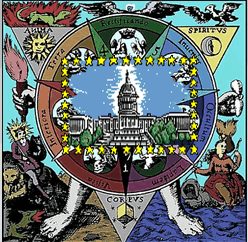
Legislative Alchemy
Acupuncture is a theatrical placebo. Its proposed mechanism of action is highly implausible and:
after decades of research and more than 3000 trials, acupuncture researchers have failed to reject the null hypothesis, and any remaining possible specific effect from acupuncture is so tiny as to be clinically insignificant.
In layman’s terms, acupuncture does not work – for anything.
Even the very CAM-friendly National Center for Complementary and Integrative Health (NCCIH), in its own weasel-worded way, comes close to conceding the point:
Research suggests that acupuncture can help manage certain pain conditions, but evidence about its value for other health conditions is uncertain. [Emphasis added.]
Somebody tell the state legislatures. Via the magic of Legislative Alchemy, 47 states have legalized the practice of acupuncture along with, in some cases, Traditional Chinese, Oriental or East Asian medicine. In several states, acupuncture practice acts describe acupuncturists as primary care practitioners and/or give them the authority diagnose and treat any condition or disease. For example, in my state, Florida, the practice act says that acupuncture:
means a form of primary health care, based on traditional Chinese medical concepts and modern oriental medical techniques, that employs acupuncture diagnosis and treatment, as well as adjunctive therapies and diagnostic techniques, for the promotion, maintenance, and restoration of health and the prevention of disease. [Emphasis added.]
In Nevada,
“Acupuncture” means the insertion of needles into the human body by piercing the skin of the body to control and regulate the flow and balance of energy in the body and to cure, relieve or palliate:
(a) Any ailment or disease of the mind or body; or
(b) Any wound, bodily injury or deformity. [Emphasis added.]
And in New Mexico:
“doctor of oriental medicine” means a person licensed as a physician to practice acupuncture and oriental medicine with the ability to practice independently, serve as a primary care provider and as necessary collaborate with other health care providers . . .
“oriental medicine” means the distinct system of primary health care that uses all allied techniques of oriental medicine, both traditional and modern, to diagnose, treat and prescribe for the prevention, cure or correction of disease, illness, injury, pain or other physical or mental condition by controlling and regulating the flow and balance of energy, form and function to restore and maintain health. [Emphasis added.]
As with state chiropractic and naturopathic licensing, most states rely on a closed-loop system of education and examinations that is completely controlled by acupuncturists in determining who is qualified to become licensed. The National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) administers the certification exams recognized by the states. Applicants for certification must have either graduated from schools accredited by the Accreditation Commission for Acupuncture and Oriental Medicine (ACAOM) or foreign schools meeting criteria set by the NCCAOM.
While the ACAOM is approved as an accrediting agency by the U.S. Department of Education, the Department does not review the scientific validity of what is taught or perform any independent analysis of the graduates’ ability to competently and safely practice. Its focus is on administrative matters and the financial stability of the schools. The ACAOM standards do not require a college degree for admission to an accredited acupuncture/Oriental Medicine school and only 500 hours of supervised patient care are required in accredited programs to graduate with a Master’s in acupuncture (700 hours for a Master’s in Oriental Medicine). A Master’s allows one to sit for the NCCAOM exam. In sum, someone with no college degree and 500 hours of clinical training can become a “primary care provider” in some states.
2017 bills
Today we look at bills filed in eleven states to license, or expand the practice of, acupuncturists during the 2017 state legislative sessions. Six were successful. Two bills were defeated; three remain pending.
Prior to last year, acupuncturists did not have a practice act in Wyoming. This year they succeeded in gaining one, although the Wyoming legislature stopped short of giving them the right to practice Oriental Medicine, which was eliminated in the final bill. Acupuncture is somewhat narrowly defined as inserting needles, with or without electric current or heat, into the body for:
therapeutic purpose of promoting, maintaining and restoring health, including [but, we note, not limited to] the treatment of dysfunctions of the body involving pain.
Wyoming also joins several states who’ve been bamboozled into thinking sticking needles into peoples’ ears, otherwise known as “auricular acupuncture,” is effective for substance abuse and mental health issues. Promoted based on an unpublished and cherry-picked review of the evidence by an organization called the National Acupuncture Detoxification Association (NADA), it is a perennial favorite with state legislatures looking to address mental health issues and drug abuse on the cheap.
