This post will provide a bit more detail on vaginal seeding and the potential risks and benefits. I will also discuss how more recent data is calling the practice further into question.
Why vaginally seed your baby?
The process of vaginally seeding newborns was largely the brainchild of Dr. Maria Dominguez-Bello, an Associate Professor at the NYU School of Medicine who specializes in research on vertebrate microbiota. She has published numerous studies specifically looking at the human microbiome, including that of the newborn. The impetus for vaginal seeding was found in her 2010 paper, “Delivery Mode Shapes the Acquisition and Structure of the Initial Microbiota Across Multiple Body Habitats in Newborns.”
In this paper, the microbiota of four vaginally-delivered infants were compared to six born via C-section. They also compared the infant findings to that of their mothers. The authors concluded that “vaginally delivered infants acquired bacterial communities resembling their own mother’s vaginal microbiota, dominated by Lactobacillus, Prevotella, or Sneathia spp., and C-section infants harbored bacterial communities similar to those found on the skin surface, dominated by Staphyococcus, Cornybacterium, and Propionibacterium spp.”
This finding was quickly assimilated into our existing knowledge of long term health differences between vaginally delivered infants and those born via C-section. Research has found small but significant increases in rates of obesity, asthma, and autoimmune conditions associated with C-section birth, though there remains the issue of correlation versus causation. There is also interesting research linking alterations in the human microbiome with various pathologies, and there is legitimate plausibility to the concept of microbiome manipulation as a means of improving human health.
So it isn’t unreasonable to propose that altering the microbiome of the human newborn may have health benefits. Dr. Dominguez-Bello has even published a more recent pilot study looking at the effects of vaginal seeding on the microbiota of babies born by C-section. But in medicine there is no free lunch. All interventions to my knowledge carry some risk and vaginal seeding is not an exception to this rule.
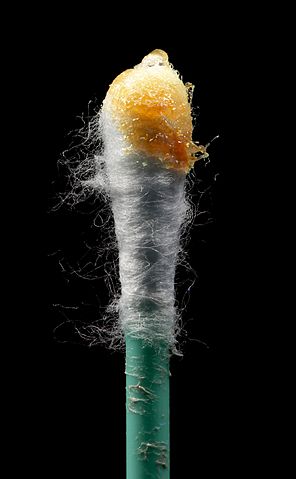
Why you should consider putting down the swab
So what is the potential harm of vaginal seeding? Babies are born vaginally all the time, after all. Don’t we screen mothers for potential pathogens that might harm a newborn?
Well, yes we do. In the United States, we screen mothers for Group B streptococcus (GBS), hepatitis B, Chlamydia, and HIV. Some women are screened for herpes simplex virus (HSV) and gonorrhea. Not all countries follow the same screening guidelines as the United States, however. All of these organisms can be spread to a newborn infant via vaginal secretions, and all can cause significant morbidity and mortality.
GBS is the most common cause of serious bacterial infection in newborns, including pneumonia, bloodstream infections, and meningitis. Hepatitis B infection in a newborn results in liver failure in a majority of cases and frequently is fatal. Chlamydia is one of the most common causes of blindness in children around the world. HSV causes life-threatening systemic infections and meningitis. Gonorrhea isn’t a picnic either, and HIV needs no further explanation of its pathology.
So we do screen for some pathogenic organisms, but no screening process is perfect. Take GBS, for example. Mothers are typically tested at 35-37 weeks gestation and, if positive and delivering via a vaginal delivery or C-section after labor has started and her membranes have ruptured, she is given antibiotics prior to delivery in order to reduce the risk to the baby. But some mothers deliver too quickly for antibiotics to be administered. And some, labeled as GBS unknown, deliver prior to testing, don’t get full prenatal care, or even refuse GBS testing for a variety of ill-conceived reasons.
So, you might ask, why not consider vaginal seeding when the mother is known to be GBS negative but proscribe it when she is positive or unknown? It’s actually a good question and similar to one that I get from medical students frequently: “Why worry about GBS infection at all when a mother is GBS negative and a newborn is showing early signs of an infection?”
The reason that being GBS negative shouldn’t change clinical management in these situations is that many women who are negative when tested may be positive by the time that they deliver. And GBS isn’t the only bacteria in vaginal fluid that puts an infant at risk. With the decline in GBS infections related to antibiotic prophylaxis, we have seen an increase in the rates of serious neonatal infections with E. coli.
All of the potential pathogens listed above can be found in the vaginal fluid of asymptomatic women and missed because of imperfections in the screening process or a lack of screening altogether. They can all potentially be spread to a newborn via seeding maneuvers. Admittedly the risk would likely be low in most situations, but if vaginal seeding becomes more widespread, and if women are encouraged by certain providers to participate in high-risk seeding, we will see babies harmed by the practice.
Do the benefits of vaginal seeding outweigh the risks?
In medicine, there is a constant requirement to weigh both the risks and benefits of an intervention. There are many treatments, such as a bone marrow transplant, that carry extreme risk, even of death, but offer a cure in the face of a uniformly fatal condition. Some treatments fall decidedly on the opposite end of the risk-benefit spectrum, providing little or no benefit whatsoever and significant risk. Vaginal seeding must be evaluated no differently than any other intervention.
As it stands, there is currently only the speculation of benefit from vaginal seeding. First off, there is no evidence to date that possible differences in the microbiota of newborns is a causal factor in the small increased risk of some conditions seen in babies born by C-section. And the studies being used to support these microbiota differences are only a portion of what is a fairly inconclusive literature. There is recent evidence calling into question that the mode of delivery plays an important role at all, with some researchers claiming that the maternal condition leading to a C-section is more important.
The initial paper from 2010 which showed differences in microbiota between vaginally and C-section delivered newborns looked at 10 babies. A January 2017 paper in Nature Medicine looked at 81 and found that any potential differences essentially wash out within a few weeks. This doesn’t mean that the minor differences found prior to 6 weeks aren’t involved in long term health, but proof is still lacking.
Even if there were a proven difference between these populations, we don’t have good evidence that vaginal seeding is a replacement for a vaginal delivery. The pilot study mentioned earlier only looked at 18 infants. Of the 11 born via C-section, only 4 underwent seeding. They did find some overlap between these 4 babies and the 7 vaginally delivered newborns at 30 days of life, and a larger study by the same author is currently enrolling. But it all may just be noise in the background.
Conclusion: To swab or not to swab
I get it. The microbiome is a hot topic right now. As with epigenetics, people are jumping on the bandwagon left and right and enthusiasm is outpacing the evidence. It may pan out, and there is certainly a plausible connection between the microbiome and our health, but it is far too premature to be promoting novel interventions in newborns. Currently the very real possibility of harm should be a rate-limiting factor in the implementation of vaginal seeding, at least until we have more data.
Here is the ACOG comment on vaginal seeding. The AAP has yet to comment. And here is a comment from a “holistic psychiatrist’s” website discussing vaginal seeding:
Some animals purposefully bring their newborns into contact with the mother’s feces. Animals do not go to the university and do not give birth in a hospital…
They simply use their innate wisdom! We all but forgot about Nature (not the magazine!).
Have a great weekend.