The sale of dietary supplements is booming and continues to grow. Supplements are enormously popular with an estimated 75% of Americans using some form of supplement regularly. Supplements are widely believed (and advertised) to provide meaningful health benefits. As cardiovascular disease is the leading cause of death in the US, it is not surprising that supplements purported to treat, mitigate, or prevent cardiovascular disease would be popular. It has been noted in many posts on this blog that the supplement industry is very lightly regulated, meaning that claims of effectiveness may not be backed by credible evidence. Additionally, safety concerns have been raised with some supplements, with the suspicion that in some cases, they may harm more than help. With this question in mind, Safi Khan and colleagues from West Virginia University and other organizations undertook a massive umbrella review (a summary of systematic reviews) of dietary supplements and their effects on cardiovascular outcomes. The paper was published in the Annals of Internal Medicine in July 2019, and is entitled “Effects of Supplements and Dietary Interventions on Cardiovascular Outcomes“.
What did we know about supplements?
Before we get into the analysis, some background and context is helpful. There is a lot of interest in understanding if dietary supplements benefit cardiovascular health, and there have been several large trials designed to answer this question. The evidence overall is not compelling. A 2013 United States Preventive Services Task Force systematic review found little support for vitamin and mineral supplements. A meta-analysis of RCTs through 2017 found some stroke benefit from folate (folic acid) but no cardiovascular benefits from multivitamins, vitamin C, vitamin D, or calcium. Interestingly the analysis found evidence of harm for niacin and antioxidants. Other trials have looked at fish oils and vitamin D, with generally unimpressive results, with the exception of the REDUCE-IT trial which did find a clinical benefit with a prescription-only form of an omega-3 acid.
What did the authors do?
The methodology of the approach was as follows: The authors searched health databases for relevant English-language papers using appropriate key words. They included any meta-analyses or randomized controlled trials assessing efficacy of supplements or dietary interventions in adults that reported estimates of all-cause mortality and cardiovascular outcomes. These secondary outcomes were cardiovascular mortality, heart attacks, strokes, and coronary heart disease. Studies that looked at “surrogate” or other endpoints (surrogate endpoints are endpoints that patients don’t care about until their health professional tells them it’s important) were excluded. This review was narrowly focused just on these specific endpoints, so even measures like quality-of-life (which is highly relevant to patients) were excluded.
What did the authors find?
With these restrictive criteria the researchers found 942 citations but eventually extracted data on 24 interventions (16 types of supplements and 8 dietary interventions) which formed the data set for the analysis. This included 9 systematic reviews and 4 new RCTs, for a total of 105 meta-analyses, and 277 RCTs, encompassing 992,129 patients. The interventions studied included:
- 16 different supplements: antioxidants, beta-carotene, vitamin B complex, multivitamins, selenium, vitamin A, vitamin B3 (niacin), vitamin B6, vitamin C, vitamin E, vitamin D, calcium plus vitamin D, folic acid, iron, omega-3 fatty acids.
- 8 different dietary interventions: Mediterranean diet and intake of reduced saturated fat, modified dietary fat, reduced dietary fat, reduced salt diets, increased omega-3 alpha-linolenic acid, and increased omegas 6 fatty acids.
Here are some of the key findings, some of which are contrary to other published studies:
- Reduced salt diets in people without high blood pressure (“normotensive”) was found to reduce all-cause mortality with moderate certainty. None of the other 23 supplement or dietary interventions were associated with any demonstrated risk reduction.
- Reduced salt intake in hypertensive individuals was found to reduce cardiovascular mortality, again with moderate certainty. None of the other 20 evaluated dietary interventions or supplements were found to demonstrate any effect on cardiovascular mortality.
- 21 interventions studied myocardial infarctions. Only the use of omega-3 fatty acids was associated with a modest but statistically significant reduced risk of heart attacks.
- 20 interventions studied stroke. Folic acid was associated with lower risk of stroke, while calcium and vitamin D were associated with increased risk. Other interventions had no effect on risk.
