We all construct our narrative based on our biases and spin the facts so that the narrative confirms our biases. Among other characteristics, what separates an SBM provider from a SCAM provider is realizing that biases are always active and apply to me as well as everyone else.
My biases are simple: I am skeptical that humans can reliably understand reality without assistance and the best source of assistance is science.
I have a job where the expectation is that I will change practice as information changes. How I practiced medicine 30 years ago is very different from how I practice it today. Still, I note it is harder and harder to change my approaches as I get older. I get more set in my ways and it takes more effort to change as new studies are published. Sometimes it seems almost physically difficult.
Again, it is expected that not only will I change my mind over time, as the sole ID doctor at my hospitals, I will be the one to lead the change. Imagine how much harder it would be to change your mind if you were committed to a universal truth such as those that are alleged to underlie reiki or chiropractic. Years committed to a pseudo-medicine probably renders changing one’s mind virtually impossible.
I will admit there is one bias I cannot fathom, the conspiracy/pharmaceutical shill world view. The idea that those of us concerned with pseudo-medicine are doing so because we are paid by big pharma is just so weird. There are a number of articles on Pubmed concerning medical conspiracies, but the search term “pharmaceutical shill’ yields nothing on either Google scholar or Pubmed. It is a bias that evidently has no research to help understand why people have that opinion. I suspect it is derived in part from the often-remarkable sums paid to some doctors to pimp medications to other doctors. But I can’t even find how common the belief is.
I can kind of understand why people practice and/or participate in the various SCAMs given my understanding of the various fallacies and dysfunctional ways the mind works. It is easy to see how both the practitioners and patients misjudge the efficacy of pseudo-medicine. We have evolved to survive reality, certainly not to understand it.
Bias leads to spin, and it is curious how bias can warp the reports in the medical literature.
It is a curious fact that acupuncture studies from the East are virtually always positive:
Research conducted in certain countries was uniformly favorable to acupuncture; all trials originating in China, Japan, Hong Kong, and Taiwan were positive, as were 10 out of 11 of those published in Russia/USSR. In studies that examined interventions other than acupuncture, 405 of 1100 abstracts met the inclusion criteria. Of trials published in England, 75% gave the test treatment as superior to control….No trial published in China or Russia/USSR found a test treatment to be ineffective.
I find that fascinating. Is it publications bias i.e. only positive studies are published? Or is it, due to deep cultural bias combined with poor methodology (adequate blinding and placebo), that all studies are indeed positive, a massive example of N-rays in action?
pronounced bias due to lack of patient blinding in complementary/alternative randomized clinical trials
leads to:
nonblinded patients exaggerated the effect size by an average of 0.56 standard deviation
and the effect is more pronounced in acupuncture trials, I suspect it is a combination, especially given a similar results with yoga studies out of India:
Positive conclusions were reached in 277 RCTs (91%); with more positive RCTs being conducted in India than elsewhere (odds ratio=24.8; 95% confidence interval=3.3, 184.5; p<0.001) while type of journal was not associated with the direction of the conclusions (odds ratio=1.2; 95% confidence interval=0.5, 2.9; p=0.828).
CONCLUSIONS:
RCTs on yoga that are conducted in India have about 25 times the odds of reaching positive conclusions as those conducted elsewhere.
Amazing how the positive results of large swaths of pseudo-medical studies can be biased by the culture in which they are done. It would appear that the country of origin may have a far more positive effect on a SCAM study outcome than the effect of when a real medication trial is funded by pharmaceutical companies. Money, as Cindy Lauper noted, changes everything, but world view with its concomitant bias is likely more important. Ioannidis was understating the issue when he noted:
Prejudice may not necessarily have financial roots. Scientists in a given field may be prejudiced purely because of their belief in a scientific theory or commitment to their own findings. Many otherwise seemingly independent, university-based studies may be conducted for no other reason than to give physicians and researchers qualifications for promotion or tenure. Such nonfinancial conflicts may also lead to distorted reported results and interpretations.
