We have long argued that the most effective medicine is science-based medicine, ongoing efforts of alternative and “integrative” medicine advocates to promote placebo medicine notwithstanding. Unfortunately, a depressing number of physicians do not share this philosophy, resulting in the rise of a specialty known as “integrative medicine” and “subspecialties” of quackery like “integrative oncology.” We have also long bemoaned one of the consequences of this increasing acceptance, namely the infiltration of quackery into medical schools and academic medical centers, a phenomenon for which Dr. R. W. Donnell coined the term “quackademic medicine” nearly 16 years ago. Although its proponents like to bill “integrative medicine” as being the “best of both worlds,” combining the benefits of science- and evidence-based medicine with the supposed benefits of medicine not based in science and evidence, in reality and practice, integrative medicine involves “integrating” quackery like homeopathy, acupuncture, naturopathy, reiki and “energy medicine,” and more with medicine. As Mark Crislip has long put it:
So integrative medicine is taking rank pseudo-scientific nonsense and combining it with real medicine. That is why I say, when you integrate cow pie with apple pie, the cow pie is not made better, the apple pie is made worse.
A recent study (hat tip: Edzard Ernst) examining attitudes of physicians in Europe who embrace alternative medicine modalities “integrated” into medicine in “integrative medicine” has yet again reinforced just how correct Dr. Crislip was when he first wrote these immortal words. It also describes just how common both the embrace of various forms of quackery and antivax are among physicians in the countries studied. It is a cross-sectional study by a team of researchers from Germany, France, Finland, and Portugal. including a co-author with whom regular readers of this blog might be familiar: Stephan Lewandowsky, who co-authored an excellent lay primer on conspiracy theories, examining attitudes among physicians who have vaccination responsibilities in the four countries from which the authors hale. The results are depressing but instructive.
Unscientific medicine is associated with unscientific views towards vaccination, prologue
In the introduction, the authors lay out the rationale for the study:
Prior studies among the general population and nurses suggest that complementary and alternative medicine (CAM) is positively related to vaccine hesitancy.9–14 CAM is defined by the World Health Organization as “a broad set of health care practices that are not part of that country’s own traditional or conventional medicine and are not fully integrated into the dominant health care system”15—in Western societies: homeopathy, acupuncture, energy and crystal healing, reflexology, magnet therapy, or anthroposophic medicine.16–18 Due to its potential effect on willingness to recommend and receive vaccines, the analysis of the relationship between vaccine hesitancy and CAM endorsement among physicians is particularly relevant due to their direct contact with the general public and vulnerable populations, as well as to their key role in patients’ vaccine-related decision-making processes.19,20.
I can’t help but note here that the authors seem to be using an outdated term: CAM, which was often used in years past to describe adding alternative medicine and non-science-based medicine to science- and evidence-based medicine. However, alternative medicine advocates didn’t like the term CAM because it placed alternative medicine as “complementary,” meaning something secondary added to medicine, the “cherry on top,” if you will. In other words, it was an implicit admission in the name that the “alternative medicine” was ineffective (or at least far less effective) compared to the actual medicine. That’s why around 15 years ago CAM was “rebranded” as “integrative medicine” and the even vaguer and more general term “integrative health” arose. They imply the “integration” of “equals,” or the true “best of both worlds” in the alternative medicine belief system. Integrative medicine practitioners still (usually) don’t use the quackery alone, but rather with evidence-based medicine, but now they approach the modalities as co-equals even though they most definitely are not.
Whatever term is being used—CAM, integrative medicine, integrative health, or any of the other euphemisms for integrating quackery with medicine—the authors sought to examine the correlation between CAM beliefs and vaccine hesitancy (or antivaccine) beliefs, noting:
Despite studies reflecting physicians’ general dissatisfaction with the state of knowledge and research about CAM,21,22 a literature review of 21 survey-based studies in Canada and the U.S. found that a substantial number of HCPs express positive attitudes toward CAM and recommend, or would consider recommending, CAM to their patients—e.g., between 6% and 80% used CAM in their clinical practice, with these results varying depending on the definition of CAM and sampling methods used in the study.23 In fact, one systematic review suggested that HCPs are equally, or even more likely, than the general population to use CAM.24 Another systematic review, this time of surveys with British physicians, found that the mean prevalence of personal use of CAM among physicians was 20.6%, with an average referral rate to CAM of 39%, even though only 10.3% of these physicians had received specific training in CAM.25 Other studies conducted in European countries show a similar scenario. For example, in the study by Berretta et al.26 55% of the sample of Italian physicians recommended CAM to their patients, whereas in the German sample analyzed in the study by Linde et al.27 23% of family physicians, 6% of internists, and 31% of orthopedist personally used four or more forms of CAM frequently, and 68% reported using homeopathy to treat patients.