- 19 interventions studied coronary heard disease. Only omega-3 fatty acids were associated with a reduced risk of coronary heart disease.
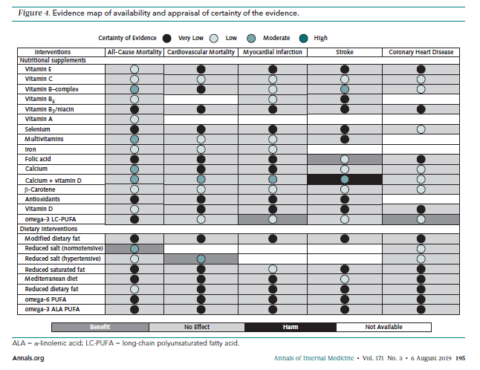
The authors generated an “evidence map” which I will reproduce here summarizing the findings for all interventions. (The paper is open access and you can find it here.) Regrettably the colour choices are poor, but you can see how the authors attempted to map the certainty of the evidence (the circles) with the nature of the effect (the box shading). It is obvious from this representation, that the certainty of the evidence overall is not impressive. None of the interventions are backed by high-quality evidence.
Assessment
This analysis of 24 different dietary supplements and interventions found only modest evidence for a small number of products and approaches. The authors discuss the findings related to sodium and diet, an area of continued debate and controversy. A few observations: It seems implausible that a low sodium diet will decrease all-cause mortality in those without hypertension, but not in those with hypertension, while at the same time hypertensives have reduced cardiovascular mortality.
Findings related to omega-3 long chain polyunsaturated fatty acids are also puzzling, which is regrettable because fish oils are enormously popular. This study found evidence of some benefit with low quality evidence, yet some high quality randomized trials have shown no compelling evidence of effect. This isn’t to say that there may not be something to the ingredients in fish oils, as the REDUCE-IT trial showed a significant effect on cardiovascular outcomes in a specific population with a prescription-only, high-dose purified omega-3 fatty acid.
The authors note that folate’s benefit was driven by a single trial that evaluated its efficacy in China, where fortification is not done. Consequently the beneficial effects may not be relevant in countries like the US, where foods are routinely fortified.
Calcium and vitamin D, however, were associated with harm, including both stroke and heart attacks. This has been shown or hinted at in a few studies, suggesting that routine calcium supplementation in the absence of a medical need is probably not warranted and may in fact be harmful. Vitamin D on its own, however, at least hasn’t been shown to be harmful – but neither has it been shown to reduce the risk of cardiovascular disease.
For multivitamins, singly and overall, the authors restate the USPSTF 2014 statement that there is a lack of evidence to support the benefit of multivitamins to reduce cardiovascular disease or death.
The authors point out some important limitations that need to be considered when looking at the data:
- There was a huge variation in the baseline characteristics of the different groups in the studies, including factors like age, sex, health and socioeconomic status.
- There was a lack of dose-response analysis.
- There was no stratification of these results by demographics or underlying medical disorders.
- The certainty of evidence, overall, was very low.
Conclusion: No strong case for supplements
Reading studies of dietary interventions and supplements can be frustrating. The data is often poor, much of it is observational, and there are so many other variables that might possibly affect efficacy (e.g., product quality, baseline diets, accuracy of dietary recall) that identifying any signal in all this noise is inevitably going to be challenging. Reading this paper which focused on highly selected evidence, you may make one of the following assessments:
- Dietary supplements don’t provide any meaningful benefits.
- Dietary supplements haven’t been studied sufficiently or extensively enough to demonstrate the benefits that you believe exist, despite the lack of any convincing evidence.
- The benefit of any dietary supplement, if it is real at all, is small in the context of all the factors that influence cardiovascular health.
In light of the overall evidence, I’m leaning towards the third assessment. If dietary supplements or specific dietary approaches had substantial effects on cardiovascular disease, we should have seen them consistently in the medical evidence. We do not. Consequently, it’s reasonable to assume that the overall benefit of individual dietary supplements or dietary interventions for cardiovascular disease has not been demonstrated, and that there is no solid evidence to support their use.

