[Editor’s note: This is the full version of the post from yesterday, with a much more comprehensive examination of infectious diseases that Humphries illogically compares with polio. Note that a downloadable PDF version of complete paper, including a detailed reference list, can be accessed here.]
Suzanne Humphries, MD and Roman Bystrianyk (2013). “Dissolving Illusions: Disease, Vaccines. and the Forgotten History.” CreateSpace Independent Publishing Platform.
[Note that I refer often to Wikipedia articles. I do this because they are easily available, accurate based on my other readings, and include extensive reference lists that I have checked out. However, as the reader will find, I also include numerous other references.]

Introduction
From early childhood, though enjoying Sherlock Holmes, H.G. Wells, Jules Verne, and other works of fiction, I especially liked reading history and science, subscribing to the old adage that “truth is stranger than fiction.” Then I read a book that had a profound effect on me, William H. McNeil’s 1976 Plagues and Peoples. McNeil made a compelling case that much of human history has been determined not by great statesmen, nor military leaders, nor technology; but by the lowly microbe. In the subsequent 40 years, I have read dozens of books and hundreds of articles on each of the various infectious diseases from plague to smallpox to influenza to polio, numerous histories of each, their current status around the world, and, of course, their epidemiology. Along the way I did graduate work in epidemiology, and biostatistics, read numerous textbooks and articles, and audited courses on microbiology and immunology.
Though a long proponent of vaccines, only over the past five years have I focused on mainly writing articles supporting them (Harrison, 2017, Harrison, 2018). I was driven to do so in response to what seems to be an ever-increasing noise and misinformation on vaccine safety and efficacy from anti-vaccinationist groups and web blogs. Since beginning of my writings on vaccines I have contemplated writing on polio. This is not only because polio seems to be one of the antivaccinationist favorite topics, which they often use to demonstrate to their uninformed readers the evils of vaccines and national vaccination programs (e.g., Adams. 2018; Child Health Safety, 2018; Olmsted, 2011, Olmsted, 2016; VacTruth, 2018; whale to, 2018); but also because polio has a special significance for me. As a child I remember my mother not allowing me to go to the local municipal swimming pool nor to the movies during polio season. In my elementary school was a little girl with a steel brace on one leg. During my life I have known several paraplegics, one, in particular, the older sister of one of my oldest andd dearest friends, met a man in the late 1980s who had been in an iron lung for almost 40 years, and several people who suffered from post-polio syndrome. And through my readings I discovered that my hometown, San Diego, had a major epidemic of polio in 1951 and being in the first cohort to receive the new Salk vaccine, I more than likely received a dose from a lot manufactured by Cutter Industries which because of poor production and quality control caused 204 cases of paralytic polio and 10 deaths (to be discussed in a later paper). So, fortunately, I dodged at least two bullets.
I am focusing on Humphries and Bystrianyk’s book for two reasons:
- Their chapter on polio, “Chapter 12. The ‘Disappearance’ of Polio”, pp. 210-261, as far as I can tell, covers each and every claim/assertion made by antivaccinationists together with a large reference list;
- Suzanne Humphries is a medical doctor. Most antivaccinationist articles that I have come across are written by people with little to no background in medicine or any of the other subjects relevant to vaccines, e.g., microbiology, immunology, epidemiology, etc. As a medical doctor one would expect that Humphries has had the basics of the aforementioned subjects and her expertise as an MD, perhaps, has had a greater impact than her antivaccine peers.
In this paper quotes from Humphries and Bystrianyk’s book will be referenced as “(Humphries, p. __).” Note that Humphries uses extensive quotes in her book, so I will do the same.
Unfortunate incidents and avoidable errors do occur, but these rare events should not be the basis on which to decide the merit of things like public health programs, as some, including Suzanne Humphries and Roman Bystrianyk in their book Dissolving Illusions, have attempted. Even more egregious is the attempt to take a monumentally significant public health issue like polio and, using “alternative facts”, minimize its significance. In Humphries’ and Bystrianyk’s book, the subject of this article, they even go so far as to claim that polio was an “insignificant” disease.
Incidence, mortality, disability, suffering: Comparing apples to oranges
From Humphries:
Prevalence of polio, 1912–1969
Since the early 1900s, we have been indoctrinated to believe that polio was a highly prevalent and contagious disease. Graph 12.1 depicts the incidence of various diseases in the United States between 1912 and 1970. Poliomyelitis is the line (with square points) at the bottom and reveals that the incidence was very low when compared to that of other infectious diseases. Polio has also been portrayed as a vicious crippler in the early and mid-1900s when it was habitually diagnosed by doctors who used a very loose definition of the disease. This graph denotes rates of clinical disease, most of which resolved and left no residual paralysis at all.
Given what a low-incidence disease it was, how did polio come to be perceived as such an infamous monster? This is a question worthy of consideration, especially in light of the fact that the rate was far less than other common diseases, some of which declined in incidence to nearly zero with no vaccine at all. Those who still embody a fear of polio may argue that it was a monster because it crippled people, especially children. But it was later revealed, after a vaccine was lauded for the eradication of polio, that much of the crippling was related to factors other than poliovirus, and those factors could not possibly have been affected by any vaccine (pp. 212-213).
Graph 12.1 referenced in the quote above is copied below as Figure 1. Note, that as the graph appears in her book, it is difficult to discern by color which of the lines represent which disease, so I have included a red arrow to indicate the line representing poliomyelitis. The data Humphries used to produce this graph is in Table 1 below Figure 1.