This summary of existing evidence with respect to physicians and CAM is truly disheartening to be reminded of, but not at all surprising to those of us who have been paying attention to the increasing infiltration of unscientific medicine into medicine under the rubric of CAM or “integrative medicine.” Seriously, if you are a physician and use homeopathy—or, as I like to call it, “The One Quackery To Rule Them All”—you need to go back to medical school to learn basic biochemistry and pharmacology. In fact, you need to go back to college and take a basic physics class. Of course, it’s not entirely surprising that homeopathy is so popular among German physicians given that the man who invented it nearly 230 years ago, Samuel Hahnemann, was German. Unfortunately, as a result, homeopathy continues to be viewed very favorably in Germany.
The authors of the current study also reiterate something that we’ve long pointed out here at SBM, namely how among the general public acceptance of the alternative medicine treatments commonly used in CAM correlates with negative views towards vaccines:
The link between CAM endorsement and negative attitudes toward vaccines has been documented in previous research among the general public. A systematic review, which categorized arguments against vaccines retrieved from peer-reviewed articles and debunking texts published by international fact checking agencies, identified a category of arguments largely based on alternative health beliefs related to CAM.28 This category was the third most common in the scientific and fact-checking literature. Furthermore, anti-vaccination arguments related to CAM were also among the most endorsed arguments by individuals from the British general population in a study by Holford et al.29 These results suggest that CAM beliefs play an important role in individuals’ justification of their hesitant attitudes toward vaccines for both adults and children.30 Bryden et al.,31 Soveri et al.,12Lewandowsky et al.,11 and Hornsey et al.10 analyzed samples from the Australian, Finnish, American, and Spanish general populations and found that positive attitudes toward CAM were related to negative attitudes toward vaccines. In a recent large-scale study in 18 European countries, parental consultation with homeopaths was associated with higher vaccine hesitancy than consultation with pediatricians or nurses.32 Moreover, in a systematic review, Wardle et al.33 found that CAM use tended to be positively associated with lower childhood immunization – see the work by Bleser et al.34 and Frawley et al.35 for more recent results from the U.S. and Australia.
I was most interested in reference 28 cited above because it is a recent paper about the taxonomy of antivax arguments mapped to eleven common alternative medicine beliefs and attitudes. Unfortunately, my library does not carry the journal, so I’m still waiting for the article through interlibrary loan and can’t comment about it other than by the abstract. However, I will be curious to see how closely the findings resemble things that I’ve been saying all along—also, whether I need to alter my beliefs on this based on new evidence or can just use this article going forward as evidence supporting those beliefs.
In any event, it is not even controversial that belief in unscientific medicine of the sort “integrated” into medicine by “integrative medicine” is associated with vaccine hesitancy and even outright antivax beliefs among the general public. But what about physicians? That’s what the study cited by Prof. Ernst set out to try to quantify by testing two hypotheses, H1 and H2:
H1:
CAM endorsement among medical practitioners with vaccination responsibilities will predict negative vaccination attitudes and behaviors.
Following the well-established theory of planned behavior, according to which behaviors are influenced by previous attitudes in a process of sense-making,Citation36 we also hypothesized that negative attitudes toward vaccines associated with CAM endorsement would constitute a motivational context in which physicians’ willingness to recommend and receive vaccinations is reduced:
H2:
Attitudes toward vaccines will mediate the relationship between CAM endorsement and vaccine-related behaviors.
Let’s dig in.
