“Even in the Sickest of the Sick, Covid-19’s Effect on the Heart Appears to be Modest”
On May 14th 2021 Drs. John Mandrola, Andrew Foy, and Vinay Prasad wrote an article titled “Setting the Record Straight: There is No ‘Covid Heart’.” The article acknowledged “that SARS-CoV-2 can sometimes, though rarely, cause heart inflammation — just as many other viruses do”, but there was no indication that “SARS-CoV-2 had some special proclivity to harm the heart”. Fearful that needless tests may uncover incidental “injury”, causing unnecessary fear, they wrote “people who have recovered from Covid-19 have no special reason to worry about their hearts.” Even “in the sickest of the sick”, they wrote,
Covid-19’s effect on the heart appears to be modest. A London-based team reported on a series of 148 patients who had recovered from severe Covid-19. Cardiac magnetic resonance scans done during convalescence showed that nearly half of the individuals had no major heart abnormalities, and 9 out of 10 had normal heart function.
This referenced a study that found a “myocarditis-like scar in 26% (39/148), infarction and/or ischaemia in 22% (32/148) and dual pathology in 6% (9/148)”. Of course, a study that found that “nearly half of the individuals had no major heart abnormalities” also found that over half of the individuals did have major heart abnormalities. Nevertheless, it’s unclear what the clinical implications of this are, if there are any at all. After all, this was an imaging study and it’s not clear what to make of a “myocarditis-like scar.”
Generally, I liked this article. It acknowledged that COVID-19 can cause some heart inflammation, while pushing back on sensationalized narratives that captured the public’s attention. It reasonably concluded that “The issue of Covid-19 induced cardiac problems was massively overblown” and felt that the initial worries about “COVID heart” represented an opportunity to learn “lessons for how science is communicated to the public”. Though I feel it would have been strengthened had it mentioned myocarditis as a complication of multisystem inflammatory syndrome in children (MIS-C) in children, I agree that COVID-19 is scary enough without the need to exaggerate its dangers. The overall prognosis seems good too. Over a year into the pandemic, we are not seeing large numbers of post-COVID-19 patients with unexpected cardiac complications as far as I know.
The article noted that “incentives in the modern media” favor fearful headlines and that reassuring but more accurate information “won’t spread nearly as quickly”. Drs. Mandrola, Foy, and Prasad concluded their article by writing, “The broader lesson is that science communication in times of crisis must keep a level head. The public, and decision-makers, need properly controlled studies instead of early sensational reports”. I agree.
“Humans have only one heart; inflaming it at a young age is not a small thing”
With this in mind, it’s worthwhile to examine how one of these authors has since discussed vaccine-induced myocarditis. On July 1st 2021, cardiologist Dr. Mandrola wrote an article titled “Vaccine-Induced Myocarditis Concerns Demand Respect, Not Absolutism”. I won’t go over them all, but the article checked off many “red flags” I wrote about in my previous article on this subject. I urge you to read both our pieces. On balance, I feel that Dr. Mandrola’s article omitted key facts and rebutted invented arguments, overestimating the harms of the vaccine relative to the virus in the process.
Dr. Mandrola’s aim was “to argue that when it comes to vaccinating young people at low risk from the virus, parents and younger people should be allowed to weigh the vaccine decision with their clinicians without anyone being tarred as an antivaxxer.” I know of no one who would call parents and younger people antivaxxers for this reason.
In his article, Dr. Mandrola pushed back on those who called vaccine-induced myocarditis “mild” by writing,
I disagree; calling myocarditis mild reminds me of the saying about minor surgery. Minor surgery is surgery on someone else; mild myocarditis is something that happens to other folks’ kids. Humans have only one heart; inflaming it at a young age is not a small thing.
He rightly noted that affected young people were “discharged from the hospital” and said that, “As an electrophysiologist, I see the complications of myocarditis: heart failure and ventricular arrhythmia due to scar. Availability bias notwithstanding, heart rhythm doctors feel the asymmetry of myocarditis risk. Although it is true that most myocarditis resolves without issue, it is also true that sometimes it does not.” He favorably quoted University of Michigan cardiologist Dr. Venk Murthy, who said in a Twitter thread that influenced my thinking on this topic that, “people with myocarditis are usually counseled to limit activity, placed on 1 or more meds and are at lifetime increased risk of cardiac complications. This can have profound consequences.”