New Hampshire enacted legislation creating something called a “Certified Acupuncture Detoxification Specialist,” who must be trained in the NADA protocol and supervised by an acupuncturist, although the “Specialist” needn’t be an acupuncturist himself. They can use “acu-detox” for:
behavioral health applications, including addictions, mental health, and disaster and emotional trauma.
One version of the bill specified that “acu-detox” could be used only in conjunction with other therapies but that bit of consumer protection against the ineffectiveness of pseudoscience in treating serious conditions was rejected.
Likewise, in Maine, a new law requires the state Department of Health and Human Services to develop a pilot project that will treat alcohol and substance abuse using the unproven NADA protocol. Fortunately, more sober minds prevailed in West Virginia, where a bill allowing the practice of NADA auricular acupuncture for chemical dependency failed.
Like their fellow CAM practitioners, naturopaths and chiropractors, once licensed, acupuncturists will return again and again to the state legislatures for practice expansion. In 2017, they succeeded in a big way in Illinois. There the legislature added the practice of “East Asian” medicine to the acupuncturists’ scope of practice, defined to include needle acupuncture, moxibustion, herbal medicine, and dietary supplements, among others, to:
normalize physiological functions, or for the treatment of diseases or dysfunctions of the body.
Acupuncture itself is broadly defined to include not only traditional needle acupuncture, but also far-infrared, electro- and magnetic stimulation, cold laser, cupping, dry needling (discussed below), and the bruising massage practice known as gua sha:

Apparently his Chi wasn’t up to par. From Bradwesley69 on the Wikimedia Commons.
In a move reminiscent of the chiropractic lobby’s efforts to make chiropractic schools the arbiter of what chiropractors can and cannot do, Illinois practitioners of acupuncture and East Asian medicine are permitted to perform a differential diagnosis via principles and techniques taught in acupuncture schools, like the fanciful tongue and pulse diagnosis.
Acupuncture: ineffective but treats everything
Illinois practitioners must refer patients to a physician or dentist if the patient’s condition is beyond their scope of practice, which raises and interesting question: Just what is beyond the East Asian medicine/acupuncture practitioner’s scope of practice when he is permitted to perform a differential diagnosis (albeit based on total pseudoscience) and treat, without limitation, “diseases or dysfunctions of the body”?
If you consult the Acufinder acupuncture referral website, you’ll find acupuncture’s usefulness in treating disease is virtually unlimited:
Acupuncture and Chinese medicine are extremely successful in the treatment of a multitude of conditions. Many people try Acupuncture and Oriental Medicine as a “last resort” to serious and complex medical problems and find that it can help them when other treatments could not.
Acupuncture is also often used as a preventative medicine. Many people see their acupuncturist only 2-4 times a year for a “tune up” or “balancing” treatment. This can prevent disease and promote health, energy and vitality.
“While no means a complete list of what Acupuncture and Traditional Chinese Medicine can treat,” Acufinder lists, among many others, allergies, anemia, depression, high blood pressure, heart disease, bronchitis, impotence, infertility, fibrosis, candida, Epstein Barr virus, lupus, hepatitis, stroke, polio, emphysema and diabetes. No evidence is cited for any of these claims.
Acufinder is, by the way, on Heatlhline’s list of “Best Blogs: Alternative Medicine 2017.” Healthline, which is Hon@Code certified, apparently has a high tolerance for quackery. Sayer Ji’s GreenMedinfo blog, which our good friend Orac has anointed one of the “quackiest, crankiest sites on the Internet” (sample post: “The Homeopathic Answer to Mumps”) also made the list.
If we can’t trust Acufinder, how about a more responsible source for determining what acupuncture can successfully treat? How about the University of Miami’s Miller School of Medicine? Unfortunately, in a perfect example of “infiltrative pseudoscience,” the University agrees with Acufinder on a number of diseases and conditions “for which acupuncture is effective” or for which, more vaguely, “people commonly find acupuncture treatment to be effective,” including allergies, asthma, depression, high blood pressure, impotence, Bell’s palsy, infertility, heart disease, bronchitis, and stroke. In addition to “people,” the University lists the NIH (without any specific citations) and the discredited WHO report on acupuncture as its sources of evidence. Oddly, if the NIH really supports these claims, no one told the NIH’s own National Center for Complementary and Integrative Health.