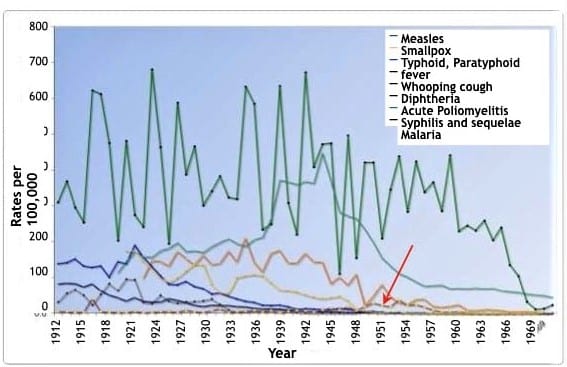
Figure 1: United States disease incidence from 1912 to 1970 (Graph 12.1 in Humphries, 2013, p. 215)
Table 1: Rates Per 100,000 Population for Specified Reportable Diseases: 1912 to 1970. Historical Statistics of the United States: Colonial Times to 1970, Part 1. Bureau of the Census (1970), p. 77.
| Year | Disease incidence per 100,000 population | |||||||
| Syphillis | Malaria | Typhoid | Diptheria | Pertussis | Measles | Poliomyleitis | Smallpox | |
| 1970 | 43.8 | 1.5 | 0.2 | 0.2 | 2.1 | 23.2 | <0.5 | |
| 1969 | 48.1 | 1.5 | 0.2 | 0.1 | 1.6 | 12.8 | <0.5 | |
| 1968 | 49.9 | 1.2 | 0.2 | 0.1 | 2 .4 | 11.l | <0.5 | |
| 1967 | 53.2 | 1.0 | 0.2 | 0.1 | 4 .9 | 31.7 | <0.5 | |
| 1966 | 57.1 | 0.3 | 0.2 | 0.1 | 3.9 | 104.2 | 0.1 | |
| 1965 | 59.7 | 0.1 | 0.2 | 0.1 | 3.5 | 135.1 | <0.5 | |
| 1964 | 62 .9 | <0.5 | 0.3 | 0.2 | 6.8 | 239.4 | 0.1 | |
| 1963 | 69.8 | 0.1 | 0.3 | 0.2 | 9.1 | 204.2 | 0.2 | |
| 1962 | 68.1 | 0.1 | 0.3 | 0.2 | 9.6 | 259.0 | 0.5 | |
| 1961 | 69.7 | <0.5 | 0.4 | 0.3 | 6.3 | 231.6 | 0.7 | |
| 1960 | 68.0 | <0.5 | 0.5 | 0.5 | 8.3 | 245.4 | 1.8 | |
| 1959 | 69.3 | <0.5 | 0.5 | 0.5 | 22.7 | 230.1 | 4.8 | |
| 1958 | 68.5 | <0.5 | 0.6 | 0.5 | 18.6 | 440.5 | 8.3 | |
| 1957 | 78.8 | 0.1 | 0.7 | 0.7 | 16.6 | 285.9 | 3.2 | |
| 1956 | 77.1 | 0.1 | 1.0 | 0.9 | 19.0 | 865.9 | 9.1 | |
| 1955 | 76.0 | 0.3 | 1.0 | 1.2 | 38.2 | 337.9 | 17.6 | |
| 1954 | 87.5 | 0.4 | 1.3 | 1.3 | 37.8 | 423.5 | 23.9 | |
| 1953 | 100.8 | 0.8 | 1.4 | 1.5 | 23.5 | 283.7 | 22.5 | |
| 1952 | 110.8 | 4.5 | 1.5 | 1.9 | 28.9 | 438.5 | 87.2 | |
| 1951 | 131.8 | 3.7 | 1.4 | 2.6 | 44.8 | 345.6 | 18.5 | |
| 1950 | 154.2 | 1.4 | 1.6 | 3.8 | 80.1 | 210.1 | 22.1 | |
| 1949 | 197.3 | 2 .8 | 2.7 | 5.4 | 46.7 | 420.6 | 28.3 | <0.5 |
| 1948 | 234.7 | 6 .6 | 2.5 | 6 .5 | 51.1 | 421.0 | 19.0 | <0.5 |
| 1947 | 264.6 | 10.5 | 2.8 | 8.5 | 109.1 | 155.0 | 7.5 | 0.1 |
| 1946 | 271.7 | 34.7 | 2.8 | 11.7 | 78.4 | 496 .8 | 18.3 | 0.2 |
| 1945 | 282.3 | 47 .4 | 3.7 | 14.1 | 101.0 | 110.2 | 10.3 | 0.3 |
| 1944 | 867 .9 | 43.4 | 4.0 | 10.6 | 82.7 | 474.3 | 14.3 | 0.3 |
| 1943 | 447 .0 | 40.6 | 4.1 | 11.0 | 142 .9 | 472.0 | 9.3 | 0.6 |
| 1942 | 363.4 | 44.9 | 4.6 | 12.1 | 142.9 | 408.8 | 8.1 | 0.6 |
| 1941 | 368.2 | 51.1 | 6.5 | 13.5 | 166.9 | 671.7 | 6.8 | 1.0 |
| 1940 | 359.7 | 59 .2 | 7.4 | 11.8 | 139.6 | 220.7 | 7 .4 | 2.1 |
| 1939 | 367 .1 | 63.2 | 10.0 | 18.4 | 140.0 | 308.2 | 5.6 | 7.5 |
| 1938 | 372.0 | 64.9 | 11.5 | 23.5 | 175.1 | 633.8 | 1.3 | 11.5 |
| 1937 | 264.8 | 84.2 | 12.4 | 22 .2 | 166.6 | 249.6 | 7 .4 | 9.1 |
| 1936 | 212.6 | 104.6 | 12.4 | 23.4 | 115.0 | 284.0 | 3.5 | 6.1 |
| 1935 | 205.6 | 108.1 | 14.4 | 30.8 | 141.9 | 584.6 | 8.5 | 6.8 |
| 1934 | 186.7 | 105.4 | 17.6 | 34.1 | 209.9 | 632.6 | 5.9 | 4.8 |
| 1933 | 193.4 | 100.0 | 18.6 | 40.2 | 142.6 | 319.2 | 4.0 | 5.2 |
| 1932 | 208.2 | 55.0 | 21.4 | 48.0 | 172.5 | 323.2 | 3.1 | 9.0 |
| 1931 | 197 .4 | 56.7 | 21.4 | 57.1 | 139.l | 382.8 | 12.8 | 24.4 |
| 1930 | 185.4 | 80.0 | 22.1 | 54.1 | 135.6 | 340.8 | 7.5 | 39.7 |
| 1929 | 169.2 | 134.7 | 19.1 | 70.1 | 162.l | 300.6 | 2.4 | 34.7 |
| 1928 | 174.2 | 138.2 | 22.6 | 75.9 | 134.3 | 466.3 | 4.3 | 32.7 |
| 1927 | 171.9 | 118.2 | 29.2 | 89.8 | 152.4 | 387.6 | 8.8 | 31.6 |
