[Editor’s note: Not enough Clay for one day? Check out this post on homeopathy over at The Scientific Parent!]
It was recently brought to my attention that a chiropractor was promoting his profession on Facebook by claiming to have treated and cured a potentially life-threatening cardiac arrhythmia. The condition in question, supraventricular tachycardia (SVT), can be very serious and even deadly in patients of all ages. Needless to say, the thought of anyone but a well-trained medical professional with access to appropriate medication and equipment to control the heart rate if necessary was unsettling to say the least.
After a deep breath, I followed the link and was sadly not surprised to find that it was true. In fact, after taking a minute for the rage to subside, and a few more to delve deeper into the case, I found that it was in reality much worse that I had initially imagined. The intervention, a stealthy adjustment of the child’s first cervical vertebrae, was performed by her father while she was being treated in a neonatal intensive care unit just hours after being born.
The events in question were posted by the chiropractor on a public account for his practice. Still, I feel hesitant to link to them directly as they reveal not only the name of the child but the identity of the cardiologist and intensive care doctor involved in her care (who naturally cannot respond because of privacy laws). If readers want to go to the trouble of locating the source of my outrage, they certainly can.
I will provide details of the child’s care as described by her father, but first a brief primer on SVT to set the stage a bit.
What is supraventricular tachycardia?
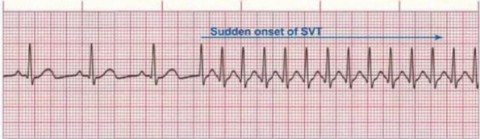
SVT is the fancy medical name for an excessively fast heart beat that has an origin above the heart’s lower chambers, also known as the ventricles, which pump blood out of the heart into either the lungs or the rest of the body. SVT, which is the most common abnormal cardiac rhythm diagnosed in children, typically occurs in patients with a normally-formed heart and no other medical problems, but is more likely to occur in the presence of congenital heart defects. Regardless of whether the heart is structurally normal or not, the problem stems from an abnormality in the conduction pathway that defines the electrical communication between the upper and lower chambers.
In a neonate, the most common form of SVT is known as atrioventricular reentrant tachycardia (AVRT). The electrical activity within the muscle of the heart under normal circumstances is initiated in the upper chambers and passes into the lower via the AV node, a specialized collection of cells between the chambers that slows conduction just a bit in order for the ventricles to fill with blood prior to their contraction. AVRT becomes possible only when an accessory pathway for electrical activation of ventricular contraction exists that bypasses the normal route.
Electrical signals can pass through the accessory pathway from the atria to the ventricle or vice versa. Anterograde conduction results in a signal that bypasses the AV node and avoids that important slight delay. This “preexcitation” can be seen on an EKG as the infamous “delta wave” that medical students and residents learn about several hundred times during their training, despite it being relatively uncommon. Patients who develop SVT in the setting of preexcitation are diagnosed with Wolff-Parkinson White syndrome (WPW). Retrograde conduction absent SVT, where the accessory pathway allows electrical activity to pass from the ventricles back into the atria, cannot be seen on ECG.
The process that results in abnormally increased heart rate in SVT, which can be as fast as 300 beats per minute in young infants (normal is less than half of that) and 220 to 240 in older children, is when a reentrant circuit forms. The most common form of this, seen in roughly 95% of cases, is when electrical conduction goes through the AV node and then quickly moves retrograde through the accessory pathway where it can go right back through the AV node. This results in the impressively fast heart beat associated with SVT and can lead to a variety of clinical presentations.
How does SVT affect children?
Despite heart rates that seem too fast to believe, most episodes of SVT occur suddenly, stop without any intervention within 10-15 minutes, and are clinically silent. Some episodes resolve spontaneously within a couple of minutes while others, less commonly, last much longer. When they do cause symptoms, older patients will often describe heart palpitations (the sensation of their heart beating in an abnormal way), chest pain, and feeling tired or lightheaded. Infants and toddlers, who obviously can’t express what they are feeling, may just act fussy or funny.
Some patients will actually lose consciousness because of associated dips in blood pressure and poor perfusion of the brain with oxygenated blood. In general, the longer that an episode lasts, the more likely it is to result in more serious complications, and Wolff-Parkinson White syndrome in particular is associated with sudden death. Neonates and older infants, because persistent or frequent episodes are less likely to be recognized in a timely fashion, are much more likely to present in heart failure with excessive fussiness, poor sleep, feeding difficulty, bluish skin because of low oxygen levels, and abnormally fast and difficult breathing.
How is SVT diagnosed?
There are additional causes of SVT other than AVRT, although it is the most common of the vast majority of cases in kids under 2 years, and even in older children. Other potential etiologies can be associated with worse prognoses so it is extremely important for the right diagnosis to be made. This requires the involvement of a pediatric cardiologist and appropriate testing modalities, most importantly an ECG, but also an echocardiogram to rule out any structural abnormalities. Ambulatory monitoring of the heart at home is often necessary because of the sporadic and brief nature of most SVT episodes.
