
Hydropsfetalis – the consequences of untreated hemolytic disease of the newborn
I have encountered a great deal of harmful nonsense over the years. Vaccine and vitamin K refusal, vaginal seeding, placentophagy, and waterbirth are all topics I’ve covered in the past on SBM, and all are recommended by so-called experts in natural or holistic health. So when I was alerted to recommendations by a popular pseudoexpert to avoid yet another safe and effective means of preventing the suffering of children, I wasn’t surprised. Angry, yes. Frustrated, definitely. But not surprised at all. Sigh.
A follower on Twitter recently shared a link to an article written by Sarah Pope, a Weston-Price Foundation board member with training in economics and financial management who refers to herself as “the healthy home economist.” Pope, who has in the past recommended that parents avoid all vaccines, preferring homeoprophylaxis and immune boosting diets, refuse the newborn vitamin K shot, and lie to their pediatricians about giving babies raw milk, has come out against a safe medical therapy that has saved countless lives: anti-D immunoglobulin for the prevention of hemolytic disease of the fetus and newborn, caused by a mismatch in mother-fetal blood type. As expected, her article is dense with factual errors and anti-medicine propaganda.
Before I tackle Pope’s article, which is 97% fearmongering and links to whale.to, I’ll provide a brief primer on anti-D immunoglobulin and the disease it prevents. This is a complex topic that I plan on doing a reasonable, if not deep, dive into. As with most aspects of science-based medical care, there is nuance and we don’t have all the answers. But I’ll do my best.
How is blood type determined and what are the clinical implications?
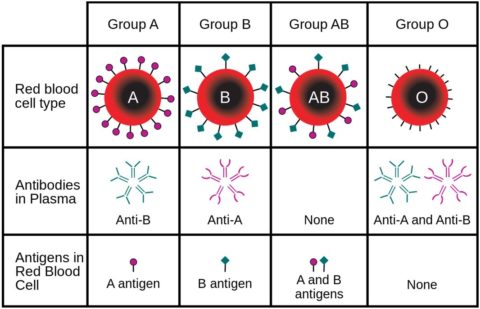
The relationship between blood type, blood antigens, and red blood cells.
Human blood type is identified using the presence or absence of major blood group antigens on our red blood cell membranes, specifically A, B, and Rhesus, which is commonly referred to as simply Rh. The most clinically important Rhesus antigen, and the one designated by the + or – in your blood type, is D. There are actually a total of 48 antigens in the Rhesus system, but most of them, as well as the over 300 different minor blood group antigens, are much less frequently expressed and often not particularly immunogenic. There are exceptions that are beyond the scope of this post.
When a patient is A+, for example, her red blood cells express A antigen and D antigen. An O- patient, on the other hand, does not express any A, B, or D antigen and thus her immune system would not recognize them as having been produced by her own body. Our immune system, shaped by at least a few thousand years of evolution, has a tendency to make note of such foreign antigens when first encountered by producing immunoglobulins. Perhaps more commonly known as antibodies, these specialized proteins are tailored to recognize specific invading antigens quickly and to initiate a more robust response with each subsequent exposure. It’s a process that helps to keep us healthy and free from disease, but these antibodies are problematic in certain situations, such as when the foreign protein might be useful or isn’t actually foreign.
One example of the former is when a patient requires a blood transfusion. Haphazardly giving improperly matched blood can result in a fatal transfusion reaction, which is why O- blood, the so-called “universal donor”, is so useful in emergencies. In reality, it is possible for even O- blood to result in a reaction when non-D Rhesus or minor blood group antigens are present and the recipient has been previously sensitized. So when blood is needed less urgently, additional screening for the presence of unexpected antibodies is performed, and typically a crossmatch between the patient’s blood and potential donor blood is performed in order to completely avoid the risk of a transfusion reaction.
As I mentioned above, there is the potential for an immune response (sensitization) to several blood group antigens other than A, B, or D. These may or may not result in clinically important reactions, or in disease in a fetus or newborn. Plus they are significantly less commonly expressed. In this post, I’m going to focus on the Rh(D) antigen and maternal production of anti-D antibody because it is what Pope discusses in her article. It is also the only scenario where we have an effective strategy for preventing disease in the baby.