| 1926 | 196 .1 | 98.9 | 35.5 | 80.7 | 172.2 | 587.1 | 2.3 | 28.7 |
| 1925 | 181.2 | 86.8 | 40.0 | 82.1 | 131.2 | 194.3 | 5.3 | 84.2 |
| 1924 | 174 .2 | 98.4 | 31.0 | 105.6 | 145.0 | 463.7 | 4.6 | 49.6 |
| 1923 | 156 .2 | 124.2 | 31.0 | 131.4 | 146.7 | 680.0 | 3.1 | 27 .6 |
| 1922 | 157 .7 | 142.9 | 33.0 | 156 .9 | 97.7 | 241.8 | 2.0 | 30.8 |
| 1921 | 172.3 | 174 .7 | 43.5 | 190.7 | 274.6 | 5.8 | 94.7 | |
| 1920 | 145.3 | 173.0 | 33.8 | 139.0 | 480.5 | 2.2 | 95.9 | |
| 1919 | 113 .2 | 42.9 | 144.7 | 203.2 | 2.8 | 68.8 | ||
| 1918 | 50.0 | 101.5 | 474.9 | 2.8 | 83.1 | |||
| 1917 | 63.0 | 183.0 | 611.6 | 4.9 | 52.7 | |||
| 1916 | 82.3 | 129.2 | 621.8 | 41.1 | 23.4 | |||
| 1915 | 74.0 | 132.7 | 254.1 | 8.1 | 50.2 | |||
| 1914 | 82.4 | 152.5 | 295.8 | 2.4 | 66.4 | |||
| 1913 | 84.2 | 142.1 | 368.5 | 4.0 | 55.7 | |||
| 1912 | 81.8 | 139.0 | 310.0 | 5.5 | 30.8 | |||
Note that between years 1944 through 1955 (BOLDED) poliomyelitis incidence can be more clearly seen as increasing than appears in Figure 1 (dashed line indicated by arrow). However, it is not the incidence of a disease that is most relevant, otherwise all the diseases included in Humphries graph pale compared to the common cold and even food poisoning, which an estimated 1 in 6 Americans (48 million people) get every year, resulting in 128,000 hospitalizations, and 3,000 deaths (CDC. Burden of Foodborne Illnesses). What is important are:
- Degree of suffering
- Disability
- Mortality
- Mode of transmission
- Factors affecting the above (e.g., public health measures)
The main focus of this paper is Humphries claim that polio was an “insignificant” disease. However, given that her book covers each of the diseases compared in Figure 1, the following will give a description of each based on the five points listed above, allowing the reader to gain a better picture of each disease, why Humphries is comparing apples to oranges, and, especially how, by focusing on incidence and death, Humphries mostly ignores suffering and disabilities. Besides polio, measles is a prime example of this. Though I believe the following description of each of the diseases is well worth a look, feel free to skip to the Poliomyelitis section below.
Measles
According to Wikipedia:
Measles is a highly contagious infectious disease caused by the measles virus. Symptoms usually develop 10–12 days after exposure to an infected person and last 7–10 days. Initial symptoms typically include fever, often greater than 40 °C (104.0 °F), cough, runny nose, and inflamed eyes. Small white spots known as Koplik’s spots may form inside the mouth two or three days after the start of symptoms. A red, flat rash which usually starts on the face and then spreads to the rest of the body typically begins three to five days after the start of symptoms. Complications occur in about 30% of cases and may include diarrhea, blindness, inflammation of the brain, and pneumonia, among others.
Measles is an airborne disease which spreads easily through the coughs and sneezes of infected people. It may also be spread through contact with saliva or nasal secretions.
People are infectious to others from four days before to four days after the start of the rash.