Dr. Mandrola worried that “minimization of harm from myocarditis, might reduce trust in messaging” about the vaccines, even in “at-risk adults who refuse the vaccine”. Was he at all concerned by those who minimize the myocarditis caused by the virus? No, he was not. He was only concerned that some minimized vaccine-induced myocarditis. I share Dr. Mandrola’s worry that the “minimization of harm from myocarditis” might be responsible for low vaccination rates in large swaths of the country. Many people are under the illusion that COVID-19 is completely harmless in children.
While he did acknowledge that COVID-19 has killed hundreds of children, something other articles on this subject neglected to do, Dr. Mandrola, a cardiologist writing about children, COVID-19, and the heart, did not even mention MIS-C-associated myocarditis in either of his articles, even though it is much more severe than vaccine-induced myocarditis and likely occurs at a slightly higher rate. In an article in which he says, “medical decisions should be made” with “judgment and benefit-harm balances and considerations of special circumstances”, he doesn’t even acknowledge the most severe form of cardiac damage to affect children and young adults during the pandemic. I will discuss it.
In addition to this, Dr. Mandrola belittled the successful vaccine trial in adolescents as follows:
After a “positive” trial in which just over 1100 kids aged 12 to 15 years received an mRNA vaccine, a movement arose to vaccinate young and old alike. I put “positive” in quotes for two reasons: The first is that this trial measured noninferiority of the immune response, not clinical outcomes. That was necessary because so few kids get sick with COVID-19. The other reason is that the authors claimed a favorable safety profile, but 1100 kids is not enough to inform the safety of a vaccine that will be given to many millions.
To be generous, this is only partially correct. The trial was titled “Safety, Immunogenicity, and Efficacy of the BNT162b2 Covid-19 Vaccine in Adolescents”. As the title clearly states, the trial evaluated “efficacy against confirmed coronavirus disease 2019”. Sixteen COVID-19 cases occurred among placebo recipients, while none occurred in those who received the vaccine:

A clinical outcome from a trial that Dr. Mandrola claimed did not measure clinical outcomes.
The trial authors wrote that “the vaccine efficacy in this trial provides a high level of certainty about the efficacy results”. I would call this clinical outcome positive – without the quotation marks.
I confess to being confused by Dr. Mandrola’s description of this study. I think he means that severe clinical outcomes, being rare in children, couldn’t be evaluated in this study. This is true, as I will explain below. However, even if severe outcomes are not common, kids definitely get sick with COVID-19. In fact, sixteen children who received a placebo injection got COVID-19 in this trial. Dr. Mandrola does not believe it is a “clinical outcome” when an adolescent gets COVID-19 in a trial of a vaccine designed to prevent them from getting COVID-19. I bet most of his readers would disagree with him, however they wouldn’t know the vaccine prevented COVID-19 in adolescents unless they read the trial themselves. His article omits this fact.
Dr. Mandrola is right that this trial was not large enough to fully “inform the safety of a vaccine that will be given to many millions”. It was too small to detect rare events, such as myocarditis from the vaccine or serious complications from the virus. However, only the largest trials can detect rare events, and the rarer the event, the larger the trial must be to detect it. The adult vaccine trials, which were about twenty-times larger than the adolescent trials, also did not detect rare events, such as blood clotting with the Johnson & Johnson vaccine. The inability to detect rare events is a fundamental limitation of clinical trials, not a flaw of this particular trial.
Rare events can usually be detected once a vaccine or medication is taken by large numbers of people. This is why post-marketing surveillance, called a phase IV trial, is so crucial. It’s a fact that no serious safety signal emerged during the trial. The authors were not only justified to report this finding, the data from their study required it. They didn’t claim that rare side effects would not emerge once millions of children received the vaccine.
