The practice of medicine is an art, not a trade; a calling, not a business; a calling in which your heart will be exercised equally with your head.
The practice of medicine is an art, based on science.
-Sir William Osler, AEQUANIMITAS
The truth is that many of us have some kind of “extraordinary gift.” For a few of us, that gift is the ability to throw a ball at 90 miles per hour and hit a catcher’s glove. For others, that gift is a form of extraordinary perception. Medical intuitives “see” things that others don’t. Wendy Marks has been described as a “human CT scan.” What no one has been able to diagnose by conventional methods is often seen when Wendy scans a body.
–Boston Women’s Journal April/May 2002
The concept of an art to the practice of medicine comes up frequently and in a variety of contexts. Early on in our medical education, we are exposed to the phrase and what it supposedly means, which I will discuss in more detail shortly. But the art of medicine is always painted (pun intended) in a positive light. I will admit that I have a strong opinion, perhaps biased by my involvement with the science-based medicine movement and an equally early exposure during my medical training to champions of evidence-based practice and the use of critical thinking in the approach to patient care.
But first, imagine the following four scenarios:
- A patient seen by an emergency medicine physician for complaints of chronic mild and intermittent periumbilical abdominal pain has a normal physical exam. The physician establishes rapport with the patient while efficiently discussing her past medical, surgical, social and family history among other components of a thorough investigation. The patient is reassured that her normal exam, and a history absent any concerning red flags for organic illness, do not warrant additional laboratory or radiologic studies at this time. The physician discusses the potential role of stress in chronic abdominal pain and recommends that the need for outpatient mental health services be discussed with her primary care physician as well as implementation of lifestyle modifications such as increased exercise and a healthy diet with adequate intake of fiber. The patient is educated on possible concerning new signs or symptoms that would necessitate further work up.
- The same patient is seen by her primary care physician the following week. She has a normal physical exam. The physician establishes rapport with the patient while efficiently discussing her past medical, surgical, social and family history among other components of a thorough investigation. The patient is told that while her normal exam, and a history absent any concerning red flags for organic illness, are reassuring, in her experience some serious conditions can present without obvious findings in the early stages. The physician relates the story of a similar encounter during residency to one of her colleagues and sends the patient down the street for a number of metabolic studies and an abdominal CT to rule out inflammatory bowel disease. She is referred to a gastroenterologist.
- The patient is then seen by a local gastroenterologist one week later. She has a normal physical exam and no concerning red flags are discovered during brief questioning. The physician is in the room for about ten minutes when he abruptly recommends endoscopy to “see what’s going on in there” and shows her to the clerk for scheduling of the procedure. She is given a packet of information on the risks and benefits of the procedure and a prescription for medicine to clean out her bowels in preparation. She is reassured that biopsy findings will likely be normal and told that it is best to figure these things out so that she can quit worrying.
- The patient, having failed to show up for the endoscopy, is seen by a practitioner of Naturopathy recommended by a friend. The practitioner establishes rapport with the patient while discussing her past medical, surgical, social and family history along with a number of questions about potential exposures to chemicals and toxic substances in her environment and diet. The patient’s concerns are validated and she is warned that often problems like systemic yeast and various nutritional imbalances can present with vague symptoms but may become more debilitating. The practitioner orders a variety of metabolic studies as well as tests for heavy metals in the patient’s saliva, and he performs live blood cell analysis in the office. A number of supplements and a homeopathic remedy are prescribed, and acupuncture sessions are scheduled.
At first glance, especially to those who are familiar with and support the ideals of science-based medicine, it’s easy to see which of these scenarios is full of blatant pseudoscience and a good example of what goes on in the world of alternative medicine. Sadly, the practitioner of Naturopathy probably convinced our patient that she suffers from one of the many “one true causes” of all disease. You also probably realize, even without any specific medical training, that the physician in scenario 1 provided the most science-based approach to the patient’s symptoms, with excellent communication skills and an admirable level of comfort with a likely stress induced complaint.