In May 2015, the journal Science, published a report in which researchers found that the measles infection can leave a population at increased risk for mortality from other diseases for two to three years. (Wikipedia. Measles; see also: CDC. Pink Book. Measles; Cliff, 1993; Mina, 2015; Perry, 2004; Strebel, 2018)
The CDC Pink Book’s Chapter on Measles gives the following statistics:
Before 1963, approximately 500,000 cases and 500 deaths were reported annually, with epidemic cycles every 2–3 years. However, the actual number of cases was estimated at 3–4 million annually. More than 50% of persons had measles by age 6, and more than 90% had measles by age 15. The highest incidence was among 5–9-year-olds, who generally accounted for more than 50% of reported cases. In the years following licensure of vaccine in 1963, the incidence of measles decreased by more than 95%, and 2–3-year epidemic cycles no longer occurred…Some form of residual neurologic damage occurs in as many as 25% of cases [including loss of hearing, seizure disorders, and mental retardation…(CDC. Pink Book. Measles). [thus, up to 250 cases with permanent disabilities]
And from the CDC website on measles:
About one child out of every 1,000 who get measles will develop encephalitis (swelling of the brain) that can lead to convulsions and can leave the child deaf or with intellectual disability (CDC. Measles).
And according to Orenstein:
By the late 1950s, even before the introduction of measles vaccine, measles-related deaths and case fatality rates in the United States had decreased markedly, presumably as a result of improvement in health care and nutrition. From 1956 to 1960, an average of 450 measles-related deaths were reported each year (∼1 death/1000 reported cases), compared with an average of 5,300 measles-related deaths during 1912–1916 (26 deaths/1000 reported cases). Nevertheless, in the late 1950s, serious complications due to measles remained frequent and costly. As a result of measles virus infections, an average of 150,000 patients had respiratory complications and 4,000 patients had encephalitis each year; the latter was associated with a high risk of neurological sequelae and death. These complications and others resulted in an estimated 48,000 persons with measles being hospitalized every year (Orenstein, 2004; see also: Roush, 2007).
Langmuir writes:
Note the stability of the morbidity and the steady downward trend in the mortality. Also, there is the somewhat ominous suggestion of a cessation of this downward trend since 1955 similar to the leveling off of the infant death rates during the past six years. (Langmuir, 1962).[Note that if one looks at Figure 2 below the deaths fluctuate from 1953-1960 within a range, so one should not rely on a single year’s stats]
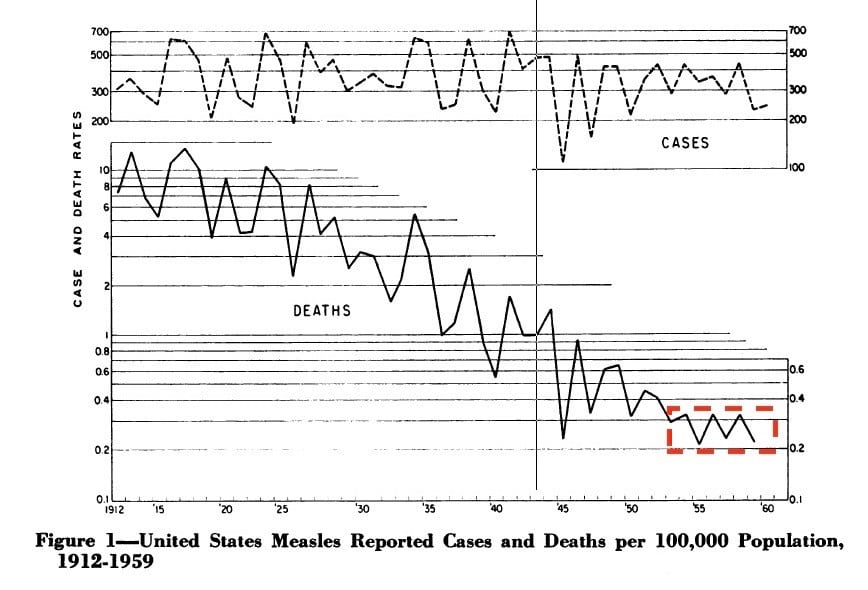
Figure 2: United States Measles Reported Cases and Deaths per 100,000 Population, 1912-1959 (from Langmuir, 1962, Figure 1).
Humphries writes:
In the case of measles, the death rate had declined by almost 100 percent. You would never know it today, but the dreaded measles was no longer a major issue in the Western world by the time vaccines were deployed (p.174)
And:
…deaths from asthma were 56 times greater, accidents 935 times greater, motor vehicle accidents 323 times greater, other accidents 612 times greater, and heart disease 9,560 times greater (p. 308).
Talk about comparing apples to oranges. Almost all measles deaths are in children, the overwhelming majority with heart disease in middle aged and older adults. And motor vehicle accidents? I’m surprised Humphries didn’t just list the high death rate in those over 65, or murder victims. Maybe in a new edition of her book? As will be clear from my discussion below, the causes, and approaches to prevention, of Humphries hodgepodge of incidence and deaths differ significantly, that is, they are NOT comparable.
Humphries downplays not only deaths; but acute suffering and long-term disabilities. In the case of measles, she discounts an average of 450 deaths per year in the U.S. (even if these were eliminated, the following remains), the 7-10 days suffering, possible diarrhea, otitis media, and seizures, given > 50% of cases were in 5-9 year-olds, their missing up to two weeks of school, the estimated 48,000 hospitalizations, and permanent disabilities. In addition, given that nowadays approximately 60% of families are dual income households, one of the parents would more than likely have to stay home to take care of the child for up to two weeks (Pew Research Center, 2015). As only about 14% have access to paid family leave, for many, a child ill with measles can also represent a substantial financial burden (DeSilver, 2017). Humphries seems unaware of how measles weakens our immune systems, increasing the mortality risk for 2-3 years afterwards (Mina, 2015). Finally, given that the estimated number of cases per year in the U.S. was 3-4 million annually, the actual number of deaths and persons with measles-associated disabilities may have been substantially higher due to under-reporting or misdiagnosis (CDC. Pink Book. Measles). For instance, if a child developed secondary bacteria pneumonia, the death record may only list pneumonia.
