Blogging is a rather immediate endeavor. Over the last nine years (nearly), I’ve lost track of how many times I saw something that I wanted to blog about but by the time I got around to it, it was no longer topical. Usually what happens is that my Dug the Dog tendencies take over, as I’m distracted by yet another squirrel, although sometimes there are just too many targets topics and too little time. Fortunately, however, sometimes the issue is resurrected, sometimes in a really dumb way, such that I have an excuse to correct my previous oversight. This is just such a time, and the manner in which the topic has been resurrected is every bit as dumb as the rant by the Food Babe that Mark Crislip so delightfully deconstructed last Friday. Unfortunately, for purposes of snark, I’m not Mark Crislip—but, then, who is?—but fortunately I am known elsewhere (and sometimes here) for being a bit “insolent.” So let’s dig in. We’ll start with the idiocy and then use that as a “teachable moment” about cancer biology. Funny how I manage to do that sort of thing so often.
Abuse of cancer science for political purposes
I realize that we at SBM are supposed to stay, for the most part, apolitical, but the idiocy that’s leading me to revisit a topic is unavoidably political because it involves using a profound misunderstanding of science for political ends. Specifically, I’m referring to the misuse of a legitimate scientific debate about cancer screening and diagnosis for purely political ends. First, however, for those not living in the US or my fellow citizens who might be blissfully unaware (in this case) of recent events, during the first half of October, our nation underwent what can only be described as a self-inflicted crisis that could have caused worldwide economic turmoil if it hadn’t been (sort of) resolved at the last minute. The reason for the crisis boiled down to the extreme resistance of some of our more radically conservative Representatives to the Patient Protection and Affordable Care Act, usually referred to as just the Affordable Care Act (ACA) or, colloquially, Obamacare. Normally when we write about Obamacare here on SBM, it’s to complain about how advocates of unscientific medicine and outright quackery have tried to piggyback their advocacy on the ACA in order to have health insurance plans sold through government exchanges cover modalities like naturopathy, chiropractic, and other so-called “complementary and alternative medicine” (CAM) or “integrative medicine.” In related posts, I’ve examined the evidence with respect to the relationship between health insurance and mortality and whether attacks on Medicaid as not improving the health of patients insured by it have any validity. (Let’s just say they are oversimplifications and distortions.)
The claims I’m about to address come from a place every bit as brain dead as the Food Babe in its own way and seem to have originated from an article on Forbes by someone named Paul Hsieh, who claims to “cover health care and economics from a free-market perspective.” Imagine my relief, because he sure doesn’t seem able to cover them from a science-based prospective. Behold his op-ed, Why The Federal Government Wants To Redefine The Word ‘Cancer’. The insinuation (although Hsieh is quick to deny that that’s what he’s really saying) is that the government wants to redefine cancer so that fewer patients will be diagnosed with cancer and qualify for treatment under Obamacare:
With respect to the definition of “cancer,” downgrading some conditions as no longer being “cancer” can and will used to justify reducing “unnecessary” screening tests (e.g., mammograms for women between ages 40-49). Mammograms can now detect the condition known as “ductal carcinoma in situ” (DCIS), which would no longer be called a cancer under the new proposal.
And, later:
I don’t believe the individual scientists arguing for a redefinition of cancer are driven by inappropriate political motives. But government will soon account for 66% of health spending and is aggressively seeking to limit health expenditures. Hence, the government may have a vested interest in definitions that err towards undertreatment, rather than overtreatment. We must remain vigilant against any attempts by the government to use language as a tool of covert rationing.
Imagine my further relief that Hsieh doesn’t think those of us who are interested in reducing overtreatment are twirling our moustaches and rubbing our hands with glee as we plot on “death panels” how to deny mom and grandma her mammograms to save money, all in the service of Obamacare. Not that I actually believe him. Or maybe he doesn’t believe that, but knows that the rubes who read his column do.