How is SVT treated?
In many cases of acute SVT, no treatment is required at all because it stops spontaneously without any intervention. The parent or patient may even be completely unaware it happened. When a child with SVT does come to the attention of medical professionals, whether in the office, emergency department, or inpatient unit, the first step is always an assessment of their hemodynamic stability. An ECG with continuous monitoring of the child’s heart rhythm is of course important as well, but assessing for evidence of low blood pressure, heart failure, and shock is critical.
Stable patients, which make up the majority of cases, are typically managed conservatively at first, but still with urgency. The goal is always to convert the rhythm back to normal – we don’t wait to see if it will stop on its own. The initial approach is usually trying one of several vagal maneuvers, which can be done while appropriate resources and personnel are gathered for additional treatments if necessary. A vagal maneuver is one of several techniques employed in an effort to increase the activity of the vagus nerve, which can slow conduction through the AV node and convert SVT to a normal rhythm.
Vagal maneuvers can involve having an older and cooperative patient bear down as if trying to have a bowel movement or blow through an occluded straw. In younger patients and infants, a common vagal maneuver involves covering the face with a bag filled with ice water for up to 30 seconds in order to stimulate the “diving reflex” and slow AV nodal conduction. Massaging the carotid arteries or pressing down on the eyes have been tried historically but are currently not recommended in children because they are less effective and can cause harm.
Another key component of any vagal maneuver is close observation of the patient and their cardiac rhythm during the attempt. The particular pattern seen if successful can help diagnose the etiology of the SVT. And although rare, vagal maneuvers can potentially result in different and more concerning abnormal rhythms or even prolonged asystole, which is when the heart fails to contract at all. Sometimes parents of older patients are counseled to evaluate their child at home and perform or assist in vagal maneuvers. To perform an unsupervised vagal maneuver on a newborn having their first episode of SVT is, well, I’m getting a little ahead of myself. Let’s put a pin in that for the moment.
If vagal maneuvers were to fail, and the child remains stable, the next step in treatment is almost always big pharmaceutical. The drug of choice is adenosine, which acts on cardiac cell surface receptors leading to an increase in the normal AV node delay in conduction. This can interrupt the reentrant circuit that is usually causing all the fuss in the first place.
Adenosine is an IV medication that acts extremely rapidly, usually within seconds. Continuous ECG monitoring is a must in order to document what happens and help make the diagnosis. It has an extremely high rate of successful conversion to normal rhythm in most cases of pediatric SVT, but should be avoided in some circumstances. It can worsen the situation if used in a patient with WPW, for example. Adenosine should never be given without the team being ready to provide emergency resuscitation if needed.
Patients who are unstable at presentation are treated very differently. Time is never wasted on vagal maneuvers or even medications. Instead, the child is given appropriate sedation and electrode paddles are used to cardiovert (i.e. shock) the rhythm into a normal pattern.
What are the long term implications of SVT?
SVT can recur in many children. Depending on the etiology, the risk of recurrence can be higher or, as in the case of WPW, associated with more concerning acute events, even sudden death. I won’t get into too much detail on this because it is complex and there is much less of a clear evidence base to go on. Essentially, some children can be observed without any preventative medications, just counseling on recognition, use of vagal maneuvers, and when to seek medical attention. Some children may be placed on medications or even undergo procedures to remove the abnormal accessory pathway. Luckily, many young children who are diagnosed will stop having episodes as they age.
Chiropractic management of SVT in a newborn infant?
Now back to the case in question, which to refresh your memory involved the patient’s father, a chiropractor, claiming to have successfully treated his child’s SVT while in the NICU (emphasis added by me for future reference):
…Within an hour (of being born), things became very serious as her heart rate went to 300+ BPM and was taken to the special care nursery. Nobody knew what was going on and they had called care flight to take her to another hospital. As the nurses stepped out of the room to make arrangements to move my daughter to another hospital, I decided to step in and check her out while all the nurses were out of the room. As I walked closer I began to pray and cry, I thought my girl was dying. With one adjustment to her atlas (C1), her heart rate fell to zero and then quickly back to up to 140. The nurses all rushed in to see what was going on. To their astonishment, Gemma’s heart rate was normal. They had no clue what had just happened and so I told them I adjusted her…By removing the interference, her parasympathetic nervous system took back over and did what it was suppose to [sic] do.
From another post in which he throws the obstetrician under the bus (emphasis added by me for future reference):
…Our bodies are self-healing and self-regulating and our nervous system is the master system and master controller of our body. Without interference it functions correctly. So what happened to Gemma? Her ability to self heal and self regulate was taken away. She was healthy before birth, her delivery was quick and the doctor pulled too hard on her neck. Her atlas was subluxated causing interference of her parasympathetic nervous system, specifically the Vagus nerve, which slows heart rate. Without the inhibition of the parasympathetic nervous system, the stress of being born caused her sympathetic nervous system to speed up her heart rate. The adjustment allowed her brain to function correctly and self regulate her heart rate. Without an adjustment, Gemma could have possibly died, been injured, or have been on harmful medications the rest of her life. How many kids are medicated because their nervous system isn’t functioning properly? EVERY kid needs to get checked by a ChiropracTOR. [sic] Their health and well-being depends on it. You may just be saving their lives! Feel free to share.