Unscientific medicine is associated with unscientific views towards vaccination, the study
One thing about this study that interested me is when the survey was done to assess the attitudes of physicians towards CAM and vaccines: between 03/31/2022 and 04/24/2022 via Schlesinger Group Germany; between 04/06/2022 and 05/06/2022 through invitations sent to the mailing list of the Portuguese Society of Pediatricians and the Portuguese Association of General Practice and Family Medicine; between 03/18/2022 and 04/27/2022 in France through invitations sent to the mailing list of National Association of General Practitioners; and in Finland, GPs between 04/25/2022 and 05/16/2022. This was a period of time after the initial wave of hope and enthusiasm about COVID-19 vaccines and right about when antivax sentiments toward the mRNA vaccines had risen markedly and attitudes linking antivax views with ideological and political orientations had hardened.
Instruments assessing attitudes towards CAM and towards vaccines were used on a sample of 2,875 physicians, of which 88 were excluded due to missing values on one or more variables of interest, resulting in a final sample of 2,787 participants. The instrument measuring attitudes towards CAM was a five-item scale measuring CAM rejection developed by Lewandowsky et al., with 2 items taken from Hyland et al. The authors listed sample items, which included: “complementary medicine builds up the body’s own defenses, so leading to a permanent cure” and “complementary medicine is superior to conventional medicine in treating chronic ailments such as allergies, headaches, and back pains.”
For vaccine attitudes, the authors used the international version of the Professionals Vaccine Confidence and Behaviors Questionnaire (I-Pro-VC-Be), which is composed of 33 items to measure psychosocial determinants of HCPs’ attitudes toward vaccines, which are grouped into six constructs, described thusly:
-
Confidence in Vaccines, composed of items reflecting perceived risks of vaccines (i.e., how safe HCPs perceive certain vaccines to be), complacency (i.e., the perception of lack of usefulness of vaccines), perceived benefit-risk balance of vaccines (i.e., the degree to which HCPs perceive that the benefits of vaccines outweigh their potential risks), and perceived collective responsibility (i.e., the extent to which HCPs recommend vaccines to contribute to community immunity). Sample items: “vaccines against human papillomaviruses are safe” and “the benefits of the vaccine against measles outweigh its potential risks.”
-
Trust in Authorities (i.e., trust in institutions and health authorities to provide reliable vaccine information and to define the vaccination strategy). Sample items: “I trust the information provided by the [relevant national institution] about the risks and benefits of vaccines” and “I trust the [relevant national institution] to establish the vaccination strategy.”
-
Perceived Constraints (i.e., perceived practical constraints, such as cost of or access to vaccines). Sample items: “the cost of some vaccines is a problem for some patients and can keep me from prescribing them” and “the lack of availability of certain vaccines in my country is sometimes a problem that can keep me from prescribing them to my patients.”
-
Proactive Efficacy, composed of items reflecting commitment to vaccination (i.e., the extent to which HCPs are proactive in motivating their patients to accept vaccinations) and self-efficacy (i.e., how prepared HCPs feel in terms of knowledge and skills to address vaccination with patients). Sample items: “I am committed to developing the skills needed to communicate better with my patients about vaccination” and “I feel comfortable discussing vaccines with my patients who are highly hesitant about vaccination.”
-
Reluctant Trust (i.e., the “leap of faith” to trust vaccines and policies even if HCPs have doubts). Sample items: “I may sometimes recommend vaccines from the official schedule even if I feel I am not sufficiently informed” and “I may sometimes recommend the vaccines on the official schedule even in cases where I have doubts about their safety.”
-
Openness to patients. These items express positive attitudes toward hesitant patients, such as viewing their concerns regarding vaccination as legitimate, letting patients to delay the immunization of children, and a neutral approach to informing patients about the benefits of vaccines. Sample items: “patients who are hesitant about the benefits and risks of vaccines have legitimate questions” and “I am open to patients delaying immunization of their children.”
So what did the investigators find when they looked at these variables and assessed the participants vaccine-related behaviors, including:
- Vaccine recommendations to patients. Sample question: “Please imagine you are treating an adult who has not had the COVID-19 vaccine and has no contraindications. How likely is it that you would recommend the vaccine to the patient?”
- Self-vaccination against influenza and COVID-19 during the previous three years.
- General vaccination behavior. Sample question: “How often do you check that your patients have received the vaccines recommended for them (whether from records or asking)?”