Smallpox
According to Wikipedia:
The initial symptoms of the disease include fever and vomiting. This is then followed by formation of sores in the mouth and a skin rash. Transmission occurs through inhalation of airborne variola virus, usually droplets expressed from the oral, nasal, or pharyngeal mucosa of an infected person. It is transmitted from one person to another primarily through prolonged face-to-face contact with an infected person, usually within a distance of 6 feet (1.8 m), but can also be spread through direct contact with infected bodily fluids or contaminated objects (fomites) such as bedding or clothing. Rarely, smallpox has been spread by virus carried in the air in enclosed settings such as buildings, buses, and trains…Smallpox is not notably infectious in the prodromal period and viral shedding is usually delayed until the appearance of the rash, which is often accompanied by lesions in the mouth and pharynx. The virus can be transmitted throughout the course of the illness, but is most frequent during the first week of the rash, when most of the skin lesions are intact. Infectivity wanes in 7 to 10 days when scabs form over the lesions, but the infected person is contagious until the last smallpox scab falls off.
Smallpox is highly contagious, but generally spreads more slowly and less widely than some other viral diseases, perhaps because transmission requires close contact and occurs after the onset of the rash. The overall rate of infection is also affected by the short duration of the infectious stage. In temperate areas, the number of smallpox infections were highest during the winter and spring (Wikipedia. Smallpox; see also: CDC. Smallpox; Dixon, 1962; Fenner, 1988; Kennedy, 2018).
Variola Major vs Variola Minor (Alastrim)
According to Fenner: “Two clinico-epidemiological varieties of smallpox were recognized: variola major (case-fatality rates, 5-40%) and variola minor (case-fatality rates, 0.1-2%) (Fenner, 1988, p. 96; see also: Chapin, 1913; Chapin, 1932).” Note that the American version of variola minor is also called alastrim. Besides variola major’s exponentially higher mortality, blindness and/or severe disfigurement from pockmarks often occurred.
Other complications:
Complications of smallpox [variola major] include bacterial infections of the skin and other organs, pneumonia, generalized sepsis, destructive arthritis in young children and arthropathies, corneal ulceration resulting in blindness, keratitis, osteomyelitis, and encephalitis. The latter, present in approximately 1 in 500 cases (Kennedy, 2018, p.1003).
According to Fenner:
Patients with variola major usually excreted more virus and were thus more infectious than patients with variola minor, and variola major was more likely to overcome the effects of slight residual immunity due to vaccination. On the other hand, the severity of systemic symptoms from the prodromal stage onwards was so great in variola major that most patients were confined to bed and thus their contacts were greatly limited. Patients with variola minor usually had such a mild systemic illness that they were often ambulant throughout the course of the disease, and therefore made many more close contacts (Fenner, 1988, p. 317).
Fenner continues with:
Variola major prevailed throughout the USA until the summer of 1897 but by then had disappeared from the country except for about 100 cases, with 30 deaths, which occurred in 16 different states.
The substrain of variola minor that was later called “alastrim” (see Chapter 2) remained the dominant form of smallpox in the USA thereafter.
Although some cases of variola major were reported every year from 1900 until 1927, there were only 2 major outbreaks during this period. The first, in 1902-1903, affected particularly Boston, New York, Philadelphia, New Jersey and Ohio; variola minor was then prevalent in the Mid-West. The last large epidemic of variola major in the USA occurred in 1924-1925, when some 7400 cases were reported, over one-third of them in 4 cities: Cleveland and Toledo (Ohio), Detroit (Michigan) and Pittsburgh (Pennsylvania).
Vaccination played an important role in both the progressive fall in the incidence of smallpox and in the replacement of variola major by variola minor.
In the year 1927, for the first time, no case of variola major was reported in the USA, and apart from an outbreak in 1929 no further cases were notified until 1946. In that year a soldier returning from Japan introduced smallpox into Seattle, Washington, which resulted in an outbreak of 51 cases, with 16 deaths (Palmquist, 1947). In 1947 a man with undiagnosed haemorrhagic smallpox died in a Manhattan, New York, hospital. Twelve other persons were infected.
The last outbreak of smallpox in the USA occurred in Texas in 1949 (8 cases with 1 death), probably after importation from Mexico. (Fenner, 1988, pp. 328-33)
Thus, mortality in the United States did decrease exponentially in the 20th century as variola minor came to dominate the landscape. However, as long as variola major remained in the world, only those actually exposed to variola minor or vaccinated were at least partially protected from the dangers of variola major, as shown in Table 2 below. Also seen in Table 2, is that though mortality is exponentially lower with variola minor, it was not insignificant:
Table 2: United States of America: numbers of reported cases and deaths from variola major and variola minor, 1900-1950 (from Table 8.8 in Fenner, 1988, p. 330).