All of this makes me wonder. Other than a trial that enrolled hundreds of thousands of adolescents, which would be required to meaningfully detect a rare event such as myocarditis, is there anything a trial could do so Dr. Mandrola wouldn’t feel he had to put “positive” in quotes? Did he make his objections known when the plans for the adolescent vaccine trial were announced or only after it was completed? Has he been similarly critical of other randomized-controlled trials, or is this the only trial he has singled out this way? As he does not feel someone getting COVID-19 is a “clinical outcome”, what would he call it? Why didn’t he inform his readers that the vaccine prevented COVID-19 in adolescents? Would he have been similarly silent had the vaccine been significantly less effective at preventing COVID-19? We can only guess.
Dr. Mandrola also raised some challenging and important questions of his own. These questions are the core of the article and by far the best part, in my opinion. For example, he asked whether it was ethical for a hospital to mandate a vaccine in an “18-year-old who works in engineering, has no patient contact, and who recovered from COVID-19 a few months ago”. I hadn’t thought of such a nuanced question. He also asked, “would one shot (especially in younger males) offer a better benefit-harm calculus?” This is a very reasonable question as the myocarditis risk is highest in young males after the second vaccine dose. However, this would have to be weighed against seeming lower efficacy of one shot (Planas et al. and Bernal et al.) against the Delta variant compared to two shots. Given the rare outcomes it would have to detect, only a massive trial, which would likely take years just to enroll subjects, could definitively determine if one shot offered a better benefit-harm calculus than two shots. The Delta variant is now the dominant strain in the US, and given how fast it is spreading, there will not be time to fully study this proposal.
But it is an interesting and valid question, as are most of the questions Dr. Mandrola ponders. There are no clear-cut answers to many of them. As viral-induced immunity seems robust and long-lasting, I do not think the 18-year-old engineer should be required to receive a vaccine as long as he can document he was previously infected and no new information emerges about COVID-19 reinfection rates. You may disagree, but Dr. Mandrola is right- he is not an antivaxxer for asking these questions, nor am I for my response.
How common is vaccine-induced myocarditis?
Though we don’t know the true incidence, vaccine-induced myocarditis seems uncommon. According to the CDC, “The highest reporting rates were among males aged 12−17 years and those aged 18−24 years (62.8 and 50.5 reported myocarditis cases per million second doses of mRNA COVID-19 vaccine administered, respectively)”. This translates to about 1 in 16,000 for the highest risk group, males ages 12-17 years. Israel, however, reported a higher rate of myocarditis, from 1 in 3,000 to 1 in 6,000 males ages 16-24 years. We will better learn the true incidence over time, however likely the worst is over. Vaccination rates have been dropping steadily in the US, including for young people most at risk for myocarditis.
Is vaccine-induced myocarditis mild?
As a neurologist and psychiatrist, I view the heart as a pump to deliver blood to the brain, so I am a bit out of my territory when discussing whether or not myocarditis can be “mild”. However, most medical professionals with relevant expertise seem to think “mild” is an appropriate word to describe vaccine-induced myocarditis. The CDC noted that, of the 323 persons meeting their definition of vaccine-induced myocarditis, “309 (96%) were hospitalized. Acute clinical courses were generally mild; among 304 hospitalized patients with known clinical outcomes, 95% had been discharged at time of review, and none had died.” Multiple medical organizations, including the American Heart Association and American Academy of Pediatrics agreed and released a statement expressing their view. It said,
The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination. Importantly, for the young people who do, most cases are mild, and individuals recover often on their own or with minimal treatment. In addition, we know that myocarditis and pericarditis are much more common if you get COVID-19, and the risks to the heart from COVID-19 infection can be more severe.
Israel, which first sounded the alarm about the vaccine, also noted that “95% are considered to be mild cases…In most cases myocarditis took the form of mild illness that passed within a few days”. A co-author on his original article about “COVID heart”, Dr. Vinay Prasad, also wrote an article about vaccine-induced myocarditis with Drs. Venk Murthy and Brahmajee K. Nallamothu. It properly noted that rare side effects “could not have been detected in their clinical trials” and said about vaccine-induced myocarditis that, “Although most cases reported to date are mild and resolve without consequence, myocarditis can be a serious condition”.