In fact, unsupported claims like those found on both Acufinder’s and the University of Miami’s websites appear to be more the norm than the exception. And herein lies the danger of Legislative Alchemy: States like Illinois give fantasy-based practitioners a broad scope of practice, allowing them to diagnose and treat both fake and very real diseases. Even presumably reliable sources, like medical schools, promote unproven (or disproven) uses, leaving the public with the false impression that acupuncture is effective for any number of conditions. (You can find another example here, from the University of California at San Francisco.)
A similar fate may await the citizens of Michigan, where a substantial practice expansion bill introduced in 2017 remains pending. Acupuncturists there are currently limited to needle acupuncture. In addition to giving acupuncturists licensed health care professional status, the bill would, like Illinois, give them the authority to diagnose and treat any disease or condition in patients of any age using “traditional and contemporary East Asian medical theory.” They would be able to use “electroacupuncture” (i.e., TENS rebranded as acupuncture), “dermal friction” (gua sha), cupping, herbal remedies, and homeopathy (which is German in origin, not East Asian). Acupuncturists could also supervise NADA-trained practitioners treating substance abuse.

New Mexico, as noted, already defines acupuncturists as “primary care” practitioners and permits them to perform and order diagnostic testing, as well as practice bleeding. The state Board of Acupuncture and Oriental Medicine can issue certificates expanding their practice to include the authority to compound drugs on their formulary, such as bioidentical hormones, and deliver these products by IV, as well as prescribing and administering live cell products, among others.
Fortunately, the New Mexico legislature refused to go further last year and allow the Board to issue certificates to practice “holistic integrative medicine” and add to the acupuncturists’ formulary “substances used for detoxification and chelation.” A bill permitting all that and more failed.
Mississippi and Nebraska used to require a physician referral for acupuncture treatment. Acupuncturists tried to dilute these patient protections in both states and succeeded, although Mississippi turned around and added even more limitations on their practice in the final bill. While the Mississippi legislature repealed the referral requirement, patients must, with very limited exceptions, have a physician evaluation within the last six months for the condition the acupuncturist will treat, and the acupuncturist must inform patients that acupuncture is not a substitute for medical care. Referral to a physician is required if the patient’s condition doesn’t improve and acupuncturists are prohibited from diagnosing.
Nebraska removed the referral requirement as well, but added that the acupuncturist must refer the patient to an “appropriate practitioner” if the condition is beyond his training, competence or experience. These limitations, as noted above, may not exist in the mind of the typical acupuncturist.
As if state budgets weren’t strained enough, pending companion House and Senate bills in Minnesota appropriate $375,000 of the public’s money to do what is essentially worthless “study” amounting to no more than a collection of anecdotes which will supposedly determine the effectiveness of acupuncture for pain and its potential to reduce opioid abuse. Why a much cheaper literature search on PubMed could not meet this goal is not explained, although the bills are perhaps a testament to the scientific illiteracy of the legislators who support it.
Finally, the turf wars: Physical therapists (PTs) and acupuncturists are fighting over a practice called “dry needling.” According to physical therapists, dry needling:
uses a thin filiform needle to penetrate the skin and stimulate underlying myofascial trigger points, muscular, and connective tissues for the management of neuromusculoskeletal pain and movement impairments.
It is based on, according to PTs, “western neuroanatomy and modern scientific study of the musculoskeletal and nervous system” and not on the mumbo jumbo of blocked “qi” and “meridians.” Just because the technique is similar to needle acupuncture, the American Physical Therapy Association points out, does not mean it constitutes the practice of acupuncture. Acupuncturists say it is just that and are trying to lock PTs out of using dry needling.
In addition to their huge practice expansion in Illinois, acupuncturists there convinced the legislature to define dry needling as “acupuncture,” thereby preventing PTs from performing it (unless they go to the trouble of getting a license to practice acupuncture). A similar bill defining dry needling as the practice of acupuncture remains pending in Massachusetts.
You can follow pending acupuncture/Oriental medicine/East Asian medicine/Traditional Chinese medicine (as well as chiropractic and naturopathic) bills on the Society for Science-Based Medicine website and find out how to contact your state legislators about them. Bills introduced in 2018 will be added to the SfSBM website soon.
