
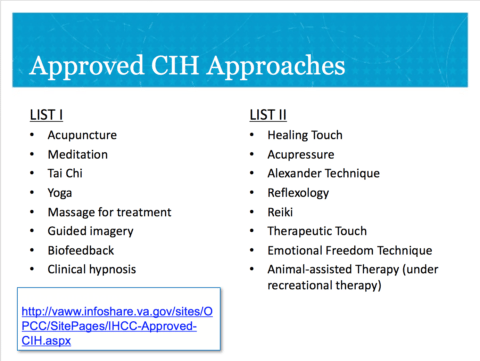
The Veterans Health Administration (VHA) has announced (VHA Directive 1137: VA Provision of Complementary & Integrative Health) that acupuncture, reiki, and reflexology, among other “complementary and integrative health [CIH] practices” will now be included in the standard veterans’ medical benefits package. [Translation: You, the taxpayer, will foot the bill.] The VHA found “adequate evidence exists to support the use” of some of these CIH practices, despite their own evidence review showing otherwise (“List I”). These must be offered at all VHA medical facilities, either on-site or by referral to community providers. Other CIH approaches (“List II”) will be included in veterans’ medical benefits because they “are generally considered to be safe,” any pretense of efficacy having been totally abandoned; whether to offer them at any particular facility is optional.
(Aromatherapy has since been added to List II.)
To make it easy, the VHA has created its own codes for inclusion of CIH in the VHA system: “RFLX” for reflexology; “CGQC” for Qi Gong, and so on. (For codes, see the CIH resource guide) And so enthused is the VHA about this new endeavor, it’s offering a bonus to veteran’s health facilities for promoting it, according to this VA powerpoint. Facilities will receive up to $7,000 in additional funds per veteran if he or she receives 10 CIH visits in one fiscal year.
Borrowing from the quackademic medicine playbook, this mandate is wrapped in the protective coating of what the VHA calls the “Whole Health System,” the definition of which is adapted from the Academic Consortium for Integrative Medicine and Health:
Whole Health is patient centered care that affirms the importance of the relationship and partnership between a patient and their community of providers . . . This approach is informed by evidence and makes use of all appropriate therapeutic approaches, healthcare professionals and disciplines.
In other words, it is no different from the biosocial model of medicine, except that, like “integrative medicine,” it incorporates:
a full range of conventional and complementary and integrative health.
As David Gorski has pointed out regarding integrative medicine, it is, in short, an excuse to incorporate quackery into conventional medical care. And as with quackademic medicine, conventional modalities like exercise (tai chi, yoga) and massage are somehow rebranded as “integrative.”
This is appalling enough on principle alone. In addition to the ethical issues posed by integration of pseudoscience into medical care, funding for veteran medical care is a zero-sum game. Congress allocates a finite amount of money to the VA, so monies absorbed by, say, therapeutic touch, do not get spent on, for example, cognitive behavioral therapy for PTSD. But, however willing the VHA might be to sidestep the ethical and financial implications, it cannot ignore federal regulatory requirements for veterans’ medical care. In my view, the VHA has done just that, a point we’ll return to in a moment.
Acupuncture tops the list
Mandating unproven treatments for veterans is the culmination of a long-term campaign by integrative medicine ideologues, like Wayne Jonas (also here) and Tracy Gaudet, the current director of the VHA’s Office of Patient Centered Care and Cultural Transformation, who aspire to dumb down evidence of safety and efficacy to accommodate pseudoscience. For integrative medicine advocates, the maxim “extraordinary claims require extraordinary evidence” is turned on its head: extraordinary claims (e.g., that humans can transfer an undetectable “energy” to one another; that our bodily functions are controlled by “qi“) require no evidence. Thus, this from a RAND Evidence Map of Acupuncture, published in 2014 by the VA:
In general, acupuncture is the stimulation of specific acupuncture points through penetration of the skin with needles, which aims to correct imbalances in the flow of qi, a concept of energy in traditional Chinese medicine (TCM), through meridians (i.e., energy channels.)
