 This year’s Nobel Prize in Physiology or Medicine goes to three researchers, William G. Kaelin Jr, Sir Peter J. Ratcliffe and Gregg L. Semenza, “for their discoveries of how cells sense and adapt to oxygen availability.” You can read an in-depth discussion of the science here, but I would like to give a summary and highlight some broader implications of this research.
This year’s Nobel Prize in Physiology or Medicine goes to three researchers, William G. Kaelin Jr, Sir Peter J. Ratcliffe and Gregg L. Semenza, “for their discoveries of how cells sense and adapt to oxygen availability.” You can read an in-depth discussion of the science here, but I would like to give a summary and highlight some broader implications of this research.
The researchers elucidated the specific mechanisms by which cells sense and react to the presence or absence of oxygen. Oxygen is obviously a critical substance for life and its delivery to all tissue as well as physiological processes dependent on oxygen need to be carefully regulated by the body. But how does this all work?
Previously it was known that the carotid bodies in the arteries in the neck that deliver blood to the brain can sense low oxygen levels and in response send signals to the heart to increase blood flow and pressure. The brain generally has priority when it comes to blood, oxygen, and nutrient delivery, and so if the brain is getting enough oxygen, the rest of the body probably is also. This is an immediate-response system.
There are also longer-term responses that react to chronic hypoxia (when tissues do not have enough oxygen to meet their needs). One response is to grow new blood vessels to deliver more blood to the tissue. The other is to release a hormone called erythropoietin (EPO), which is made in the kidneys. EPO increases the production of red blood cells, which contain the oxygen-carrying hemoglobin that delivers oxygen to tissues. So if you move to a higher altitude with lower partial pressures of oxygen, your body will react by making more red blood cells until a new equilibrium of oxygen delivery is reached.
This is the part of the story where the three researchers come in – they were instrumental in elucidating the precise mechanisms by which various tissues sense and respond to oxygen levels. Semenza and Ratcliffe both studied the EPO gene to see how oxygen was related to its regulation. They both found oxygen sensing machinery in all tissues, so this is a basic function of all cells, not just the kidney cells that make EPO.
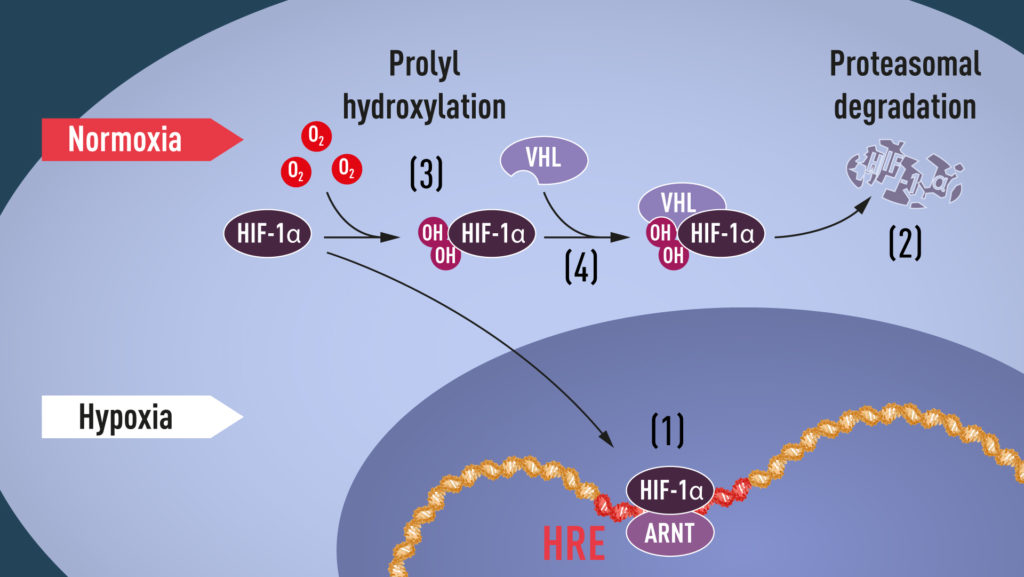
Semenza discovered a protein complex he called “hypoxia-inducible factor” (HIF). Semenza further discovered that HIF is comprised of two transcription factors, now called HIF-1α and ARNT. A transcription factor controls the rate at which proteins are made from specific genes. This was starting to make sense. Semenza’s work led to other research that discovered when oxygen levels decreased HIF-1α levels increased, which increased the transcription of the EPO gene, making more of the hormone. Other researchers also discovered that the enzyme (called a proteasome) that degrades HIF-1α is dependent on oxygen. So when oxygen levels are low, the rate at which HIF-1α breaks down is decreased, and so levels increase, thereby increasing EPO levels and finally red blood cell levels.
But there was still one more piece to this puzzle – how does oxygen affect the degradation of HIF-1α by the proteasome? This is where Kaelin comes in. He was researching the effects of oxygen on cancer cells, specifically in the genetic disease von Hippel-Lindau’s disease (VHL disease). This is a genetic disease that predisposes people to certain cancers. Kaelin found that the VHL gene prevents the onset of cancer, and is linked to higher levels of hypoxia-regulated proteins. Further, the VHL protein is needed to tag other proteins with ubiquitin, which marks them for degradation. So without VHL the degradation of certain proteins is decreased, so their levels rise.
This is now where Ratcliffe comes in. He discovered that VHL interacts with HIF-1α, and is necessary for the degradation of HIF-1α at normal oxygen levels. Finally, both Ratcliffe and Kaelin simultaenously discovered that at normal oxygen levels hydroxyl groups are added at two specific positions in HIF-1α, allowing VHL to bind and mark HIF-1α for degradation. This was the final connection between oxygen and the function of these proteins, indicating at least one mechanism by which cells can sense the relative levels of oxygen.
This research has implications for cancer research. Cancer cells have to adapt or have mutations that allow them to thrive even in hypoxic conditions, and/or to increase their oxygen supply. Interrupting these mechanisms is one way to attack cancer cells. This research can also potentially have implications for stroke, anemia, wound healing, and certain infections.
We can speculate, but it is always difficult to predict exactly what will come from basic science research like this. These three researchers, and the many others that were involved in this research, were simply trying to understand a basic function of biology, to satisfy their curiosity, and to increase our collective knowledge. There didn’t have to be a direct utility to their research. But these kinds of discoveries create the potential for new mechanisms of treatment.
This research also highlights the fact that biological systems are complex webs that exist in dynamic equilibrium states. It’s important to remember this whenever we think about potential new interventions. Simplistic notions that if something is low we will just increase it and have a predictable benefit without downsides are often naïve (although sometimes things do work this way – we just have to be careful). We have to think of our interventions in the context of interacting with an existing equilibrium.
Sticking with oxygen as an example, if someone with chronic lung disease (COPD) has low oxygen levels, and you supplement their oxygen, they may stop breathing. Chronic high levels of CO2 may have made their feedback drive for breathing insensitive to CO2, which means low oxygen levels are driving their breathing. Take that away and they stop breathing. This is actually a relatively simple example, but it shows the general principle.
Oxygen sensing is also important not just for normal physiological functioning, but for development as well. This highlights the fact that develop itself is a feedback system. Genes are not blueprints telling cells exactly how to build a person, but rather a set of processes that will unfold to develop a person. Blood vessels, for example grow based only partly on a basic anatomical plan, but mainly in response to hypoxia. Wherever there is low oxygen, grow more blood vessels to deliver more oxygen until an optimal equilibrium is reached.
This general principle is good to keep in mind when being sold supplements or other interventions based on simplistic notions of more is always better.