It is amazing how such bias can lead to the inability to see effects even when it is staring you in the face. My favorite example is “Decreased Risk of Stroke in Patients with Traumatic Brain Injury Receiving Acupuncture Treatment: A Population-Based Retrospective Cohort Study” where they conclude:
Patients with TBI receiving acupuncture treatment show decreased risk of stroke compared with those without acupuncture treatment.
even though patients:
with acupuncture treatment had higher proportions of using anticoagulants (2.3% vs. 1.7%, p = 0.0003), antiplatelet agents (28.7% vs. 22.3%, p<0.0001), and lipid-lowering agents (24.7% vs. 18.4%, p<0.0001) compared with those had no acupuncture treatment.
The use of anti-stoke medication was then ignored as the possible explanation of the ‘effects’ of acupuncture.
Of course, acupuncturists are not the only ones who cannot look at data and see the obvious.
Chiropractors like to point to “Risk of Vertebrobasilar Stroke and Chiropractic Care Results of a Population-Based Case-Control and Case-Crossover Study” as evidence that their particular pseudo-medicine does not cause strokes.
We found no evidence of excess risk of VBA stroke associated chiropractic care compared to primary care.
Although as I have mentioned in the past the paper does suggest that in a group that should not be having strokes, the young, seeing a chiropractor is associated with having a stroke.
Table 3 has the smoking gun. The highest odds ratio (14) for a stroke is 12, 4 times any other, in the age less than 45 in the first 24 hours after a visit to a chiropractor.
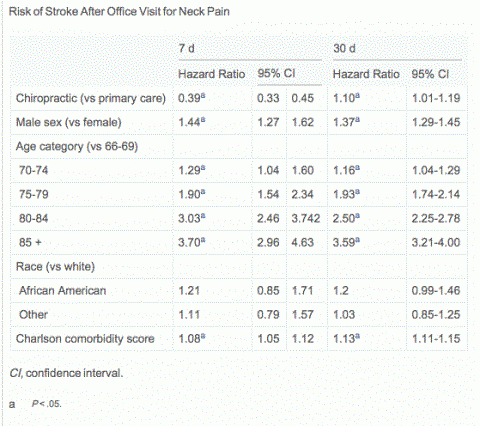
Saying that a paper does not support chiropractic as a risk of stroke when the data suggests it probably does continues. In the study “Risk of Stroke After Chiropractic Spinal Manipulation in Medicare B Beneficiaries Aged 66 to 99 Years With Neck Pain” by a chiropractor, suggests the older you are, there may be greater the risk of stoke after visiting a chiropractor.
They conclude that
Among Medicare B beneficiaries aged 66 to 99 years with neck pain, incidence of vertebrobasilar stroke was extremely low. Small differences in risk between patients who saw a chiropractor and those who saw a primary care physician are probably not clinically significant.
Given that the chiropractic cohort was both younger and healthier, and the rarity of stroke, I am not sanguine that this study can be used as evidence that chiropractic neck manipulation is safe and it suggests that, as the older you get, the more likely chiropractic will be associated with a late stroke, a 10% increase at 30 days that was statistically significant. But if due to chiropractic cannot be determined from the study
They suggest it may not be clinically important. While a 10% change in a pain scale may not be clinically relevant, I am not so sure a 10% increase in stroke has the same degree of triviality.
I am also not sanguine the study supplies evidence that chiropractic is safe; it is more spin than fact. Like the Cassidy study, it suggests that a risk of stroke is lurking in the background in some populations, is rare, and hard to see. For now I will stick with the preponderance of data, nicely summarized by the AHA position paper:
Although current biomechanical evidence is insufficient to establish the claim that CMT causes CD, clinical reports suggest that mechanical forces play a role in a considerable number of CDs and most population controlled studies have found an association between CMT and VAD stroke in young patients. Although the incidence of CMT-associated CD in patients who have previously received CMT is not well established, and probably low, practitioners should strongly consider the possibility of CD as a presenting symptom, and patients should be informed of the statistical association between CD and CMT prior to undergoing manipulation of the cervical spine.
And when I see an article called “Is there a role for neck manipulation in elderly falls prevention? – An overview“, I think NONONONONONO.
That’s my bias, and I am sticking to it.