The Department of Clinical Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, published a preprint on COVID vaccination-associated myocarditis recently, whose core strength is its prospective cohort design, one of the only potential analyses of asymptomatic (subclinical) COVID vaccination myocarditis, and close follow-up with vaccination dose #2. While it is a strong effort from a team who had very little time to compile the project, there are multiple actors distorting the cardiac evaluation that was done, which demands immediate discussion from a board-certified pediatric cardiologist – like me.
Methods
COVID vaccination myocarditis, while not being completely solved from a mechanistic standpoint, is a well-known disease process now, mostly associated with the mRNA subtype of COVID vaccinations. The age groups most at risk are older boys and young adult men. The time period of highest risk is after the 2nd dose, hence the effort by many national health agencies like the Canadian NACI, US CDC and British NHS to find ways to raise awareness and decrease the risk of vaccine-associated myocarditis. Hypothesized mechanisms generally fall within the realm of transient autoimmune reactions, such as molecular mimicry, a reaction against the lipid nanoparticle, vesicle trafficking resulting in an immune reaction against distant targets, and potential dendritic cell activity. The goal of the present study was to characterize the incidence of symptomatic and asymptomatic myocarditis in a group of students after they received the 2nd dose of COVID vaccination (this dose was chosen because it is previously known to be the period of highest risk).
The authors of the preprint were able to analyze 301 students ranging from 13-18 years of age, of which two-thirds were boys. They tried to record baseline characteristics of these children including ECG, past medical history, echocardiogram, and physical examination. The team then tried to repeat that assessment at least two points although not all the data at each of these points was displayed in the preprint version of paper.
Results
Of the data displayed to the reader, they indicate that some of the kids met criteria for myocarditis, evidenced by EKG changes, troponin detectable in the blood, and some had cardiac MRI findings consistent with myocarditis. They also report a rate of subclinical myocarditis and a rate of abnormal EKG findings amongst their 301 students. While the MRI findings are rigorous and clearly support the diagnosis of myocarditis in those patients in which it was done, the remainder of the patients EKG findings deserve detailed discussion because characters who wish to maximize fear surrounding myocarditis are hyping the EKG findings with a lack of medical knowledge in regards to their clinical significance. The crowd who believes COVID vaccinations in kids is not necessary is saying that abnormal EKGs by themselves are sufficient to diagnose subclinical myocarditis, which is incorrect. At the most basic level of research analysis, the least one can do is compare EKG findings before and after. While the preprint claims they did this, the EKG findings pre vaccination are not available to the reader. It is difficult to compare the cited rates given in this article with the rates used in the prior population studies due to their different statistical methods, but I wish to strongly emphasize, that articles portraying a high rate of myocarditis are not deserving of hype on that reason alone. I can only hypothesize why the timing of the troponin elevation is only after several days, but this may be due to the amount of time required to generate the immune response. The timings of troponin elevation discussed also mirror what has been discovered in prior projects on vaccination myocarditis. Troponins are a useful test to help confirm myocarditis, but I emphasize that troponin in the bloodstream is not diagnostic of myocarditis by itself – it is a cardiologist’s role is to sort out all the other causes of troponin in the bloodstream such as physical exercise.
The EKG findings discussed in the paper are listed below:
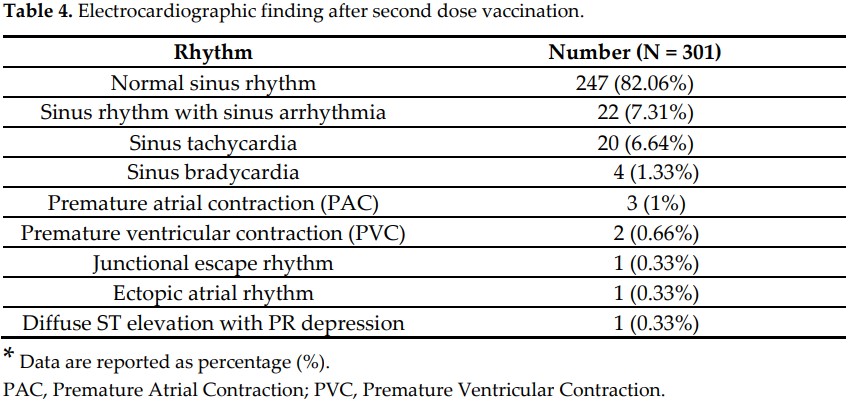
Bad actors may say that 18% of the EKGs were abnormal, but this number is derived from simple subtraction without acknowledging which of these EKG findings are normal variants. They are trying to use these findings to convince people that all the EKG findings demonstrated are abnormal, which, as any medical student or trainee physician should know, is patently false. Some people will use the argument at this point that “no science is settled”, but this knowledge is one of the foundations of general pediatric cardiology. These fundamental EKGs have extremely precise definitions that have no room for debate. I will refrain from using technical terminology as much as possible in the next paragraph, where I will define these different EKG results and what they mean.