Nowhere in this 48-page report do the authors question the concept that ill health is the result of imbalances in our qi, even though, after “thousands” of years, no one has ever demonstrated that this qi and its meridians exist. Studying it is a perfect example of Tooth Fairy Science, that is, doing research on a phenomenon before you establish that the phenomenon exists.
Yet studied it has been: there are thousands of published acupuncture studies. And the evidence is? According to the Evidence Map authors:
the effectiveness and adverse events associated with acupuncture are not firmly established [and] [r]esults from existing reviews of reviews about the effectiveness of acupuncture are non-conclusive.
Nothing in this Evidence Map constructed for the VA mitigates those conclusions. In fact, the authors specifically state that their report:
was not designed to inform policies regarding the use of acupuncture.
But note which CIH “approach” (the VHA avoids the terms “treatments” and “therapies” when discussing CIH) is number one on List I: Acupuncture. In fact, so enamored of acupuncture is the VHA that it is now making arrangements to hire acupuncturists as regular VA employees.
As Benjamin Kligler, MD, MPH, the VHA’s Integrative Health Coordinator, explains in a November 4, 2017, article in (where else?) Medical Acupuncture:
A major initiative is now underway to expand CIH nationally, with a primary focus on a number of CIH therapies with the best evidence of effectiveness, including acupuncture . . . [Emphasis added.]
And what is this “best evidence of effectiveness?” According to a VHA CIH Directive Memo signed by Kligler on Oct. 26, 2017, it’s really just:
published evidence of promising or potential benefit. [Emphasis added.]
And where is this “published evidence?” According to the VHA, it’s the aforementioned RAND Evidence Map of Acupuncture.
In sum, the VHA is including acupuncture in veterans’ medical benefits and directing all VHA facilities to provide it based on a conclusion it has “promising or potential benefit” even though it’s been told not to make policy grounded in that conclusion and even though the RAND report clearly states the evidence is “non-conclusive.”
(Unfortunately, I cannot link to the VA document citing the Evidence Map in support of mandating acupuncture because it is not publicly available, although you can find the Evidence Map cited here by the VHA as supporting its offering CIH.)
To add insult to injury, VHA acupuncture offerings will presumably include so-called “Battlefield Acupuncture” (BFA, or, in VHA coding parlance, “IACT”). BFA is a fabrication of Col. Richard Niemtzow, who based it on auricular acupuncture. Despite the fact that BFA is ludicrously implausible and there is no evidence it is effective for anything, the VHA, according to Dr. Kligler:
has rolled out large-scale training [in BFA]. . . . To date, more than 1000 providers have been trained in BFA . . . and we have more than 50 BFA VHA instructors trained as well.
Is that even legal?
While we can quibble over whether List I modalities like guided imagery, hypnosis, and biofeedback are “conventional” or “integrative,” there is no doubt that List II, with the exception of animal-assisted therapy and the Alexander Technique (although it has little evidence of effectiveness), is full-blown quackery.
But before we move on, you’re probably wondering: Where’s chiropractic? Not to worry: it’s not on any list because it is already fully covered in VA medical benefits, thanks to Congress, which was successfully lobbied by the American Chiropractic Association to include it.
Healing touch, reiki and therapeutic touch are all forms of “energy medicine,” based on the notion that one person can channel “healing energy” into another, with positive health benefits. It hardly bears mentioning that energy medicine is both highly implausible and its benefits remain unproven. Reflexology is based on the equally fanciful notion that the body is divided into 10 longitudinal energy zones that end in the hands and feet. The reflexologist claims that by massaging these zones, she can heal disease and otherwise alter bodily functions. As Mark Crislip observed:
Safe to say that the basic premises of reflexology have no bearing in reality.
Acupressure is, as the name implies, applying pressure to acupuncture points, and, by extension, suffers from the same lack of plausibility and evidence of effectiveness as acupuncture itself. Emotion Freedom Technique is based on the notion that blockages in our “energy fields” result in health problems, which can be resolved by a series of taps on the sufferer’s “energy meridians.” Aromatherapy is the use of essential oils with therapeutic intent, but without evidence that they are effective.
