Like many people I’ve suffered from occasional back pain, on and off, for years. And when I’ve had acute pain, I’ve taken non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil). Working 12-hour shifts, always on my feet, led me to some debilitating back pain. And while I’ve never found NSAIDs to be miracle drugs, I did find they were providing some pain relief. After taking them for a multi-week spell when I was really uncomfortable, I found myself diagnosed with a stomach ulcer. Once I healed, I’ve found regular exercise (particularly strength training) seems to keep the back pain at bay. I haven’t had a bad bout for years.
We may think nothing of popping a few Advil now and then, but NSAIDs have been linked to about 30% of drug-related hospital admissions, and it’s estimated that 12,000-16,000 Americans die annually as a result of gastrointestinal bleeding caused by NSAIDs.
As a pharmacist I’ve also seen first hand the devastating impact that narcotics can have on people as well. The awareness of the potential harms of opioids is much more prevalent, among health professionals and consumers, than it was 10-20 years ago.
While there have been good developments in non-narcotic treatments for conditions like migraine, there is still a lot of pain that’s treated with “conventional” drug therapy – analgesics, anti-inflammatories, and narcotics. Given none of these products actually fix the underlying cause of the pain and given their toxicity, it’s understandable there’s interest and enthusiasm for non-drug approaches to pain control. A new paper confirms that growing interest over a 20 year period.
A new paper from Richard L Nahin and colleagues at the NIH (National Center for Complementary and Integrative Health) examines responses from the 2002, 2012, and 2022 National Health Interview Survey (NHIS), which is a household interview survey done annually and nationally. The survey had the same questions about acupuncture, guided imagery and/or progressive muscle relaxation, massage, naturopathy, and yoga in the three periods. Questions on chiropractic care and meditation were worded very differently differently in 2012, limiting comparison. Typical questions looked like:
- During the past 12 months, did you see a practitioner for acupuncture?
- For what health problems or conditions did you use acupuncture?
- During the past 12 months, did you see a practitioner for naturopathy?
- For what health problems or conditions did you use naturopathy?
Utilization of Complementary Approaches Overall
Outcomes were the changes over time in use of any of the seven complementary health approaches, and each complementary approach for any reason, and for pain management. Here are the results:
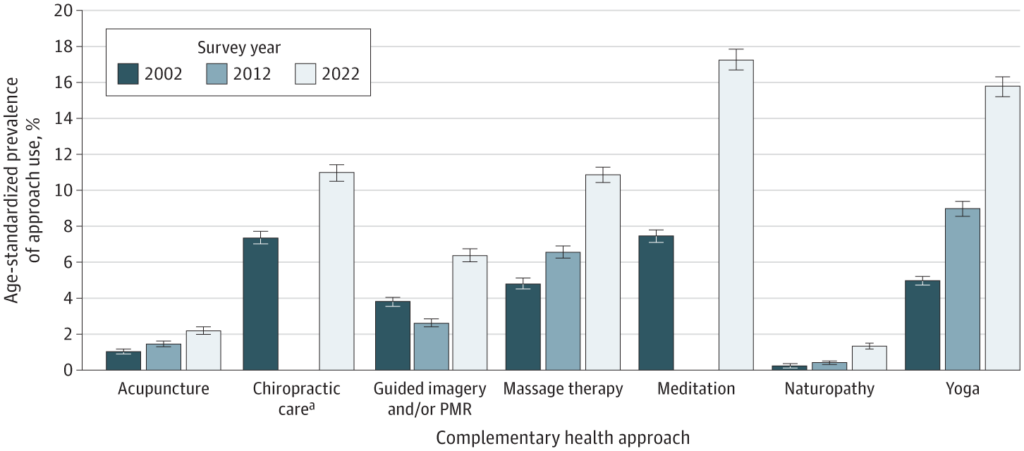
Between 2002 and 2022, there was a significant increase in the utilization of all approaches. All individual modalities experienced significant upward trends. The overall prevalence of using any of the seven approaches rose from 19.2% to 36.7%. Yoga exhibited the largest increase, growing from 5.0% in 2002 to 15.8% in 2022. Meditation had the highest prevalence in 2022, with 17.3% of individuals reporting its use. Acupuncture rose from 1.0% in 2002 to 2.2% in 2022. There was little utilization of naturopathy, but it did grow as well.
Utilization of Complementary Approaches for Pain Control
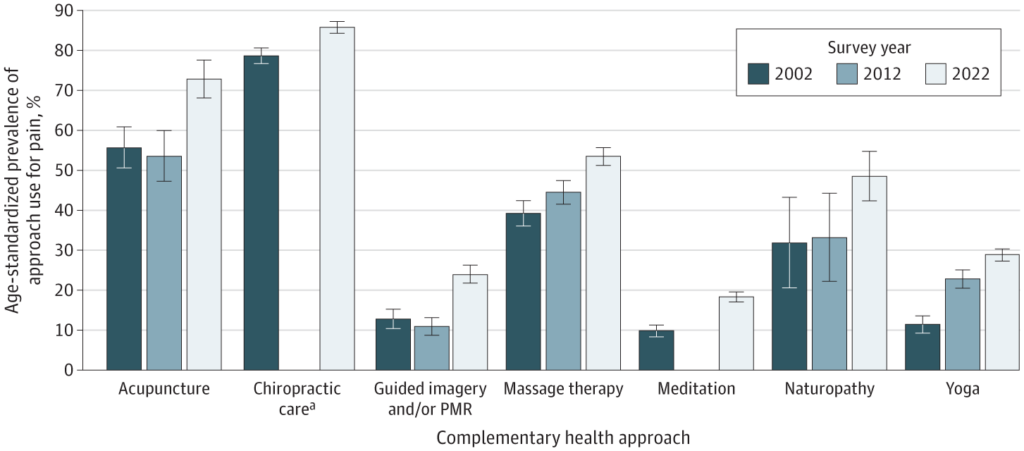
Among those using any of the seven complementary approaches, reports of use for pain management increased significantly from 42.3% in 2002 to 49.2% in 2022. All individual approaches showed statistically significant increases in use for for pain management. Yoga was associated with the largest increase, rising from 11.4% in 2002 to 28.8% in 2022. Chiropractic care had the highest overall usage for pain management, with 85.7% of individuals reporting its use in 2022.
Conclusion
The overall effectiveness of these different types of treatments have been covered in multiple posts in the past, so I won’t rehash the evidence here, other than to say that the evidence supporting them is weak. Nevertheless, over 20 years, there has been an increasing use of all of them, often for pain management. This aligns with a national increase in pain prevalence reported – which is arguably a subject for another post. This survey doesn’t outline why these approaches are gaining in popularity, but the belief that these approaches are effective, and sometimes endorsed in pain management guidelines, may be a factor. Growing insurance coverage (even for arguably ineffective interventions, like acupuncture) may also be contributing to more utilization. I suspect that there is also a growing desire to reduce the use of drug therapy, which in many circumstances is completely appropriate. With a growing prevalence of Americans suffering from pain, we should expect interest to continue to grow in different treatment options.