- Normal sinus rhythm: EKGs are a two-dimensional representation of a 3-dimensional phenomenon – the electrical wave washing over the heart, stimulating muscular contraction. If you could visualize this wave, it would look something like waves on a beach that repeat on a regular basis. This is what the expression “normal sinus rhythm” means in pediatrics; the electricity is washing over the heart from top right to bottom left in an orderly fashion. The lines on the EKG represent the height of the waves, like if you were placing a meter stick in the water.
- Sinus arrhythmia: I admit that we cardiologists could have named this better, but this means that the EKG rhythm is varying with the patient’s respiratory rate. This is most visible in toddlers, and its effects gradually disappear with age. Bad actors are trying to claim this is abnormal, but in pediatrics sinus arrhythmia is an absolutely normal finding. Even medical students learn this. Antivaxxers claiming that this is abnormal is akin to saying freckles are a medical disease (they are not).
- Sinus tachycardia: While this is a sensitive indicator of myocarditis (meaning even low level myocarditis can cause sinus tachycardia), the EKG result just means that the heart rate is faster than average for the child’s age. This EKG finding can be legitimately claimed as abnormal only if a comparison of pre-vaccination EKGs can be made.
- Sinus bradycardia: This just means that the heart rate is somewhat slower than average for the child’s age. In the vast majority of circumstances, this EKG finding is also a normal variant in pediatrics. This EKG finding can only be legitimately claimed as abnormal if a pre-vaccination comparison can be made.
- Premature atrial or ventricular contractions: These represent extra beats from the top two or bottom two chambers of the heart. Many children are found to have these incidentally; while they can be generated by myocarditis, the presence of a tiny amount of these beats is not worrisome. We start to worry when their quantity is increasing, they disturb heart function, they are triggered by exercise, or they are present in a sustained manner. While it is easier to make the argument that this EKG finding is abnormal, it again must be compared with a pre-vaccination EKG (and preferably a 24 hour EKG monitor).
- Junctional escape rhythm: This rhythm means that the top chambers are perceived, by the rest of the heart, to be slower than what is necessary for a normal heartbeat. As a consequence, the bottom chambers make their own beats to catch up. This is very, very frequent in kids who are physically fit, and especially so at rest. In the absence of blood pressure and heart function derangement, this EKG finding is normal.
- Ectopic atrial rhythm: This means that rather than starting in the top right of the right atrium, the heartbeat starts in a slightly different place. As a sole finding in a child, this is an absolutely normal EKG.
- Diffuse ST elevation: This is the only EKG in the collection of EKG findings that is abnormal at all times; it may suggest irritation of the membrane covering the heart (pericarditis).
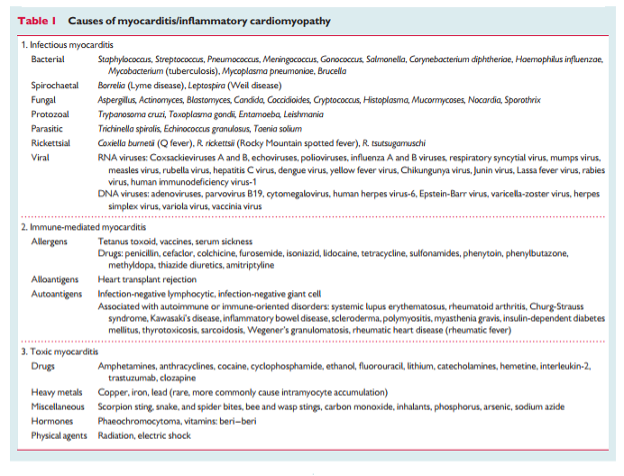
I repeat – the discovery of one of the EKG findings above is not sufficient to diagnose myocarditis. At minimum, the reader should be allowed to compare the EKG findings pre-vaccination versus post-vaccination. I include this table again to remind the reader that myocarditis has many causes:
An elevated troponin has its own causes as well, not all of which are myocarditis:
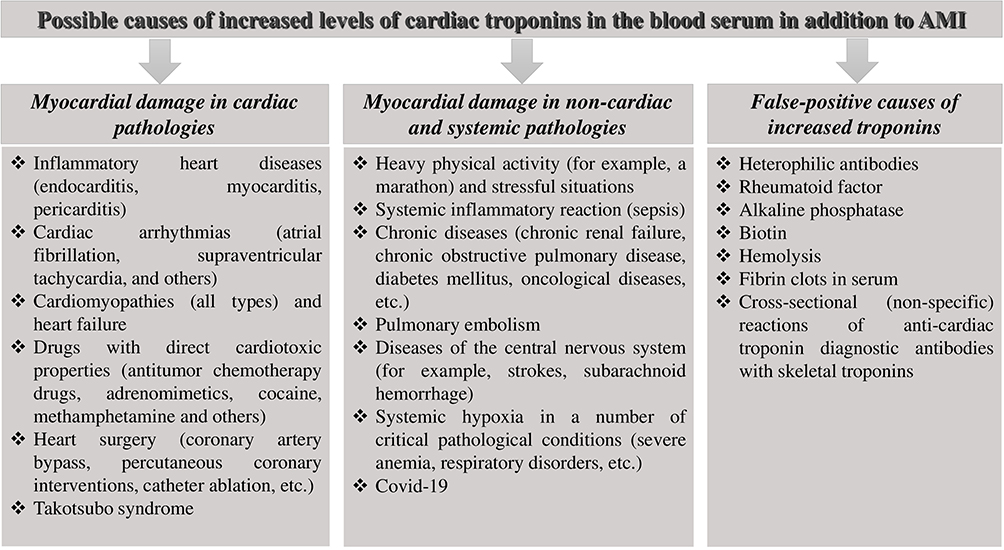
From Chauin 2021
On subclinical myocarditis
The definition of subclinical myocarditis is a patient with lab, imaging, or EKG findings consistent with myocarditis, but minimal or no symptoms (minimal chest pain, shortness of breath, or palpitations for example). The crowd that is most anti-COVID vaccination is very supportive of the finding of subclinical myocarditis in this article without considering its limitations. Cardiologists have formalized the criteria for myocarditis to avoid diagnosing every person with troponin in the blood with myocarditis. This would be misdiagnosis and, unnecessarily frighten the patient. I particularly emphasize – even if it is coming from me – a speaker who analyzes articles critically when they do not fit the speakers preconceived notions, and fails to analyze critically when the articles do match their preconceived notions, is presenting you with a biased and possibly deceptive assessment of the world. Many kinds of disinformation would not have an audience, if the public knew when a science communicator was presenting only one side of an issue. People opposing COVID-19 vaccinations especially do not consider the behavior of subclinical myocarditis – which has been researched:
- In this study from Turkey, people who had rheumatic fever-associated myocarditis did not land in the hospital due to that diagnosis (although they needed monitoring).
- In this study, some athletes were found to have subclinical myocarditis after contracting COVID.
This point is especially important – people who wish to instill fear about vaccination myocarditis rarely stays consistent, and usually do not compare discussion of vaccine myocarditis with the rates of subclinical myocarditis due to viral infections. The outcomes of mild and subclinical myocarditis are generally very good. Regarding the preprint – we need, at the very least, to understand the significance of the authors’ diagnoses of subclinical myocarditis, and a full disclosure of the children’s cardiac testing prior to vaccination (and preferably at all stated data collection time points). This is a modification to their project that can be done during the peer review process.
Conclusions
This research team made a strong effort to try and design a prospective clinical case series/ small clinical trial to see what happens to kids who get the mRNA COVID-19 vaccine. It does have its limitations but it was what they could come up with on short notice. A study on COVID vaccination myocarditis is not worthy of hype only because it reports the highest rate of myocarditis yet observed. We have strict myocarditis criteria to make sure healthcare workers who diagnose myocarditis systematically go through all the causes of elevated troponins that are not due to myocarditis.
The takeaway points are:
- In the end, to the trained observer, there are no shocking findings in this study. Overall, it supports the current body of knowledge regarding COVID vaccination myocarditis.
- The prevalence of subclinical myocarditis after COVID vaccination is not discernable based upon the project as currently presented; while preprints are a great way to get studies out quickly, they should not be used to inform policy before being peer reviewed by other healthcare professionals trained in the subject matter. It will be good to see what an updated rate of subclinical myocarditis is after peer review and editing, preferably with refinement of diagnostic criteria to match the international Brighton collaboration criteria and and myocarditis formal case definition criteria
- Based upon data available so far, people who have recovered from vaccination myocarditis have minimal to no symptoms, although they should have long term follow-up.
- While some patients with myocarditis carry some subclinical ongoing findings by MRI, one disease process does not automatically apply to a different disease process (for example certain diseases of the heart that carry gadolinium enhancement can heal to the point that some of the enhancement resolves).
- If you are concerned about subclinical myocarditis, all you need to do is discuss doing the testing with your physician.
Also, pediatric cardiologists are currently collaborating with national health agencies to continue study of pediatric postvaccine myocarditis and determine what the clinical outcomes are.
Ways you can decrease your risk of vaccine-associated myocarditis include:
- Space out your doses at 8 weeks or longer.
- If you are a teen boy or young adult male, pick Pfizer over Moderna.
- It is plausible that Novavax may produce less myocarditis but the real-life behavior of this vaccination in post-EUA surveillance has yet to be adequately studied, since it was only recently granted United States FDA Emergency Use Authorization.
- if you don’t want to have anything to do with mRNA vaccinations, nobody can twist your arm (really, pediatricians aren’t looking to twist anyone’s arms). All you have to do is not vaccinate, hopefully while understanding the risks of COVID-19 in unvaccinated populations.