Regarding the first hypothesis (positive attitudes and behaviors with respect to CAM will predict vaccine behavior and negative attitudes towards vaccines), the investigators used a linear mixed effects model and found that the results “support our hypothesis that CAM endorsement among medical practitioners with vaccination responsibilities predicts negative vaccination attitudes and behaviors.” The second hypothesis (that attitudes toward vaccines will mediate the relationship between CAM endorsement and vaccine-related behaviors) was also supported:
The results indicate that Confidence in Vaccines constitutes a significant mediator and that its mediational role is particularly strong for the relationship between CAM Endorsement and Vaccine Recommendation, accounting for 84% of the association (R2 = 0.27). Furthermore, Confidence in Vaccines accounts for 56% of the association between CAM Endorsement and Self-Vaccination (R2 = 0.16). These mediations were robust across countries, albeit the indirect effects were particularly strong in Germany (see Supplementary Material), and support our hypothesis that attitudes toward vaccines mediate the relationship between CAM Endorsement and vaccine-related behaviors.
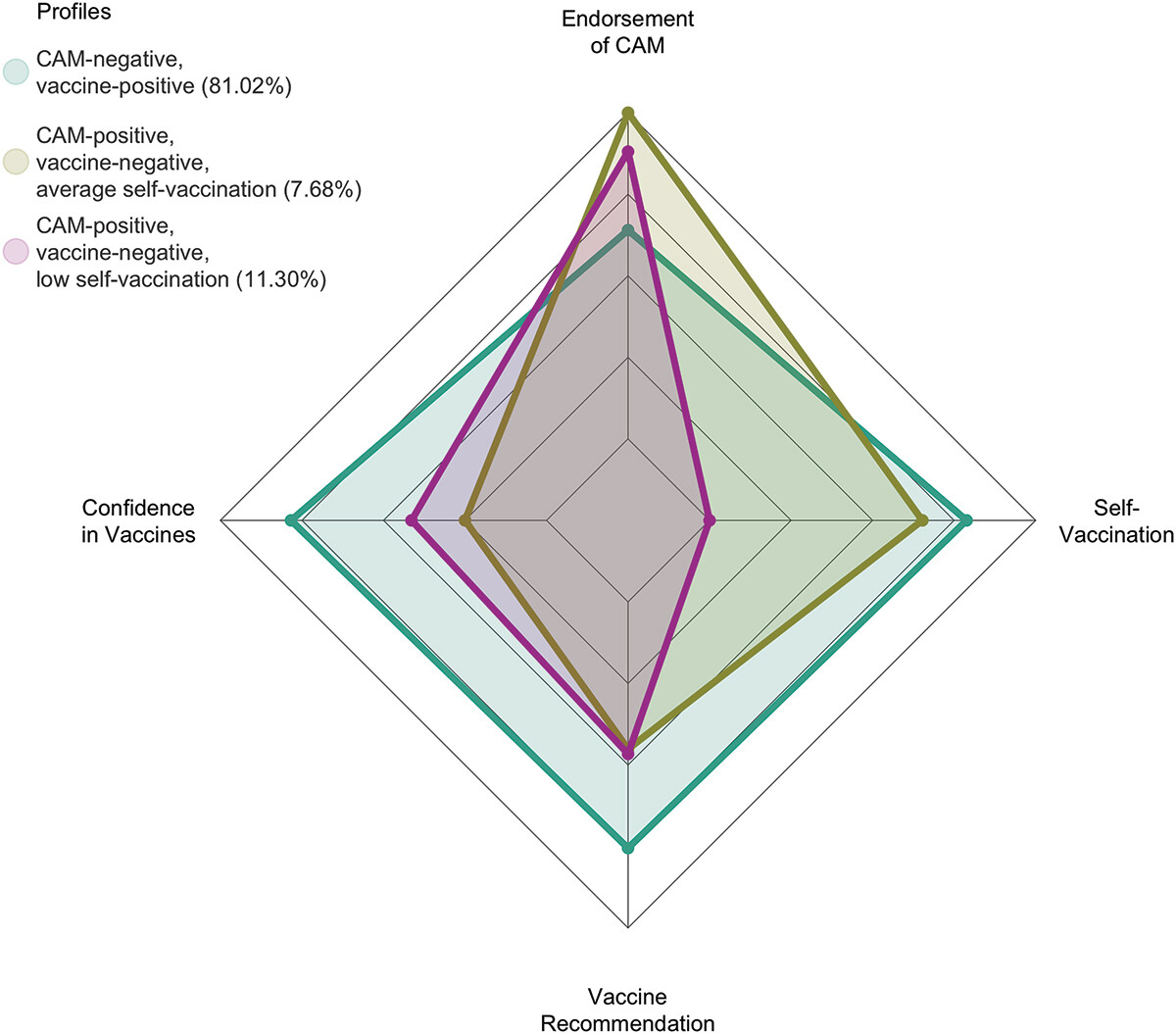
The finding that most interested me, however, was the finding of latent profiles among physicians with respect to their attitudes towards CAM and vaccines. In brief, latent profile analysis is an analytical approach that focuses on identifying latent subpopulations within a population based on a certain set of variables, assigning people with varying degrees of probabilities into categories that have different configural profiles of personal and/or environmental attributes. In this case, the latent profile analysis sought to characterize the physicians in the sample into categories based on “the number of participants expressing higher-than-average CAM Endorsement and lower-than-average Confidence in Vaccines, Vaccine Recommendation, and Self-Vaccination.”