There is a lot to unpack here but I’ll do my best. From the information provided, if accurate, it is very likely that this child did in fact have an episode of SVT. It’s possible, but very unlikely, that something else such as pain or illness caused the heart rate to increase to that degree. Usually that can be differentiated fairly easily. Fast but normal rhythm is usually variable with swings up and down, while with SVT it appears to be stuck at one rate. Also this child, from what I can tell, was otherwise perfectly healthy.
Twice he mentions that nobody knew what was going on. This seems odd as SVT is a pretty well recognized phenomenon in both pediatric and adult medicine. This child was born at around 11PM and the increased heart rate wasn’t noticed until an hour after birth. In most nurseries, this means that the pediatrician would not see the baby until the morning. Even if the facility, like my own, has an in-house pediatrician 24 hours a day, healthy babies aren’t typically seen right away unless there are problems.
This facility apparently has a special care nursery, which is usually considered the equivalent of a level 2 NICU. Babies of moderate prematurity (32 weeks gestational age and up) and/or illness can be managed in a special care nursery without needing to be transferred to a higher level of care. I would have thought that routine SVT would not require transfer.
There is no mention of a neonatologist or pediatrician being involved with the initial care of the baby, which leads me to think that this hospital doesn’t have one in-house. The father did provide a photo of a rather unhelpful consultation note from a pediatric cardiologist the following day, which also names a neonatologist, however. Any neonatologist or pediatric hospitalist would have recognized SVT and treated appropriately. Of course the provided narrative might be missing important details for dramatic effect or because of simple frailty of human memory.
Sneaking into a child’s room, even your own, in order to avoid awareness of the hospital staff is shady to say the least. I have no idea what kind of neck adjustment this father performed, but I imagine that it involved some kind of high velocity technique that would have been concerning to nursing. If he was simply going to break out his Activator, why hide it?
The father’s understanding of the pathophysiology of SVT is completely wrong. SVT isn’t caused by a malfunction in the nervous system or brain, it is almost always caused by an accessory pathway for electrical conduction in the heart. The problem isn’t an overactive sympathetic nervous system (think fight or flight), or even suboptimal parasympathetic activity (think rest and digest). Vagal maneuvers are an attempt to hyperstimulate the nerve and increase parasympathetic action above normal in order to convert the rhythm.
The father also demonstrates a lack of understanding of basic neuroanatomy despite all of that focus on it in chiropractic colleges. Manipulating the spine in any way is not going to have an effect on the origin of the vagus nerve, also known as the tenth cranial nerve, which lies in the brain stem’s medulla oblongata within the base of the skull. Even a complete injury to the spine at the level of the first cervical vertebra, which is where the father claims his child had a subluxation, would not result in changes in the heart rate let alone SVT because the vagus nerve doesn’t live there.
The roots of the vagus nerve exit the skull via bilateral jugular foramen and travel with the jugular and carotid vessels on each side of the neck. This is why carotid massage can sometimes stimulate it and convert SVT. In fact, all vagal maneuvers attempt to stimulate the nerve at the point where it runs though the neck. So it is entirely possible that a chiropractic adjustment might “work” in the sense that somebody is potentially pressing down on the side of the neck for several seconds. The more likely reason that this child’s SVT converted is because SVT tends to just stops on its own.
As a pediatrician who often cares for very ill children, and a parent myself, I can certainly relate to the feelings of panic and fear expressed by the child’s father. He may have actually thought his baby was going to die, suffer injury, or go on to require harmful medications for the rest of her life. Apparently the possibility of life flight was even on the table and there doesn’t seem to have been anyone there to talk the family through the situation. In reality, the child needed appropriate medical care but was actually at fairly low risk of any of those concerns.
Chiropractic fear-based marketing
I probably wouldn’t have written about this if the father hadn’t turned the events into a marketing gimmick on his chiropractic practice’s public social media page. It’s a practice building scheme I’ve written about before several times and it’s as cheap as it gets. What better way to sell a product, particularly if it provides no demonstrable benefit, than to make people afraid of life without it? Even more powerful is the fear that your child may suffer horrible illness, even death, if you don’t do what they recommend.
Chiropractors certainly aren’t alone in the use of this marketing tactic, but I think that they might be the best at it. Despite any evidence to support their claims, they want parents to think that hidden subluxations are a risk for a variety of problems, even SIDS and “shaken baby syndrome.” And these hidden subluxations can occur during routine delivery or even regular care and play. Here is a chiropractor demonstrating how to avoid injuring the spine while changing your baby’s diaper. If a diaper change can injure the spine, imagine what falling down while learning to walk must do!