What Hsieh is referring to is an article published online in JAMA in July, and in the dead tree edition, by Laura J. Esserman, Ian M. Thompson, Jr., and Brian Reed entitled Overdiagnosis and Overtreatment in Cancer: An Opportunity for Improvement, a viewpoint report that was reported fairly widely in the media in Medscape, the New York Times, and NPR. The article, as I will discuss shortly, should not have been a surprise to anyone who regularly reads this blog or my writings at my not-so-super-secret other blog about overdiagnosis and overtreatment of cancer and the complexities of screening asymptomatic populations for cancers. As I’ve said time and time again, the relationship between early diagnosis and improvements in survival is complex and not nearly as clear-cut as most people, even most physicians, think. What Esserman et al. discussed as part of their summary of recommendations of a working group at the National Cancer Institute was simply the next logical step, recommending possible strategies to reign in overdiagnosis without compromising treatment of potentially life-threatening cancers. Their recommendations are reasonable and science-based, although likely to be at least somewhat controversial. Near the end of his piece, Hsieh quotes Dr. Milton Wolf, who says something that is so wrong on so many levels that one wishes it were possible to strip doctors of their medical licenses for spreading medical misinformation:
Health care rationing takes many insidious forms but perhaps the most immoral is for the government to wage a public relations campaign designed specifically to dissuade patients and doctors from seeking available cures for cancer. They scheme to rename cancer, not to cure it, but to deny it exists. These government rationers have calculated that rather than actually treat patients with cancer, it’s cheaper to simply keep them as calm as Hindu cows right up to the very end.
I’ve noticed that radiologists (for example, Dr. Daniel Kopans) seem to be the ones most opposed to any recommendation that involves decreasing screening intensity or frequency. One notes that Wolf is also a conservative Republican running for the Senate in Kansas who is in favor of defunding or repealing Obamacare. Ironically, he is also Barack Obama’s second cousin, who proudly proclaims, “I may not be the first doctor to oppose ObamaCare, but I am the first doctor from Barack Obama’s own family to oppose ObamaCare” and has even written an e-book entitled First, Do No Harm: The President’s Cousin Explains Why His Hippocratic Oath Requires Him to Oppose ObamaCare (Voices of the Tea Party). He’s also written articles with titles like The FDA’s one-man death panel and Tyranny in our time, criticizing his cousin and Obamacare. You get the idea.
Well, maybe you don’t. Hsieh and Dr. Wolf are downright reasonable in comparison to how the right wing blogosphere ran with this story. Here’s a sampling:
- “It is plain and simply rationing of health care. And, at some point, rationing becomes a death sentence. So, in the opinion of your humble observer of the asylum we all have to live in, the House Republicans should go back to their original proposal to defund ObamaCare and each time the Senate sends the bill back to the House, they should just change the date and return it to the Senate. Keeping the government in partial shut-down may be a godsend.” – Asylum Watch.
- “And why would the Obama administration want to re-define cancer? Because starting tomorrow, Obamacare will begin subsidizing millions of Americans’ health insurance, and cancer tests and treatments are expensive. This is nothing more than a back-door, roundabout form of rationing. It has nothing to do with improving health care or saving lives and everything to do with bureaucrats picking and choosing who gets what tests and treatments.” – Poor Richard’s News.
- “Aren’t we glad that crazy Sarah Palin lady with her death panel rants didn’t get elected. And instead we live with a wise and sane government that fights new wars while renaming them as interventions and cures cancer by renaming it and denying coverage? Hope. Change. Death.” – Daniel Greenfield, Frontpage Mag.
- “Cancer tests and treatment are expensive, and the government doesn’t want to foot the chemotherapy bill for lesions that don’t have a ‘reasonable likelihood of killing the patient.’ This redefining of the word cancer has absolutely nothing to do with improving healthcare, with saving lives, or with saving patients unnecessary anxiety; it is no more than an underhanded and surreptitious attempt at rationing. It is a cloak-and-dagger attempt to restrict who can benefit from healthcare system overpromised to us by Obama himself.’ – Crissy Brown, Thoughts on Liberty.
- “One of the great problems in allowing the government– especially one proven to be untrustworthy by a number of recent high-profile scandals– to run health care and judiciously dole treatments with an idea toward cost-saving, is that the truth becomes completely lost. Any sort of trust that is supposed to exist between patient and doctor is lost as doctors are required to redefine, to the point of untruth, diagnoses, treatment options, and future prognosis due to the federal legal requirements. It’s Orwellian and wrong. And it’s guaranteed by ObamaCare.” – Yukio Ngaby at the very much misnamed Critical Narrative.