In scenario 2, a well-meaning and competent personal physician perhaps placed too much importance on personal experience than was deserved, and I imagine this fictional doctor probably eschews what she perceives as excessive reliance on cookie cutter algorithms in “the real world.” The subspecialist in scenario 3 certainly didn’t demonstrate a good bedside manner, but probably meant well in his attempt to put his patient’s mind at ease with what is arguably an unnecessary invasive diagnostic procedure. All of these practitioners would almost certainly claim to be practicing the art of medicine, however, which should raise the question of just what the heck it means to do so.
What is the art of medicine?
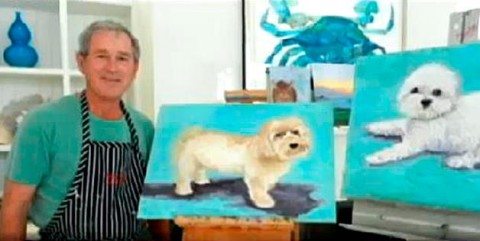
This is a question I have often asked myself. When doing so I am frequently reminded of how politicians present themselves to the public in radio and television spots, which essentially amount to “Candidate Jenkins is for good things and against bad things!”, or for the bad and against the good if you happen to fall on the other side of the political spectrum. But they don’t really tell you anything about the candidate as a person. In a similar fashion, talk of the art of medicine is almost always focused on the positive aspects. Always a Rembrandt, never a Bush.
According to Sharon Bahrych, a Denver-based physician assistant, in her post on KevinMD, the art of medicine involves several components:
- Caring for patients, showing honest concern and compassion
- Giving patients time, not rushing in and out of the exam clinic room, being patient with them, having a great bedside manner
- Using the evidence based medicine algorithms as a guideline, as we apply them to each and every patient we see. Understanding that every patient is an individual who has individual circumstances that affect their lives.
- Helping every patient to acquire the best outcome they can for themselves by working with them, educating them, coming up with a mutually agreed upon plan of action
This is in keeping with most examples of how the art of medicine is defined. It’s about compassion, communication, professionalism, respecting patient autonomy, treating each individual as a beautiful and unique snowflake, and not being afraid to go off protocol when things get squirrelly. It all sounds very nice and hard to argue with.
It’s particularly hard to argue with the narrative when people start dropping quotes from Sir William Osler, like I did at the onset of the post. Osler, widely considered to be the father of modern medicine, accomplished many things during his career, not the least of which was the medical residency as an entity and the push to teach the practice of medicine at the bedside more so than in the classroom. An even-brief skimming of his biography should be sufficient to leave any physician feeling rather inadequate.
Osler’s legacy consisted of much more than this. A variety of medical conditions and specific findings bear his name, as do many buildings. He also left us with a seemingly endless supply of quotes, with several appropriate candidates to choose from for the title slide of almost any PowerPoint presentation. His notable quotes regarding the art of medicine speak volumes. Osler called for physicians to care for the patient, not the disease. To employ empathy, humanity and love, and accept that uncertainty and error are unavoidable in the practice of medicine. And to respect experience as a means of learning the art of medicine, but never forget that the art is subservient to the science.
The most compelling aspect of the art of medicine involves communication. While it really doesn’t matter all that much if you are an excellent communicator full of empathy and love for a patient who was diagnosed with an ear infection, the next patient may not be so simple. As Harriet Hall once wrote, “Medicine is not an art like painting. Neither is it a science like physics. It’s an applied science.” While I often, with tongue in cheek, make the claim that a robot could perform a lot of my job successfully, nobody wants to be told that they have cancer by a machine. The application of science to the patient will always need a human component.
Is there a dark side of the art of medicine?
If, like the Force in the Star Wars Universe, the art of medicine manifests itself as our “compassion, selflessness, self-knowledge and enlightenment, healing, mercy and benevolence”, then it seems fitting that there would also be a dark side. As water takes the shape of the vessel which contains it, the fluid nature of this aspect of medical practice allows misuse in the wrong hands. There is, after all, an “art” to more than just medical practice. Proponents of chiropractic, acupuncture and naturopathy, not to mention every other alternative medicine modality, incorporate similar language into their propaganda.