Dr. Mandrola disagrees with this characterization, and I can see why. All but a few young people with vaccine-induced myocarditis have been admitted to the hospital for monitoring and have had elevated troponin levels, a marker of cardiac injury. Dr. Mandrola is right that I would not call this “mild” if it happened to my vaccinated son. Even if he was admitted “just for monitoring”, this would be frightening; I wouldn’t feel comfortable until he was back home and without symptoms for some time.
Fortunately, the vast majority of young people with vaccine-induced myocarditis do go home without symptoms. Most are hospitalized for only a short time, often just a couple days, and require only over-the-counter pain medications. Nearly 80% of cases have recovered without symptoms thus far, and the rest are presumably headed in that direction:
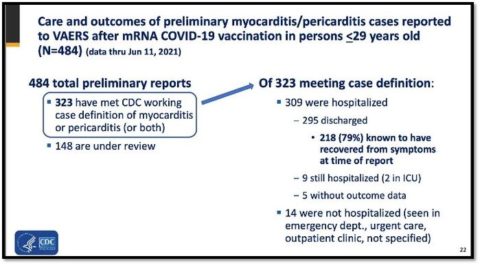
CDC data on vaccine-induced myocarditis
Most importantly, according to Dr. Katherine Poehling, a pediatrician on the CDC’s Advisory Committee on Immunization Practices (ACIP), no deaths or severe outcomes have been reported so far. (I’ve heard rumors on social media that the deaths of two teens are being investigated. Neither was diagnosed with myocarditis as far as I know, and history shows us why it is important not to jump to conclusions about these sad cases.)
Commenting on its favorable prognosis, Dr. Grace Lee, a pediatrician at Stanford, said “This is not like any myocarditis I’m used to seeing”. Dr. Sallie Permar, the chair of pediatrics at Weill Cornell Medicine and New York–Presbyterian Komansky Children’s Hospital, said children are being hospitalized “because we wanted to monitor them, out of an abundance of caution…Even the kids are asking, ‘Why am I going to the hospital?'” Other doctors who have treated and authored case series on these patients agree on the favorable outcome so far. Dr. James de Lemos, a professor of medicine, said, “They’ve all done well” and all recovered clinically after spending “just a couple of days” in the hospital. Dr. Pei-Ni Jone, a pediatric cardiologist, said, “The good news is, all these children recovered”.
Dr. Jone is right – this is good news, though these favorable outcomes are sometimes inexplicably omitted from articles on this subject. Dr. Mandrola’s article, for example, noted that no one has died from the vaccine and that “most of the affected kids recovered and were discharged from the hospital,” but otherwise provided no information on either the clinical course or frequency of vaccine-induced myocarditis.
So is vaccine-induced myocarditis “mild”? This is clearly a subjective question. I don’t think I’ve ever described it that way, though I’ve certainly quoted many others who have. In fact, as I wrote previously, to me it’s serious any time a young person gets admitted to the hospital, even if they leave after a few days of feeling well, as most seem to do. Cardiac injury, even if temporary, is obviously not trivial. Affected people are often advised to limit vigorous activity for 3-6 months, which must stink, especially during the summer.
Though vaccine-induced myocarditis is rare, rare harms multiplied by tens of millions of people add up. Over 1,000 cases of myocarditis have been reported to the Vaccine Adverse Event Reporting System (VAERS), and there are certainly cases that have gone unreported. While reports to VAERS do not prove causality, it’s clear that a large number of people, most of them young, have suffered from this problem. I fully agree with Dr. Mandrola that vaccine-induced myocarditis shouldn’t be minimized.
