even those with an underlying condition, were robbed of many decades of life. Sadly, adolescents who were eligible for the vaccine have died since the vaccine became available to them. (here, here, here, here, here, here, here, here, here, here, here, here, here, here, here, here, here, here, here, and here).
In contrast, the CDC investigated the deaths of several adolescents and concluded that none were related to the vaccine, though six are still under investigation. Thus far, 8.9 million adolescents have been vaccinated. People should know this.
Conclusion: Assess the risks of the vaccine and the virus
It’s not easy to write about children, COVID-19, and the vaccine. There’s a lot we don’t know, the pandemic is a dynamic, unpredictable target, and new information emerges all the time. Several of the papers I referenced previously came out after Dr. Hoeg’s pre-print. There’s plenty of room for nuance and good-faith disagreement. A healthy teen in Norway does not have the same risk as an obese teen in Florida. A child who recovered from the virus does not have the same risk as one who has never been exposed. Several countries are vaccinating adolescents with just one vaccine dose. This will reduce their risk C-VAM, but will leave them more vulnerable to the virus. This strikes me as an entirely reasonable balance in places where most adults have been vaccinated and the virus isn’t spreading out of control. Soon we will be having a similar discussion for children younger than 12-years.
Determining the best course of action necessitates a thorough and comprehensive review of all available data. The risks of the vaccine shouldn’t be minimized or maximized. The risks of the virus shouldn’t be minimized or maximized. We need to be as clear as possible about the risks we are facing. Though the vast majority of children do well, the virus can be really bad for a small percentage of children. I believe that anyone who writes about COVID-19 and children has an obligation to make this very clear.
Dr. Hoeg’s paper does not do this. Even if it nailed the rate of V-CAM, its omissions of key facts means that overall, it obscures more than it clarifies. Dr. Hoeg and her colleagues have repeatedly stated they are pro-vaccine and welcome feedback on their pre-print. As such, I hope that when the final version of their paper is published in a peer-reviewed medical journal, pertinent information will not be omitted. Sadly, even if these omissions are rectified in the final version of their paper (which has already been rejected from three journals), it won’t get nearly the same attention as the pre-print. That cat is out of the bag.