The dark art, so to speak, of medical practice is often employed as a rationalization when ignoring established evidence. Medicine can be very complicated, messy even, but a great deal of it is actually fairly straightforward. We have picked a lot of the low- and even high-hanging fruit in regards to both prevention and treatment of injury and illness. And when we can’t cure, we can often manage symptoms and improve the quality of a patient’s life. Of course there are gaps in our knowledge, but those gaps are steadily shrinking. The so-called art of medicine does often thrive in those gaps, and that can be a good thing, but the gaps are also where there is the greatest potential for harm when seen as a license to do whatever you want regardless of plausibility and basic science.
What many people think of as an art in medicine is the ability to make a diagnosis. Mark Crislip once referred to it as a craft rather than an art, but I just call it pattern recognition. Dr. Crislip went on to further elucidate his concept of the art of medicine:
The Art in medicine may occur as thinking about cases moves more and more over time from the conscious level of a third year medical student to the subconscious level of an experienced clinician. I recognize subtleties and important findings faster than newbies or the inexperienced.
Over the decades, as evidence has accumulated, we have learned a vast array of patterns and associations that are beyond the ability of most if not all individual physicians to maintain a complete working knowledge of. Hence we must increasingly rely on specialists who focus on specific areas of medicine and, when possible, the incorporation of the available evidence into algorithms that fit most patients most of the time. It is hard to deny the improved accuracy and outcomes that this approach has led to.
Certainly there will always be exceptions where patients don’t present in such a way that an applicable protocol is easily chosen or even available, and diagnosis does elude us at times. And patients will not always respond to treatment as we expect them to. But we must be wary of experience-based practice that focuses too much on individualization. Without due caution, and awareness of the many biases and errors in perception that plague us all, the difference between expert-level subconscious pattern recognition and the bogus concept of medical intuition may not always be clear.
In the world of alternative medicine, the complexity of medicine is exchanged for the simplicity of pure invention and excessive generalization (everybody has a spinal subluxation), even while attacking medicine for not being holistic enough. While we may quibble about how much of a role art plays in medicine, it is all that alternative practitioners have to offer really, with rare exception. And examples of our occasional difficulty applying what we know to the individual patient commonly serve as justification to ignore scientific progress entirely.
Physicians aren’t immune to this. The art of medicine is often described as how we apply the science to the individual, but taken too far it can serve as a shield against criticism, a place for quacks of all kinds to take shelter against evidence. The art of medicine is all-too-often used as a conversation-ending justification for what is simply bad medical practice.
Conclusion
In my opinion, the phrase “art of medicine” needs to be retired or at least restricted in use. Aside from being nebulous to the point of nearly losing all meaning, and serving as fertile ground for all manner of bogus approaches to healthcare, to me it almost implies that there should be some kind of innate ability to practice medicine that some people have and some don’t. I don’t believe that there are medical equivalents of Leonardo da Vinci or Yo Yo Ma, virtuosos with skill that can’t be acquired by practice alone.
But we shouldn’t throw the baby out with the bathwater. While I certainly understand the desire to have an all-encompassing ideal phrase, I believe that we would be better served to be more specific when talking about the important aspects of being an effective healthcare professional, and more honest about when we are making an educated guess secondary to a lack of evidence. When a legitimate healthcare professional chalks their action up to the art of medicine, it lends credence to when a quack does the same thing.
Good communication, in my opinion, stands out as the most legitimate aspect of the art of medicine. While it is true that some people do have a knack for it, and even that some physicians will probably never develop into excellent communicators, the vast majority of physicians can be taught how to speak to patients competently. And preternatural communication skills aren’t called for very often in medicine.
I don’t know if the net positive benefit of focusing on the art of medicine is worth the negative. It probably is. Think of this as a conversation starter and please let me know your thoughts in the comment section. I feel very comfortable saying though that we would certainly be a lot better off if we focused more on critical thinking during medical training. A strong foundation in scientific skepticism would very likely decrease the potential for abuse of the art of medicine.