Of course, the VHA doesn’t claim that List II CIH approaches are effective, merely that they are safe. (Oddly, they adopt the FDA standard for food additives as their definition of safety.) And therein lies their legal problem.
Federal regulations prescribe the type of care covered in the veterans’ medical benefits package. This includes such routine items as periodic exams, immunizations, surgery, nutritional counseling, medical equipment and the like, with this caveat:
Care referred to in the “medical benefits package” will be provided to individuals only if it is determined by appropriate healthcare professionals that the care is needed to promote, preserve, or restore the health of the individual and is in accord with generally accepted standards of medical practice. [Emphasis added.]
In VHA Directive 1137, mentioned earlier, the VHA states that List I and List II CIH practices:
meet the definition of care in 38 CFR 17.38(b), thereby making them suitable for inclusion in VA’s medical benefits package
Meaning they, in the VHA’s view, promote, preserve or restore health and are in accord with generally accepted standards of medical practice. (The Directive also says that “conventional medicine and CAM should be held to the same standards for validating clinical effectiveness.” So much for that idea.)
Two problems with meeting these criteria immediately present themselves. First, if a practice lacks evidence of effectiveness, as many of these do, how can they be said to “promote, preserve or restore health” unless the VHA is willing to accept anything that elicits a placebo response as promoting, preserving or restoring health?
Second, it is highly doubtful that battlefield acupuncture, reflexology, energy healing, acupressure and Emotional Freedom Technique meet “generally accepted standards of medical practice” as that term is commonly understood.
“Generally accepted standards of medical practice” is not defined in the regulation. However, because government regulations are presumed to use words and phrases in accord with their normal meaning, we can look to how other responsible authorities have defined the term. The National Academies of Science quoted these definitions with approval:
Based on credible scientific evidence published in peer-reviewed medical literature generally recognized by the relevant medical community, or otherwise consistent with the standards set forth in policy issues involving clinical judgment. (Kaminiski, 2007)
Known to be effective in improving health outcomes. For new interventions, effectiveness is determined by scientific evidence. For existing interventions, effectiveness is determined first by scientific evidence, then by professional standards, then by expert opinion (Singer et al., 1999)
In an article on utilization management, the authors used the definition:
“generally accepted standards of medical practice” means standards that use clinical guidelines that are based on credible scientific evidence published in peer-reviewed medical literature generally recognized by the relevant medical community; [i.e., Evidence Based Medicine] (taking into account Physician Specialty Society recommendations, the views of Physicians practicing in the relevant clinical areas, and any other relevant factors) when making medical necessity determinations.
Finally, according to Cigna, a large health insurance company:
“generally accepted standards of medical practice” means:
- standards that are based on credible scientific evidence published in peer-reviewed, medical literature generally recognized by the relevant medical community;
- Physician Specialty Society recommendations;
- the views of Physicians practicing in the relevant clinical area; and
- any other relevant factors.
Simply put, nothing on List II meets these criteria and, arguably, acupuncture (and perhaps others on List I that I didn’t review) doesn’t either. I propose that this makes the VHA’s decision subject to a legal challenge as being in conflict with the federal regulations governing what can be included in veterans’ medical benefits.
A recent RAND report, Complementary and Alternative Medicine in the Military Health System, showed that over 80% of military treatment facilities already offer some form of CAM services. The same report said that 64%-84% of facilities cited evidence or clinical practice guidelines in support of CAM recommendations. Yet, the report also reveals that acupuncture is used for stress management, anxiety disorder and sleep disturbance, conditions for which there is insufficient evidence for acupuncture use. The report also shows that military health system already spends millions of dollars each year on provision of CAM services.
Use of CIH, or CAM, or whatever term you might prefer, will only increase under the VHA’s new mandate. Further inappropriate use of CIH “approaches” and a drain of fiscal resources away from proven treatments will naturally follow, evidence and regulations be damned.

