Humans evolved in an environment where they were exposed to animals, dirt, and a variety of pathogens and parasites. Our immune systems evolved to cope with that environment. Now most of us live in a different environment, with safe drinking water, flush toilets, food inspection, immunizations, and public sanitation. This means that we are far less likely than our ancestors to die of infectious diseases or to harbor intestinal worms. But it seems that the cleaner we get, the more likely we are to suffer from allergies and autoimmune diseases. One hypothesis is that our immune systems evolved to require early challenges by parasites and pathogens in order to develop properly. A hygienic environment fails to give our immune system the exercise it needs, resulting in imbalances and malfunctions.
The hygiene hypothesis was first proposed to explain observations like these:
- Hay fever and allergies were less common in large families where children were presumably exposed to more infections through their siblings.
- Polio attack rates were higher in high socioeconomic groups than in lower ones.
- Allergies and many other diseases were less common in the developing world.
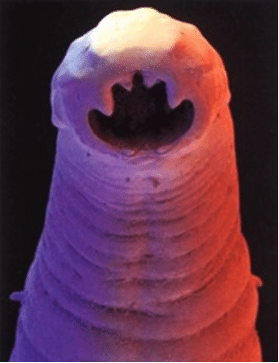
Investigation of these and other phenomena is contributing to a better understanding of the immune system, which is a good thing. At the same time, it has led some people to deliberately infect themselves with intestinal worms in an attempt to cure their allergies and autoimmune diseases, which may not be such a good thing. These treatments are far from ready for prime time, are risky, and they have a high yuck factor. The very idea of deliberately infecting yourself with worms is unpalatable, and finding wiggly live creatures in your stool or passing a 20 foot tapeworm are not generally considered to be pleasant experiences.
The immune system is an incredibly complicated mesh of many different components that interact with each other. The hygiene controversy focuses on Th1 and Th2. To grossly oversimplify, Th1 responds to intracellular pathogens (bacteria and some viruses) and Th2 responds to multicellular parasites like intestinal worms. They produce different kinds of cytokines, but there is a confusing overlap. Th1 produces inflammation and Th2 suppresses some of that Th1 inflammation and contributes to a pregnant woman’s ability to tolerate the fetus, but it is also involved in producing allergic reactions. Over-activation of either pathway can cause disease, and either pathway can down-regulate the other. Th1 and Th2 were originally thought to act like a seesaw where one goes up as the other goes down; but it turned out not to be that simple. An early hypothesis was that allergies resulted from an imbalance between the two, and that allergen exposure could somehow restore a balance. The subject is complicated. The more I try to understand the details, the more my head hurts. I hope my superficial description hasn’t misrepresented the truth too badly.
In his book An Epidemic of Absence: A New Way of Understanding Allergies, Moises Velasquez-Manoff compiles an impressive array of evolutionary arguments and evidence, everything from epidemiologic studies to personal anecdotes, to support the idea that early exposure to bacteria and parasites would reduce the incidence of allergies and autoimmune diseases, and that exposure after the condition had already developed would reduce symptoms. His book is exhaustive and I found it exhausting to read. It buried me in a mass of repetitious details.
It is an eye-opening book in more ways than one. He describes his own difficult quest to obtain worms to treat himself for his allergies and his alopecia. He has to negotiate with the hookworm underground and travel to Tijuana. He applies the larvae to his forearm and lets them burrow into his skin. Almost immediately, he feels “remarkably crappy.” He gets a headache, a hungover feeling, bloating, cramping, itchy bumps on his arm where the larvae entered, vertigo, cramps, diarrhea. The headaches lingered, but the other symptoms eventually subsided. His skin improved, his hay fever disappeared, and his sinuses were clearer for a while; but then his allergies returned with a vengeance. A stool test showed no whipworms. He assumed they had all died and would have to be replaced with new ones, but he was reluctant to let any more hookworm larvae burrow into his arm and risk experiencing all those unpleasant side effects again. He gave up on the experiment, but later his symptoms cleared again and whipworms showed up again in his stools. It’s far from clear what happened. He likes to think it has something to do with the optimum dose. He says, given his symptoms, that he would never recommend hookworms and would never deliberately administer them to his daughter… unless he was sure that she was destined to develop Crohn’s disease and debilitating allergies. Even then, he couldn’t be confident that the treatment would be effective, and he recognizes that only science can settle the question. He recounts many stories of other people who tried worm therapy and their conflicting results. They tried whipworms, hookworms, and even tapeworms, both from species that infect animals and from those that infect humans. Some people claimed to be cured. Some were improved for a time but symptoms recurred when their worms died and they had to keep infecting themselves with new ones. Some got so sick they had to be de-wormed. Some thought they got results but they also got side effects that they were willing to put up with. As with all testimonials, there is no way to know whether improvements were due to the worms or were coincidental.
Worm therapy is being seriously studied as a treatment for inflammatory bowel disease (Crohn’s disease and ulcerative colitis), celiac disease, and multiple sclerosis. Preliminary results are encouraging, but they are mostly case reports and uncontrolled open label studies. Carefully controlled studies are needed. It’s complicated; for instance, hookworms appear to reduce the risk of asthma but roundworms increase the risk.
Epigenetics and the environment in the womb come into play. Children born to mothers who were exposed to cowshed microbes were less likely to develop allergies. A double-blind randomized controlled study in Uganda showed that deworming pregnant women reduced the odds of her child developing allergic eczema by 82%. One might have expected that would make the child more susceptible, not less. The effects of bacterial exposure are different from those of parasite exposure. It’s complicated.
How ironic that the anti-vaccine folks are worried that vaccines might “overwhelm” the child’s immune system! Far from being overwhelmed, it appears the child’s immune system is not being exercised enough. It apparently needs more practice responding to microbes and parasites in early life in order to avoid allergies and autoimmune diseases in later life.
In a related development, fecal transplants and probiotics are proving to be effective in treating certain health conditions. We have only recently begun to learn about those other organisms that live in our body and outnumber our own cells by ten to one: our microbiome. Our internal and external ecosystems both affect our health. No man is an island.
Conclusion: An interesting, unproven hypothesis
Germs, worms, allergies and autoimmune diseases are all part of a complex web. If we come to understand the complexities, it could well lead to new strategies to prevent or treat allergies, diabetes, and a host of other diseases. But I don’t think we want to return to an unhygienic, parasite-laden environment. And I question the wisdom of deliberately infecting oneself with worms at this point in history, given the present state of knowledge. Not only is the evidence far from conclusive, but worms are yucky.