Happily though, the overall outcome of these cases is quite encouraging so far. Almost all seem to resolve in a short time without symptoms and with normal cardiac tests, such as ECGs and echocardiograms. These cases will have to be monitored over time, but hopefully this pattern will continue. Overall, I think the CDC has done an admirable job of informing the public about vaccine-induced myocarditis in a transparent way. The CDC says that it will continue to “closely monitor reports of myocarditis after receipt of the mRNA COVID-19 vaccines and will bring any additional data to ACIP for consideration”. For now, if it is ever appropriate to call myocarditis mild, vaccine-induced myocarditis seems to fit the bill.
How common is COVID-induced myocarditis?
MIS-C occurs in about 1 in 3,200 children infected with COVID-19, and thus far it has affected at least 4,196 American children, perhaps many more as cases may be undercounted. According to the CDC, “The median age of patients with MIS-C was 9 years. Half of children with MIS-C were between the ages of 5 and 13 years.”
In one study of 191 children with MIS-C “53% had evidence of myocarditis, 80% were admitted to an intensive care unit and 2 died”. A systematic review of 15 case series/reports found that 75% of children with MIS-C have myocarditis. Of course, MIS-C is not the only way that COVID-19 can cause cardiac damage, especially in adults, but this damage is harder to define and quantify.
Is COVID-induced myocarditis mild?
In contrast to vaccine-induced myocarditis, COVID-19 can cause severe cardiac complications. There have been cases of fulminant myocarditis in COVID-19, though it seems to be rare. Additionally, myocarditis and coronary artery aneurysms frequently occur in children with MIS-C. Other studies have reported acute heart failure in children with MIS-C. Other common cardiac complications of myocarditis due to MIS-C include “shock, cardiac arrhythmias, pericardial effusion, and coronary artery dilatation”. Cardiac arrhythmias have led “to hemodynamic collapse and need for ECMO support” in some children. This heart damage doesn’t seem “modest” to me.
Children with MIS-C are extremely sick and are treated with much more than over-the-counter pain medications. Dr. Cleavon Gilman has a heart wrenching Twitter thread of some of their stories, though it’s not as devastating as his thread on children who have died of COVID-19. Dr. Gautam Singh, chief of pediatric cardiology at Children’s Hospital of Michigan, who authored a study on cardiac dysfunction in children with MIS-C, said, “Almost invariably, half of them required going on mechanical ventilation or a breathing machine, heart-supporting medications”. 37 children have died of MIS-C. None of this has happened with vaccine-induced myocarditis, thankfully.
In contrast to vaccine-induced myocarditis, the effects are longer-lasting, though happily most children seem to recover well. Dr. Singh said about children in his study, “Fortunately, they all did very well, and they went home, which is great gratification. When we studied these children and followed them about five to six months (later), we found about 19% to 20% have some involvement of their heart function that was not clinically obvious, but by echocardiographic measurements.” One review found that 6%-14% of children had persistent ventricular dysfunction when they left the hospital. As with vaccine-induced myocarditis, the long-term consequences of this, if any, will only become apparent over time.
Dr. Mandrola wrote in his article that, “A neutral observer might wonder: well, if folks were that excited about myocarditis in young people after the infection, why are they not equally worried about this early signal of harm from the vaccine?” I understand this neutral observer’s confusion, especially if she has thus far only read articles that neglect to mention myocarditis due to MIS-C or elaborate on the favorable prognosis of vaccine-induced myocarditis. I imagine that once the neutral observer learns this information, she will better understand the asymmetries in the concern.
To summarize how COVID-19 has harmed children and young adults thus far, it has killed 488 children younger than 17 years and 2,682 young adults ages 18-29 years. It has hospitalized tens of thousands or even hundreds of thousands of children, even accounting for the fact that many tallies include incidental COVID-19 cases in children hospitalized for other reasons. Several studies (Kim et al. and Havers et al.) found that one-third of hospitalized children go to the ICU and about 5% need mechanical ventilation. There are more questions than answers about long-COVID in children, but I feel comfortable saying that a lot of children felt sick for a long time, even though fortunately the overwhelming majority are perfectly fine.