- “The government wants to redefine the word “cancer” in order to have fewer conditions that can be classified as actual cancer. I’m going to go out on a limb here and ask…..do they really believe changing a couple of definitions is really going to help lessen the lives taken by cancer? I mean, if you paint a coconut pink it is still a coconut isn’t it?” – The Black Sheep Conservative.
I’m going to go out on a limb here (actually, no I’m not) and say bluntly that all of these criticisms demonstrate an astronomical level of ignorance about cancer that at its heart boils down to a conspiracy-minded belief that the government (via the NCI) wants to redefine cancer in order to not have to treat people with cancer and save money, no matter how many lives this costs. Of course, it never occurred to them that, given by definition overdiagnosis and overtreatment mean diagnosing cancer that will never threaten the life of the patient and treating such cancers unnecessarily, reducing overdiagnosis and overtreatment is a desirable goal, both from the standpoint of improving patient care (overtreatment is all risk, no benefit, after all) and decreasing costs. This is the problem with science-based guidelines rooted in new understandings of cancer biology. Reasonable recommendations about how to decrease the rate of overdiagnosis and overtreatment are immediately seized upon by activists. Unfortunately, as can be seen from Dr. Wolf’s likening of such recommendations to slaughtering cattle, a lot of physicians share in this ignorance. With that in mind, let’s look at what Esserman et al. actually wrote and recommended.
Redefining cancer: What it really means
I’ve discussed ductal carcinoma in situ (DCIS) before on multiple occasions. To recap, DCIS is a condition in which malignant-appearing ductal cells are observed in the milk ducts of the breast but have not yet invaded through the membrane surrounding the duct to get into the tissue outside of the duct. To put it simply, that’s basically what “in situ” means, that the cancerous cells have not yet invaded the basement membrane. There are quite a few epithelial cancers that have a carcinoma in situ stage: breast, colon, bladder, prostate, and others. In the breast, DCIS is generally considered “stage 0” cancer, and treatment has a very high success rate. The reason for this success is likely because a lot of DCIS, possibly even most DCIS, never progresses to invasive cancer or progresses so slowly that the women who have it die of something else (such as old age) before it ever causes a problem. Indeed, it is estimated that low grade DCIS, if it progresses, does so within a time frame of 5 to 40 years and possibly in only 20% of DCIS cases, while high grade DCIS is more likely to progress. The same sort of behavior occurs with a lot of early stage prostate cancer in men. Since I’m a breast cancer surgeon, most of my examples will come from breast cancer. In other words, premalignant lesions are not one disease, and many of them will never cause harm within the remaining lifetime of the person harboring them.
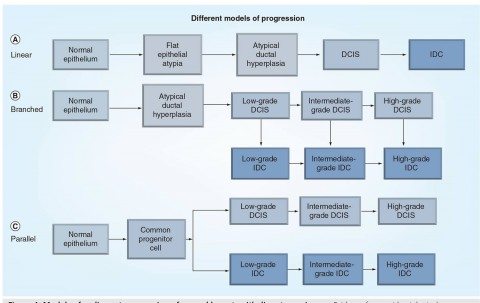
The fact is that before the advent of widespread mammographic screening, DCIS was a relatively uncommon diagnosis. Now, thirty years or so after mass mammographic screening programs became widespread, DCIS is common. Indeed, approximately 40% of breast cancer diagnoses are in fact DCIS. A recent study found that DCIS incidence rose from 1.87 per 100,000 in the mid-1970s to 32.5 in 2004. That’s a more than 16-fold increase over 30 years, and it’s pretty much all due to the introduction of mammographic screening of asymptomatic women. One potential reason is that by the time DCIS progresses to the point of being detectable by means other than mammography (such as feeling a breast mass), it has usually progressed to invasive ductal cancer. Another potential reason is that much of the DCIS we detect by mammography doesn’t progress to become symptomatic and threaten the life of the woman. Probably both mechanisms are in play. Either way, we don’t know for sure what percentage of DCIS lesions progress to cancer, and, in fact, we don’t know for sure whether the progression from normal ductal cells to cancer necessarily goes through DCIS. (Yes, I am a co-author on this paper and helped with much of the clinical discussion.) Indeed, there are currently three main models, all of which might contribute in different specific cases of DCIS, for how infiltrating ductal cancer (IDC) arises:
Supporting the hypothesis that something more than just a straight linear model of breast cancer progression is most in line with how breast cancer develops is the observation that, although the diagnosis of breast cancer has very much slanted much more towards DCIS and early stage (stage I and II) cancers over the last 30 years, detecting and treating these cancers aggressively has not resulted in a proportionate decrease in metastatic and locally advanced cancers. This was reported in the New England Journal of Medicine last December and is in line with other studies that I’ve mentioned finding that one in three breast cancers diagnosed by mammographic screening could be overdiagnosed and that one in five might spontaneously regress without treatment. Indeed, it’s becoming increasingly apparent that even a subset of frankly invasive cancers either don’t progress, progress so slowly that they won’t cause harm, or even regress. Treating these lesions provides no benefit to women, but does produce risk. In other words, these lesions (in this case, DCIS) that we refer to as “cancer” might better be considered something else, as many of them might not behave like cancer at all, at least not if defined as if untreated, inevitably progressing into a cancer that will threaten a woman’s life within her natural lifespan. Some are likely to be very indolent; some might even regress.
Who wouldn’t want to reduce the number of patients who are overtreated, and who wouldn’t want to name these premalignant, possibly malignant, conditions more accurately? Although part of this debate does have something to do with decreasing costs, contrary to what the fractally wrong quotes above more than insinuate, the primary reason is to decrease the number of patients subjected to potentially toxic therapies like radiation, surgery, and even chemotherapy for lesions that would cause no harm in their lifetime. The problem, as I’ve pointed out time and time again, is that we don’t yet know how to distinguish the in situ and early invasive cancers that are harmless from the ones that will progress. Until we can do that, we as physicians feel obligated to treat all of them aggressively.
With this background in mind, the recommendations by Esserman et al. seem downright reasonable, mainly because they are downright reasonable, beginning with the introduction:
Over the past 30 years, awareness and screening have led to an emphasis on early diagnosis of cancer. Although the goals of these efforts were to reduce the rate of late-stage disease and decrease cancer mortality, secular trends and clinical trials suggest that these goals have not been met; national data demonstrate significant increases in early-stage disease, without a proportional decline in later-stage disease. What has emerged has been an appreciation of the complexity of the pathologic condition called cancer. The word “cancer” often invokes the specter of an inexorably lethal process; however, cancers are heterogeneous and can follow multiple paths, not all of which progress to metastases and death, and include indolent disease that causes no harm during the patient’s lifetime. Better biology alone can explain better outcomes. Although this complexity complicates the goal of early diagnosis, its recognition provides an opportunity to adapt cancer screening with a focus on identifying and treating those conditions most likely associated with morbidity and mortality.
Changes in cancer incidence and mortality reveal three patterns that emerged after inception of screening (Table). Screening for breast cancer and prostate cancer appears to detect more cancers that are potentially clinically insignificant. Lung cancer may follow this pattern if high-risk screening is adopted. Barrett esophagus and ductal carcinoma of the breast are examples for which the detection and removal of lesions considered precancerous have not led to lower incidence of invasive cancer. In contrast, colon and cervical cancer are examples of effective screening programs in which early detection and removal of precancerous lesions have reduced incidence as well as late-stage disease. Thyroid cancers and melanoma are examples for which screening has expanded and, along with it, the detection of indolent disease.
All of which is basically what I’ve been saying, with the addition of the examples of cervical and colorectal cancer, which do appear to behave in a manner consistent with a more linear progression model, which means that removing early stage disease does effectively prevent the appearance of late stage disease. Based on these observations, here is what the NCI recommends, with my comment afterward
- Physicians, patients, and the general public must recognize that overdiagnosis is common and occurs more frequently with cancer screening. [Note: This is nothing that I haven’t been saying for at least four years now, ever since I started to appreciate the complexities of screening for cancer.]