| Variola major | Variola minor | |||||
| Year | Number of cases | Number of deaths | Case-fatality rate (%) | Number of cases | Number of deaths | Case-fatality rate (%) |
| 1900 | 3,328 | 603 | 18.1 | 17,736 | 291 | 1.6 |
| 1901 | 5,332 | 980 | 18.4 | 57,042 | 396 | 0.7 |
| 1902 | 10,334 | 1,841 | 17.8 | 62,612 | 669 | 1.1 |
| 1903 | 6,113 | 752 | 12.3 | 46,624 | 828 | 1.8 |
| 1904 | 5,539 | 866 | 15.6 | 26,158 | 416 | 1.6 |
| 1905 | 1,798 | 272 | 15.1 | 17,619 | 134 | 0.8 |
| 1906 | 669 | 44 | 6.6 | 14,554 | 46 | 0.3 |
| 1907 | 359 | 23 | 6.4 | 18,618 | 73 | 0.4 |
| 1908 | 391 | 27 | 6.9 | 33,607 | 81 | 0.2 |
| 1909 | 193 | 36 | 18.7 | 23,367 | 119 | 0.5 |
| 1910 | 1,216 | 252 | 20.1 | 30,038 | 177 | 0.6 |
| 1911 | 359 | 76 | 21.2 | 22,685 | 98 | 0.4 |
| 1912 | 1,164 | 204 | 17.5 | 22,402 | 101 | 0.5 |
| 1913 | 354 | 98 | 27.7 | 38,046 | 161 | 0.4 |
| 1914 | 195 | 66 | 33.8 | 40,279 | 150 | 0.4 |
| 1915 | 578 | 177 | 20.2 | 37,803 | 130 | 0.3 |
| 1916 | 300 | 78 | 26.0 | 19,440 | 169 | 0.9 |
| 1917 | 973 | 174 | 17.9 | 46,535 | 146 | 0.3 |
| 1918 | 311 | 63 | 20.3 | 80,023 | 351 | 0.4 |
| 1919 | 1,121 | 172 | 15.3 | 61,755 | 155 | 0.3 |
| 1920 | 1,214 | 157 | 12.9 | 109,458 | 291 | 0.3 |
| 1921 | 3,152 | 320 | 10.2 | 105,335 | 438 | 0.4 |
| 1922 | 2,650 | 643 | 24.3 | 30,655 | 258 | 0.8 |
| 1923 | 301 | 65 | 21.6 | 30,589 | 100 | 0.3 |
| 1924 | 4,782 | 633 | 13.2 | 51,731 | 263 | 0.5 |
| 1925 | 2,633 | 536 | 20.4 | 36,748 | 188 | 0.5 |
| 1926 | 1,560 | 238 | 15.1 | 31,134 | 152 | 0.5 |
| 1927 | 0 | – | – | 37,977 | 151 | 0.4 |
| 1928 | 0 | – | – | 39,396 | 141 | 0.4 |
| 1929 | 59 | 11 | 18.6 | 42,282 | 145 | 0.3 |
| 1930 | 0 | – | – | 48,329 | 170 | 0.4 |
| 1931 | 0 | – | – | 30,151 | 104 | 0.3 |
| 1932 | 0 | – | – | 11,194 | 52 | 0.5 |
| 1933 | 0 | – | – | 6,491 | 35 | 0.5 |
| 1934 | 0 | – | – | 5,371 | 21 | 0.4 |
| 1935 | 0 | – | – | 7,952 | 23 | 0.3 |
| 1936 | 0 | – | – | 7,834 | 33 | 0.4 |
| 1937 | 0 | – | – | 11,673 | 30 | 0.3 |
| 1938 | 0 | – | – | 14,939 | 46 | 0.3 |
| 1939 | 0 | – | – | 9,877 | 39 | 0.4 |
| 1940 | 0 | – | – | 2,795 | 15 | 0.5 |
| 1941 | 0 | – | – | 1,396 | 12 | 0.9 |
| 1942 | 0 | – | – | 865 | 3 | 0.3 |
| 1943 | 0 | – | – | 765 | 6 | 0.8 |
| Smallpox (variety not determined) | |||
| Number of cases | Number of deaths | Case-fatality rate (%) | |
| 1944 | 398 | 9 | 2.3 |
| 1945 | 346 | 12 | 3.5 |
| 1946 | 357 | 24 | 6.7 |
| 1947 | 176 | ? | ? |
| 1948 | 57 | ? | ? |
| 1949 | 49a | 1 | 2.0 |
| 1950 | 0 | – | – |
a The last probable occurrence of endemic smallpox
Though mortality was exponentially lower with variola minor, the suffering from variola minor could be substantial as shown in Table 3 below:
Table 3: Frequency of symptoms (percentages of cases) in the pre-eruptive stage in variola major and variola minor (from Table 1.3 in Fenner, 1988, p. 6). As shown in the table below, those infected with variola minor often experienced quite a bit of suffering lasting several weeks:
| Variola major | Variola minor | ||
| Symptom | 6,942 cases
(Rao, 1972) |
12,847 cases
Marsden (1936) |
859 cases
(Noble et al., 1970) |
| Fever | 100.0 | . . | 98.2 |
| Headache | 90.0 | 75.0 | 79.4 |
| Malaise | . . | . . | 66.7 |
| Chills | 6.0 | 34.0 | 62.4 |
| Anorexia | . . | . . | 60.6 |
| Backache | 90.0 | 38.8 | 44.2 |
| Pharyngitis | 15.0 | 20.6 | 38.2 |
| Nausea | . . | 11.0 | 37.0 |
| Vomiting | 50.0 | 34.2 | 30.3 |
| Diarrhea | 10.0 | . . | 3.6 |
| Delirium | 15.0 | . . | . . |
| Abdominal colic | 13.0 | . . | . . |
| Convulsions | 7.0 | . . | . . |
And, as long as variola major remained in the world, anyone anywhere was at risk from the following:
All the gravely ill patients were also tortured by mucosal symptoms. The tongue was more or less swollen and misshapen and hindered breathing through the mouth. The voice was hoarse and faltering. Swallowing was so painful that the patients refused all nourishment and, in spite of agonizing thirst, often also refused all fluids. We saw patients with deep invasion of the respiratory passages… Wails and groans filled the rooms. The patients were conscious to their last breath (Fenner, 1988, p. 27).