What is hemolytic disease of the fetus and newborn?
All pregnant women undergo blood typing and screening for the presence of antibodies against major and minor blood group antigens at the first visit, again at 28 weeks, and finally at delivery. The first two are geared towards assessing risk to the baby and the check at delivery is in case the mother has a complication and requires a blood transfusion. When a mother is Rh-negative, meaning that the D blood group antigen is not expressed on the outer membrane of her red blood cells, she has the potential of bearing a child affected by hemolytic disease of the fetus and newborn (HDFN).
HDFN can only occur once an Rh-negative mother has become sensitized to D antigen. This typically happens during a previous pregnancy when fetal Rh-positive blood has crossed the placenta and entered into the maternal circulation. This is referred to as fetomaternal hemorrhage and it likely happens in most if not all pregnancies to some degree. Unfortunately it doesn’t take much mixing of blood to sensitize a mother, and the risk increases with each exposure during a pregnancy and with larger amounts of fetal blood. Sensitization to D antigen used to happen to thousands of women every year. Now, not so much.
Exposure through fetomaternal hemorrhage occurs most commonly during delivery, but it can take place earlier in pregnancy in the event of miscarriage, abdominal trauma, or invasive intrauterine procedures, to name just a few. Or, because the universe doesn’t care about us, for no clear reason whatsoever. Historically this happened in roughly 15% of Rh-negative mothers after two deliveries of Rh-positive babies. Sensitization can rarely occur through other means of exposure, such as an improperly matched blood transfusion of Rh-positive blood or a contaminated needle.
When sensitization occurs, anti-D antibodies that are produced are of the IgM class. They can’t cross the placenta, so the current occupant of mother’s uterus is safe. Over time, the immune system begins to produce IgG class anti-D that can cross the placenta. So it is the next baby, provided that they are also Rh-positive, that can develop HDFN when some of their blood enters the maternal bloodstream and elicits a more intense immune response. With each additional pregnancy, and each additional exposure to D antigen, the immune response can be increasingly robust and result in more severe disease.
IgG antibodies are supposed to cross the placenta for very good reason. In yet another evolutionary scheme to keep enough of us alive just long enough to reproduce, these antibodies can help protect newborn humans from a variety of infectious organisms during a vulnerable transition period. But when maternal anti-D IgG antibody crosses the placenta, it attaches to Rh-positive fetal blood and marks it for destruction by the child’s own spleen. This can result in severe anemia requiring intrauterine blood transfusions, hydrops fetalis, and jaundice requiring exchange transfusion to prevent permanent injury to the brain.
What is anti-D immunoglobulin?
As I explained above, anti-D immunoglobulin (aka antibody) is produced when an Rh-negative human is exposed to Rh-positive blood. Also as stated above, if the human in question is a sensitized pregnant woman, the transition from IgM to IgG anti-D antibodies over time will result in their ability to cross the placenta and harm the fetus/newborn. Wouldn’t it be great if we could somehow prevent or at least significantly reduce the likelihood of this chain of events ever taking place?
Well, we can. Since the 1960s, we have been successfully preventing maternal sensitization to D antigen during pregnancy by giving strategic doses of the very thing we don’t want mom to produce on her own: anti-D antibodies. How this works isn’t quite clear, but the leading hypothesis is that the exogenous antibodies lead to rapid clearance of any fetal red blood cells in the maternal circulation. If timed right, the mother theoretically doesn’t have time to become sensitized.
As I mentioned earlier, antibody screening of pregnant women is recommended at the first visit. If an Rh-negative mother is already producing her own anti-D, focus then shifts to the recognition and management of HDFN in the fetus and newborn. Anti-D treatment of the mother will do nothing to prevent disease in that case.
In non-sensitized pregnant Rh-negative women, the combined strategy of giving a dose of anti-D immunoglobulin at 28 weeks of gestation and after any high risk antenatal events, and then giving a dose after delivery if the child is Rh-positive, has dramatically reduced the incidence of sensitization. Without sensitization, there can be no HDFN. Unsurprisingly, the condition has gone from common to rare in the United States and other developed regions, but sadly is still a common cause of morbidity and mortality in the rest of the world.