The authors identified three latent profiles in their subjects:
My first reaction was that I suppose I should be happy that 81% of the physicians surveyed fell into the CAM-negative, vaccine-positive profile. However, that means that the other 19% fell into CAM-positive, vaccine-negative profiles, the majority of whom also exhibited low levels of self-vaccination; in other words, they practice what they preach.
Unsurprisingly, the percentage of physicians who fell into the CAM-positive/vaccine-negative profiles varied between countries:
- 24% in Germany
- 18% in France
- 10% in Finland
- 6% in Portugal
Apparently, if you want science-based recommendations with respect to alternative medicine and vaccines in Europe, your best bet is a Portuguese doctor and your worse bet is a German doctor. In fairness, these profiles are defined by averages, as in below average confidence in vaccines and above average confidence in CAM. There is variability. Even so, these percentages of CAM-positive/vaccine-negative physicians are alarming high, even in Portugal.
This study has a number of strengths, not the least of which is that it is a large sample. However, the authors concede that it is unclear how representative their samples are of the physicians in each country and therefore how generalizable their findings are. In addition, the mediation analyses are correlations and can’t by themselves prove causation, although I would point out that we have a lot of other evidence from other sources and studies that suggest probable causation. Finally, the study was not particularly granular. CAM was treated as a single category, even though the popularity of different CAM modalities no doubt differed between countries.
Unscientific medicine is associated with unscientific views towards vaccination, what now?
I’ve long pointed out the strong association between belief in quackery and antivaccine views and how often quacks are at least highly vaccine-averse if not outright antivaccine. The authors lay out some potential reasons for their findings in their Discussion, and I can’t help but agree with much of their reasoning:
Ernst47 proposed several potential causes for the observed relationship between vaccine hesitancy and CAM.9–12,14,48 Since CAM use occurs more frequently at the poles of the disease spectrum (i.e., in cases of minor or life-threatening illness), CAM use has been identified as a marker of both misperception of risk and frustration with regular healthcare (e.g., negative prognosis or lack of remission of symptoms).49 Accordingly, CAM-related health conceptions could be motivating HCPs to be more reluctant to recommend and receive vaccinations both for illnesses that are perceived as minor and in cases of severe clinical pictures. There are also reasons related to the potential alignment between CAM and the ideology or worldview of the HCP, such as their distrust in “Big Pharma” or a general disregard for scientific knowledge.50 Along the same lines, Attwell et al.51 found in semi-structured interviews with vaccine hesitant Australian parents that the main reasons for their preference for CAM included a greater affinity between CAM, their do-it-yourself approach to health care, and their sympathy for natural and harm-free products in contrast to medications marketed by pharmaceutical companies, which were perceived as ineffective, “toxic” and “adulterating.”52
All of these are topics that have been extensively discussed here on SBM, in particular the affinity of CAM for the “natural” and the seeming belief that vaccines are “unnatural” or even something that “contaminates” the “purity” of one’s “natural” body. (It’s the reason why I frequently use clips like the clips below of Gen. Ripper ranting about the dangers of fluoridation of water and how “they” wanted to fluoridate much more—”ice cream, Mandrake, children’s ice cream!”—from the six decade old classic movie, Dr. Stangelove, or: How I Stopped Worrying and Learned to Love the Bomb.