Typhoid and paratyphoid fever
According to Wikipedia:
Typhoid fever, also known simply as typhoid, is a bacterial infection due to Salmonella typhi that causes symptoms. Symptoms may vary from mild to severe and usually begin six to thirty days after exposure. Often there is a gradual onset of a high fever over several days. Weakness, abdominal pain, constipation, and headaches also commonly occur. Diarrhea is uncommon and vomiting is not usually severe. Some people develop a skin rash with rose colored spots. In severe cases there may be confusion. Without treatment, symptoms may last weeks or months. Other people may carry the bacterium without being affected; however, they are still able to spread the disease to others. Typhoid fever is a type of enteric fever along with paratyphoid fever. Typhoid is spread by eating or drinking food or water contaminated with the feces of an infected person. Risk factors include poor sanitation and poor hygiene (Wikipedia. Typhoid fever; see also: CDC. Typhoid Fever; Levine, 2018).
Prior to the antibiotic era, due to a 10% to 20% case-fatality rate, typhoid was a much feared disease. Beginning with chloramphenicol in 1948, the case-fatality rate plummeted to below 1% (Levine, 2018).
As early as 1873, William Budd “clearly described the contagious nature of the disease and incriminated transmission via fecally contaminated water sources (Levine, 2018, p. 114; see also Budd, 1873). Besides a vaccine that conferred some protection and newer versions still given to those traveling to areas where typhoid fever is still endemic, typhoid fever was nearly eliminated by public health approaches, mainly treatment of water; but also safer handling of foods (e.g., Curschmann, 1901; Vaughhan, 1894; Whipple, 1908). As Levine writes:
Whereas chronic carriers constitute the reservoir of S. Typhi, the maintenance of a high incidence of typhoid fever requires conditions that permit amplified transmission of S. Typhi to susceptible persons. Usually this involves fecal contamination of water sources consumed by large numbers of persons. In the later 19th and early 20th centuries, it was demonstrated in Europe and the United States that treatment of municipal water supplied caused the incidence of typhoid fever to plummet, despite the continued existence in the population of large numbers of carriers. Over one to two decades this led to the near-elimination of typhoid fever from many area (Levine, 2018, p. 1142).
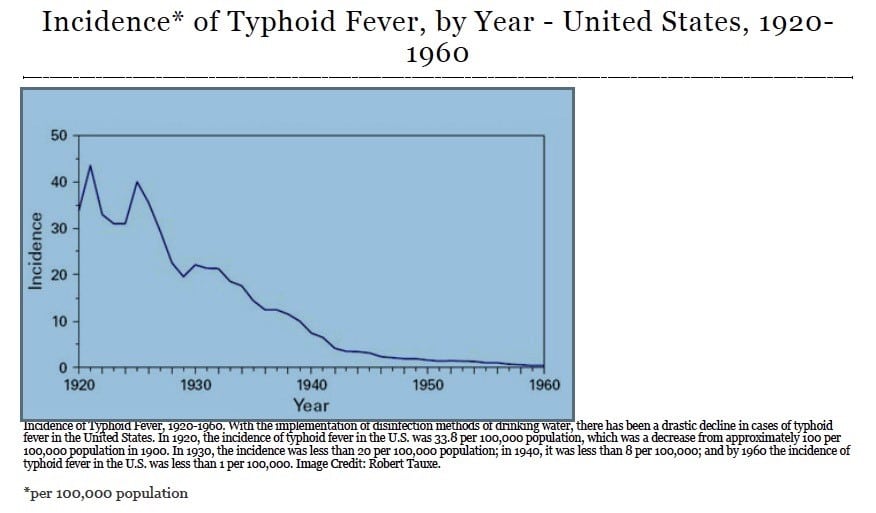
Figure 3: Incidence of Typhoid Fever, by Year – United States, 1920-1960 (from CDC. Incidence of Typhoid Fever). Besides Table 1 from the Bureau of the Census above for disease incidence from 1912 to 1970, the graph below shows the rapid decline in incidence of Typhoid Fever from 1920-1960.
Thus, typhoid fever, a mainly waterborne disease, was brought under control by public health measures with vaccinations protecting those traveling abroad and antibiotics those few unfortunate enough to become infected. Note that currently in the United States typhoid fever isn’t even included in the list of foodborne illnesses (CDC, 2016).
Whooping cough (pertussis)
According to Wikipedia:
Whooping cough (also known as pertussis or 100-day cough) is a highly contagious bacterial disease [with] weeks of severe coughing fits. Following a fit of coughing, a high-pitched whoop sound or gasp may occur as the person breathes in. The coughing may last for 10 or more weeks, hence the phrase ‘100-day cough’. The time between infection and the onset of symptoms is usually seven to ten days. Disease may occur in those who have been vaccinated, but symptoms are typically milder [my emphasis].
It is an airborne disease which spreads easily through the coughs and sneezes of an infected person. People are infectious to others from the start of symptoms until about three weeks into the coughing fits. Those treated with antibiotics are no longer infectious after five days.
The classic symptoms of pertussis are a paroxysmal cough, inspiratory whoop, and fainting, or vomiting after coughing. The cough from pertussis has been documented to cause subconjunctival hemorrhages, rib fractures, urinary incontinence, hernias, and vertebral artery dissection. Violent coughing can cause the pleura to rupture, leading to a pneumothorax [lung collapse].