Anti-D for use in pregnant women used to be collected from sensitized women. It quickly became so rare for a woman in the US to be sensitized that we have to purposefully sensitize male donors. It is increasingly difficult to keep up with demand, however, so scientists are working on means of producing anti-D synthetically, which would do away with supply issues and the small but real risk from using a blood product. Studies are already underway so stay tuned.
The (Un)healthy Home Economist swings and misses…a lot
The article by Sarah Pope is bad. It’s real bad. She tells pregnant Rh-negative women to avoid anti-D dosing during pregnancy. She even tells them it’s okay to skip it after delivery of an Rh-positive baby, which is when it is most effective. But don’t take my word for it, read the article for yourself. I will provide a few of the most blatantly ignorant claims along with some commentary.
Pope starts off with a rather misleading, likely intentionally so, comparison:
The Rhogam shot is an injected vaccination given to all pregnant women with Rh negative blood. Rhogam works very much like an immunization. It puts a small amount of Rh antibody into the mother’s blood to effectively fool it into thinking the foreign Rh protein has been eliminated.
Rhogam is the trade name for the most commonly used anti-D immunoglobulin in the United States, but there are several other products available that are used here and in other countries. There are some differences in their manufacture, but no anti-D product is in any way a vaccine. That’s just ridiculous.
A vaccine stimulates the production of antibodies in the recipient in order to protect against an infectious disease should exposure occur. Anti-D dosing involves the transient employment of exogenous antibodies against a red blood cell membrane antigen to prevent maternal development of those antibodies herself. Pope is rabidly anti-vaccine, so I can’t help but consider that this comparison is an ad hominem done in an attempt to establish guilt by association.
She continues…
This small risk arises if there is any mixing of blood between the mother and the fetus. Under normal circumstances, this never occurs, but in the event of a car accident or trauma to the mother’s belly, some mixing of blood is possible. Mixing may also occur if there is a miscarriage, amniocentesis, chorionic villus sampling (CVS), or birth interventions during the labor/birth process.
Or for no clear reason. And it isn’t a small risk. Many thousands of women became sensitized every year and thousands of babies suffered and died prior to the development of anti-D dosing to prevent it. I wonder how many dead babies it would take to meet Pope’s threshold for concern.
More nonsense:
The Rhogam shot does work, but only if the immunoglobulin is administered within 72 hours of the trauma that caused the blood mixing in the first place. What also makes no sense is that doctors recommend that all Rh negative women get RhoGam during pregnancy even if the father is also Rh negative! There is absolutely no need for Rh negative women with Rh negative partners to ever get RhoGam as the baby will always also be Rh negative and the risk from Rh antibodies is zero!
Wrong again. While true that anti-D dosing is most effective if given within 72 hours of a high risk event, such as trauma or delivery, it still reduces the risk for weeks after dosing during an otherwise uneventful pregnancy. Postnatal dosing is definitely the more important intervention, reducing risk of sensitization from 13-16% to 1-2%, but the addition of antenatal dosing at 28 weeks lowers it to .1-.3%. Also, it is incredibly naive of Pope to assume that the partner is always the father of the baby. Paternal nonparentage happens more than many might want to admit.
Pope then contradicts herself:
The Rh antibodies from the RhoGam shot hang around in the mother’s bloodstream for up to 12 weeks following the shot. As a result, if blood mixing occurs during that period of time (as in a car wreck or other trauma), it is possible for some of the Rhogam antibodies to find their way into the fetus’ bloodstream and attack them causing the very Rh Disease in the fetus that the shot is supposed to prevent!
So which is it? Is the 28 week antenatal shot ineffective because it has to be given within 72 hours or do the antibodies stick around for weeks and potentially harm the baby? In reality, they stick around for weeks, potentially removing fetal red blood cells from maternal circulation, and never harm the baby. The amount that might cross the placenta is just too small. Rarely testing of a newborn’s blood will reveal evidence of anti-D antibody but there is no evidence that this has ever resulted in clinically meaningful anemia or jaundice.
More fearmongering:
There is also the possibility of side effects from the RhoGam shot. Swelling, inflammation, hives and even anaphylactic shock are not out of the question. More concerning is that the Rh antibodies have the potential to negatively affect the immune response of either the mother or baby to other foreign substances that enter the bloodstream.