- Change cancer terminology based on companion diagnostics. Use of the term “cancer” should be reserved for describing lesions with a reasonable likelihood of lethal progression if left untreated. There are two opportunities for change. First, premalignant conditions (eg, ductal carcinoma in situ or high-grade prostatic intraepithelial neoplasia) should not be labeled as cancers or neoplasia, nor should the word “cancer” be in the name. Second, molecular diagnostic tools that identify indolent or low-risk lesions need to be adopted and validated. Another step is to reclassify such cancers as IDLE (indolent lesions of epithelial origin) conditions. [Note: Again, if you understand the more recent data with respect to screening certain cancers, none of this is an attempt by the evil government to withhold vital care from cancer patients. It is actually an attempt to improve the care of cancer patients by decreasing overdiagnosis and more carefully “personalizing”—if you’ll excuse the use of this overused term—care to the patient’s tumor.]
- Create observational registries for low malignant potential lesions. Providing patients and clinicians with pathologic diagnosis and information related to disease prognosis is crucial to informed decision making, including comfort with alternate treatment strategies such as active surveillance. [Note: Again, if we are truly going to “personalize” the treatment of lesions of low malignant potential, we need better information about what percentage of them progress into life-threatening malignancy and over what time frame they do so in order to facilitate shared decision-making between physician and patient. Again, this is not withholding treatment; this is empowering patients based on scientific findings to make decisions regarding their care with which they are comfortable.]
- Mitigate overdiagnosis. Strategies to reduce detection of indolent disease include reducing low-yield diagnostic evaluations appropriately, reducing frequency of screening examinations, focusing screening on high-risk populations, raising thresholds for recall and biopsy, and testing the safety and efficacy of risk-based screening approaches to improve selection of patients for cancer screening. [Note: Again, this is nothing that I haven’t discussed in depth many times, beginning with the USPSTF recommendations for mammography. Unfortunately, any attempt to decrease screening inevitably runs into criticism that we’ll be “killing patients,” because the idea that premalignant diseases inevitably progress to life-threatening cancer is deeply embedded not only in the popular concept of cancer, but in the medical profession itself. Indeed, physicians even go so far as to erroneously blame the New York Times for killing patients by publicizing the problems with screening tests for cancer, like PSA testing.]
- Expand the concept of how to approach cancer progression. Future research should include controlling the environment in which precancerous and cancerous conditions arise, as an alternative to surgical excision. [Note: I must admit that this one left me scratching my head a bit. What, specifically, does this mean in practice? I must admit that I don’t know.]
Esserman et al. conclude by pointing out that much of this is an issue of communication as much as it is of science. After all, for the last 30-40 years, the medical profession and public health officials have been drumming it into our heads that we have to catch cancer early and that screening tests are the best way to do it, without also pointing out that every medical tests have risks and benefits. Yes, catching cancer early tends to be better in many ways. Treatment is more likely to be successful (or at least appear so) and, in the case of many cancers, can be achieved with much less aggressive and disfiguring surgeries. In my field, the example of doing a lumpectomy compared to being forced to do a mastectomy comes to mind. However, much more difficult is explaining how much of that improved survival is due to lead time bias and how much is due to treatment and early detection (as I’ve discussed here, here, here, and here). It’s also hard to include in such discussions the concept of length bias, in which most cancer screening tests are biased towards detecting slower-growing, more indolent disease. As I’ve discussed before as well, to avert one death from breast cancer with mammographic screening for women between the ages of 50-70, 838 women need to be screened over 6 years for a total of 5,866 screening visits, to detect 18 invasive cancers and 6 instances of DCIS. The additional price of this was estimated to be 90 biopsies and 535 recalls for additional imaging, as well as many cancers treated as if they were life threatening when they are not. To prevent one death from prostate cancer, 1,410 men need to be screened over 9 years, for a total of 2,397 screening visits and 48 cancers detected. In other words, screening takes a lot of effort for, on an absolute basis, not as many lives saved as most people, even doctors, believe.