After reviewing all the data, the CDC concluded that “the benefits of vaccinating all recommended age groups with mRNA COVID-19 vaccine clearly outweigh the risks of vaccination, including the risk of myocarditis after vaccination.” They calculated that,
Per million second doses of mRNA COVID-19 vaccine administered to males aged 12–29 years, 11,000 COVID-19 cases, 560 hospitalizations, 138 ICU admissions, and six deaths due to COVID-19 could be prevented, compared with 39–47 expected myocarditis cases after COVID-19 vaccination.
Notably, this “analysis did not include the potential benefit of preventing post-COVID-19 conditions, such as prolonged symptoms and MIS-C”.
Though Dr. Mandrola claimed it was “dubious to force young people to expose themselves to a risk for an unknown benefit to society”, this is another rebuttal to a non-existent argument. Everyone is very clear: the primary reason to vaccinate young people is to protect them from COVID-19. It’s just a nice bonus that they are also less likely to spread a deadly virus to a vulnerable family member, teacher, or coach. After all, one study found that 43,000 children lost a parent to COVID-19 and assuredly some children have infected their family this pandemic. Losing a parent hurts children too.
Whether myocarditis is serious or not should not depend on its cause
In my opinion, whether myocarditis is serious or not depends on the symptoms it produces and the damages it does, not on its underlying cause. Dr. Mandrola does not seem to agree.
When discussing viral-induced cardiac damage he wrote that “the issue of Covid-19 induced cardiac problems was massively overblown” and “even in the sickest of the sick, Covid-19’s effect on the heart appears to be modest”. Remember, this statement was written in reference to an imaging study that found 28% of patients with severe COVID-19 had infarcted myocardium, which is dead heart tissue, or ischemia, a lack of blood flow that causes injury and infarction. These statements were also written well after it was known that COVID-19 had caused severe myocarditis in several thousand children with MIS-C, though Dr. Mandrola doesn’t acknowledge this in his articles. In contrast, when discussing less severe vaccine-induced myocarditis, he wrote, “Humans have only one heart; inflaming it at a young age is not a small thing”. So, which is it?
On March 10th 2021, he said on Twitter that the pandemic was “essentially done” and that “human life has to be more than avoiding one pathogen”. He compared a contagious virus to bike injuries. He implored former CDC director Dr. Tom Frieden to stop discouraging behaviors, namely congregating indoors, that spread the virus. By this point hundreds of American children had already died of COVID-19 as had thousands of young people between the ages of 18 to 30. Tens of thousands (or more) of children and young adults had been hospitalized due to COVID-19, many ending up in the ICU due to MIS-C and myocarditis. Despite this, Dr. Mandrola said that the “young have almost no risk” from the virus. In contrast, when discussing less severe vaccine-induced myocarditis, he emphasized that affected young people were “discharged from the hospital”. He further wrote that “calling myocarditis mild reminds me of the saying about minor surgery. Minor surgery is surgery on someone else; mild myocarditis is something that happens to other folks’ kids.” So, which is it?
His concern about the long-term prognosis seems similarly dictated by the cause of the myocarditis. In his article on the virus, he wrote that “people who have recovered from Covid-19 have no special reason to worry about their hearts”. Again, this statement was written after it was known that some children with myocarditis due to MIS-C have persistent cardiac dysfunction at hospital discharge. In contrast, when discussing less severe vaccine-induced myocarditis, he warned of “complications of myocarditis: heart failure and ventricular arrhythmia due to scar”. So, which is it?
Either of his two positions alone seems reasonable to me. It is reasonable if a doctor believes the effects of COVID-19 on the heart are generally “modest” even in the sickest patients, and long-term consequences are nothing special to worry about. It is reasonable if a doctor believes that myocarditis is never “mild” and long-term consequences are definitely something to worry about. However, I find it problematic when a doctor, who doesn’t want to be tarred as an antivaxxer, takes both of these positions, within weeks of each other, dependent entirely on whether the cause of the heart injury was the virus or the vaccine and in inverse proportion to both the severity of the damage and the number of affected children.
It is reasonable to expect a doctor with a large platform writing for the public about children and a deadly virus to be accurate, consistent, and thorough, especially considering the questions he poses are important and don’t have clear answers.