Yes, I’ve argued that both CAM and antivax ideology amount to, in essence, a purity cult requiring ritual purification, a.k.a. in CAM parlance, “detoxification.”
As I also like to say, the end of the second clip also partially explains why antivaxxers think that women should not have sex with vaccinated men, namely because their “purity of essence” will be contaminated or corrupted, because the male’s “corrupted essence” will be passed on through sex.
Also, there are many beliefs within CAM that are incompatible with science, but more specifically with the science behind vaccination, as the authors further note:
Besides these implicit reasons, some CAM traditions are theoretically incompatible with vaccination and portrayed as a valid, or even superior, alternative to scientific knowledge.51 A quantitative study found that pro-CAM and anti-vaccination attitudes both reflect beliefs contrary to basic scientific knowledge, such as “an imbalance between energy currents lies behind many illnesses” and “an illness should be treated with a medicine that has properties similar to those of the illness.”31,53 An example of these CAM-related beliefs that contradict the theoretical basis of vaccinations is “homeopathic immunization” through so-called “nosodes” – orally administered extreme dilutions of infectious agents.54 Similarly, Rudolf Steiner and Ryke Geerd Hamer, promoters of anthroposophic medicine and German new medicine, respectively, have sown doubts about vaccinations based on their conceptions of the etiology and treatment of diseases.55 Consequently, strong science denial and vaccine hesitancy can be found within these communities,56,57 and outbreaks of vaccine-preventable diseases, such as measles and whooping cough, have been reported in educational centers linked to anthroposophy.58
This correlation resulting in the phenomenon of CAM being linked to outbreaks of vaccine-preventable disease is something that we’ve discussed for a long time, a discussion that has continued since COVID-19 arrived in 2020. But why are there such differences between nations in the percentage of CAM-positive/vaccine-negative physicians? The authors note several potential reasons. Germany, for instance, has recognized natural health practitioners (heilpraktiker) since the late 1930s, something we’ve discussed before and something that Prof. Ernst has often mentioned. It is also common for German physicians to provide CAM – around 60% in some surveys, cited by the authors. The authors also note that CAM is embedded in the French healthcare system; indeed, recall right before the pandemic how French physicians speaking out against homeopaths and their quackery and formed fake médecine to combat homeopathic quackery were threatened with the suspension of their medical licenses. All is not bad in France, though, as the country recently stopped reimbursing its citizens for homeopathic treatments in 2021. In contrast, CAM is not integrated into the Finnish or Portuguese healthcare system, supporting our longstanding contention here at SBM that government regulation and incentives matter—a lot.
There are many examples of physicians for whom the linkage between alternative medicine and antivax beliefs is clear, something I’ve started calling a seamless simultaneous embrace of quackery and antivax views. For instance, the “early COVID-19 treatment” doctors (such as America’s Frontline Doctors and the Frontline COVID-19 Critical Care Alliance) started out promoting “early treatment” protocols for COVID-19 that often involved repurposed drugs plus a panoply of supplements, basically a CAM approach to treating COVID-19. Now, they are fully antivaccine. In the other direction are doctors like Dr. Peter McCullough, who started out being against COVID-19 mitigations, moved on to become anti-COVID-19 vaccine to the point of embracing the conspiracy theory that the vaccines were causing young people—even athletes!—to “die suddenly,” and then became fully antivaccine, who now hawks supplements containing nattokinase and bromelain to treat “spike protein” toxicity due to COVID-19 or, more commonly, the bogus claim that COVID-19 vaccine poison you with spike protein. Then there’s Tess Lawrie, who went from supporting ivermectin to COVID-19 antivaccine beliefs to an outright embrace of homeopathy. The list goes on.
The bottom line to me, though, is that the integration of quackery into medicine through the specialty of “integrative medicine” or “integrative health” has a malign influence on more than just the science of medicine. It represents a direct threat to public health not only through its undermining of the scientific basis of medicine, but how that undermined science results in increasing distrust of vaccines by physicians that will inevitably contribute to increasing distrust of vaccines and public health among their patients. Unfortunately, the alignment of believers in CAM and antivaccine beliefs with powerful right wing ideological interests has made the likelihood of increasing acceptance and tolerance of quackery in medicine more, not less, likely.