No evidence exists to support the claim that anti-D administration negatively affects the immune response of baby or mother. And risk of severe adverse events is incredibly low. One study found 11 reports of possible adverse events out of 2.9 million doses.
Anti-D is pooled antibody collected from many different donors, typically sensitized Rh-negative men who have been “encouraged” to produce antibody by repeated injection of small amounts of D antigen. So it could potentially contain IgA antibodies and other immunogenic plasma proteins. This matters because a fair amount of healthy people don’t produce their own IgA, which means that antibodies against IgA can develop and put them at risk of severe allergic reaction if exposed via blood transfusion or injection of intravenous blood products.
So the potential of an allergic reaction, even a serious one, is plausible. Even after processing, some anti-D products may still contain trace amounts of IgA and must be given via intramuscular injection to avoid this risk. RhoGAM is one, which is why pregnant women in the United States typically get a shot. Others, which are more expensive, are processed in such a way as to remove even the trace amounts and can be given via IV. Bottom line, a severe allergic reaction is extremely unlikely to occur.
Pope also mentions the risk of acquiring a viral infection from administration of anti-D. As I just mentioned, it is a blood product so this isn’t an unreasonable concern. Donated plasma is tested for the potential presence of hepatitis C, hepatitis B, HIV, and parvovirus B19, but no test is perfect. Additional steps are taken, however, such as ethanol fractionation followed by viral-clearance ultrafiltration, that greatly reduce the risk even further. The risk is real, but so low that the potential benefit far outweighs it.
Pope heads right back into the weeds:
Studies performed by Health Advocacy in the Public Interest (HAPI) in 2004 found that despite vaccine manufacturers’ claims that thimerosal was no longer being used…All vaccine vials tested by HAPI that were labeled “mercury free” did, in fact, contain this neurotoxin. All the vials also contained aluminum which enhances the toxicity of the mercury causing rapid death of brain neurons.
In 2001, the FDA mandated that thimerosal be removed from anti-D products. There was no evidence that this mercury preservative caused any harm, but there was significant public concern based largely on anti-vaccine propaganda that I’ve no doubt you are quite familiar with. The “studies” mentioned in the above Pope quote are really one study, which was funded by an anti-vaccine advocacy group run by Dawn Winkler. For $500, she sent 4 samples of anti-D to Doctor’s Data, a lab known for telling quacks and cranks exactly what they want to hear.
Pope goes on to play the shill card, of course, claiming that anti-D dosing during pregnancy lines the pockets of Big Pharma. She also claims that anti-D is never given during pregnancy in Europe, only after delivery. This is blatantly false, as antenatal anti-D is absolutely given in Europe, although it is given less often.
Some European countries rely on cfDNA blood typing and give anti-D during pregnancy only when the fetus is found to be Rh-positive. It’s a pretty accurate test if performed after 11 weeks, but not perfect and ACOG doesn’t recommend using it for this purpose. My hunch is that they will eventually as the cost comes down. This approach would reduce the need for antenatal anti-D dosing by about 30% but there would likely be a few cases of sensitization every year that would have been prevented with universal dosing.
Pope concludes her article by rehashing her previous false claims and scare tactics. She restates that mothers absolutely do not need anti-D dosing at all if the father is Rh-negative, which is dangerously naïve. She again claims that it endangers the life and health of the child. She says doctors are “WRONG.”
Pope once more writes that antenatal dosing is arbitrary and useless unless an at-risk mother is in a car accident. She implies that the risk of anti-D dosing after delivery might be greater than the benefit even when the baby is known to be Rh-positive, especially if the birth was “natural.” She finishes by giving nutritional recommendations to help “tone the uterus” and prevent mixing of blood, and somehow even manages to blame fluoride.
All of this is wrong.
Conclusion: Following advice from The (Un)healthy Home Economist puts your baby at risk
Hemolytic disease of the fetus and newborn is a potentially deadly, but nearly completely preventable, complication of an otherwise normal and healthy pregnancy. It is a great example of how evolution doesn’t have to be perfect, just good enough, because nature doesn’t care about a few thousand dead babies as long as the species survives. The development of a safe and effective means of preventing HDFN is one of the most incredible examples of the benefit of applying science to the practice of medicine.