When taken in this context, all Esserman et al. are saying is that we need to screen smarter, not more, and that we need to adjust our terminology and treatments to be more in line with our more recent understanding of biology. As Dr. Otis Brawley, chief medical officer of the American Cancer Society, put it so aptly, “We need a 21st-century definition of cancer instead of a 19th-century definition of cancer, which is what we’ve been using.” He’s right. Most of our definitions of carcinoma, carcinoma in situ, and premalignant conditions date back over 100 years and were based largely on what could be observed about tumors under the microscope. In 2013, we now have the tools to probe the molecular pathways that define and drive the progression of cancer.
Conclusions: Cancer is scary
There is actually one point that the cranks attacking the recommendations of the NCI panel make that has some validity, just not in the way that they think it does. That point is that words have power, and the word “cancer” has particular power. Of course, the cranks think that the reason the NCI is suggesting ceasing to use the word “cancer” to describe conditions that appear cancerous using old criteria but are not likely to harm patients who have them, is to deceive patients and doctors into accepting less care in order to save money. In reality, it is a plea to bring language more into line with new science, based on concern among doctors that “hundreds of thousands of men and women are undergoing needless and sometimes disfiguring and harmful treatments for premalignant and cancerous lesions that are so slow growing they are unlikely to ever cause harm.” At the same time, we do not want to go too far in the opposite direction and err on the side of undertreatment.
Frequently referenced in discussions of the NCI recommendations is another study that I had meant to blog about when it first came out but got distracted by my Dug the Dog tendencies. (It came out about the same time the NCI recommendations saw print.) This study by Omer et al. examined the effect of how DCIS is described on the treatment choices of women. In the study, 394 women without a history of breast cancer were presented with three scenarios that described ductal carcinoma in situ (DCIS) as noninvasive breast cancer, breast lesion, or abnormal cells. They were then asked to choose among three treatment options: surgery, medication, or active surveillance. When DCIS was described as noninvasive cancer, 53% favored nonsurgical options. However, 63% chose nonsurgical options when the term used was breast lesion, a number that rose to 69% when the term used was abnormal cells. The authors concluded:
We conclude that the terminology used to describe DCIS has a significant and important impact on patients’ perceptions of treatment alternatives. Health care providers who use ‘cancer’ to describe DCIS must be particularly assiduous in ensuring that patients understand the important distinctions between DCIS and invasive cancer.
Or, as Ian Thompson put it:
“That is the real world of this when you include the word ‘cancer,’” Dr. Thompson said. “Because the word ‘cancer’ has a connotation that is profoundly bad.” The word “precancerous” has that same connotation. “That means the shoe is going to drop sometime down the road and that you are irresponsible if you don’t do anything about it,” he continued.
The consequences of the use of the word “cancer” to describe conditions that are only somewhat likely to progress can be seen all around us. For instance, the NPR article on the NCI recommendations tells the story of a 42-year-old woman who was diagnosed with DCIS and decided that she wanted a double mastectomy. In fact, I was shocked to learn that 6% of women with DCIS opt to undergo double mastectomy, which is massive overkill for such lesions that will not decrease the risk of dying of breast cancer. The consequences are found in women with DCIS being pressured by well-meaning doctors to have surgery right away, as if DCIS will turn into cancer overnight if they don’t act. It won’t.
In the end, dealing with premalignant lesions comes down to three things. First, we desperately need more accurate methods of risk assessment that allow us to accurately predict the likelihood that a given lesion will progress into cancer. Second, we have to get rid of the mindset that all precancerous lesions will inevitably “turn into” cancer. They won’t, and which ones are dangerous depends on the cancer type, observable characteristics such as nuclear grade, and molecular characteristics that we haven’t dissected yet. Finally, it’s a matter of communication. Telling people that finding cancer early is always better, that precancerous lesions found by screening will inevitably kill them if they don’t act, is based on an understanding of cancer progression that is decades old and no longer appropriate given the knowledge accumulated over the last two decades. It might be a cliché, but we need to screen smarter, not more, and we need to be able to explain that not all premalignant lesions require aggressive treatment.
It’s not going to be easy to change this culture and mindset, though, not the least of which because cynical pundits like Paul Hsieh and Mark Wolf are trying to convince people for their own political purposes that any effort to decrease screening, or more accurately describe premalignant lesions that are unlikely to cause harm, is somehow wanting to let cancer patients die in order to save money.