Common complications include pneumonia, bronchitis, encephalopathy, earache, and seizures.
Before vaccines, an average of 178,171 cases was reported in the U.S., with peaks reported every two to five years; more than 93% of reported cases occurred in children under 10 years of age. The actual incidence was likely much higher. After vaccinations were introduced in the 1940s, pertussis incidence fell dramatically to approximately 1,000 by 1976. (Wikipedia. Whooping cough; see also: CDC. Pertussis; CDC. Pink Book. Pertussis; Edwards, 2018)
Also:
In the earliest decades of the 20th century, infection with Bordetella pertussis was essentially universal by school entry. A high cumulative incidence and roughly 1 death per 10 cases…Pertussis was made notifiable in the United States in 1922. For 2 decades, reported cases were never under 100 000 and in 1934 peaked at over 265 000 (Clark, 2014).
The estimated annual average number of cases of pertussis from 1934-1943 was 200,752 and 4,034 deaths (Roush, 1986. reprinted 2007; see also: CDC. Pertussis Cases by Year, 1922-2014). Deaths from Pertussis from 1950 to 1956 declined from 1,118 to 266 (CDC. Pink Book. Appendix E).
Diphtheria
According to Wikipedia:
Diphtheria is an infection caused by the bacterium Corynebacterium diphtheria. Signs and symptoms may vary from mild to severe…Diphtheria is usually spread between people by direct contact or through the air. It may also be spread by contaminated objects. Some people carry the bacteria without having symptoms, but can still spread the disease to others. The symptoms are due to a toxin produced by the bacteria. The symptoms of diphtheria usually begin two to seven days after infection. Symptoms of diphtheria include fever of 38 °C (100.4 °F) or above, chills, fatigue, bluish skin coloration (cyanosis), sore throat, hoarseness, cough, headache, difficulty swallowing, painful swallowing, difficulty breathing, rapid breathing, foul-smelling and bloodstained nasal discharge, and lymphadenopathy. Within two to three days, diphtheria may destroy healthy tissues in the respiratory system. The dead tissue forms a thick, gray coating that can build up in the throat or nose. This thick gray coating is called a “pseudomembrane.” It can cover tissues in the nose, tonsils, voice box, and throat, making it very hard to breathe and swallow. Symptoms can also include cardiac arrhythmias, myocarditis, and cranial and peripheral nerve palsies [various types of paralysis, often accompanied by weakness and the loss of feeling and uncontrolled body movements such as shaking]
Human-to-human transmission of diphtheria typically occurs through the air when an infected individual coughs or sneezes. Breathing in particles released from the infected individual leads to infection. Contact with any lesions on the skin can also lead to transmission of diphtheria, but this is uncommon. Indirect infections can occur, as well. If an infected individual touches a surface or object, the bacteria can be left behind and remain viable.
Diphtheria is fatal in between 5% and 10% of cases. In children under five years and adults over 40 years, the fatality rate may be as much as 20% (Wikipedia. Diphtheria; see also: CDC. Diphtheria; CDC. Pink Book. Diphtheria; Tejpratap, 2018).
According to the CDC Pink Book:
During the 1920s in the United States, 100,000–200,000 cases of diphtheria (140–150 cases per 100,000 population) and 13,000–15,000 deaths were reported each year. In 1921, a total of 206,000 cases and 15,520 deaths were reported. The number of cases gradually declined to about 19,000 in 1945 (15 per 100,000 population). A more rapid decrease began with the widespread use of diphtheria toxoid in the late 1940s (CDC. Pink Book. Diphtheria).
According to Roush the estimated annual average prevaccine from 1936-1945 was 21,053 cases and 1,822 deaths with a rapid decline following the introduction of the vaccine (Roush, 2007).
As Grob writes:
Whooping cough, measles, scarlet fever, and diphtheria—all of which had taken a heavy toll among children in the nineteenth century—began to fall as a cause of mortality even the prevalence rates often remained high. By 1940 these diseases no longer posed a serious threat to life. Survival rates among children were correspondingly enhanced. Mortality rates in the 1-to-4 year group fell from 19.8 per 1,000 to 2.9 in 1940.
The decline in mortality from infectious diseases associated with childhood admit no simple explanation. The case of diphtheria is something of an exception, largely because effective interventions became available in the 1890s.
By 1894 an antitoxin with therapeutic qualities had been developed, and two decades later an effective means of immunizing children became available with the introduction of the toxin-antitoxin. Yet the precise role played by both in reducing mortality from diphtheria is ambiguous…There is some evidence that the emergence of a dominant strain of mitis [Editor’s note: a variant of the bacterium that caused a relatively mild form of the disease] reduced the virulence of the disease. Antitoxin serum may therefore have merely assisted a natural decline of the disease already under way. During the 1920s …immunization campaigns probably led to the eventual disappearance of the disease by World War II (Grob, 2002, pp. 205-6).
Rosen writes:
By 1900, diphtheria could be diagnosed by precise bacteriological methods, the sick person could be treated with diphtheria antitoxin, and well carriers could be detected, thus making possible really effective control. The next important step was to be made in the direct prevention of the disease. This was achieved by active mass immunization…In 1920 active immunization of school children began…by [1940], the disease had been virtually eliminated as a cause of death, with the mortality rate at 1.1 per 100,000. This was in striking contrast to a rate of 785 per 100,000 in 1894.
That the drop in diphtheria morbidity and mortality is not wholly due to preventive immunization appears to be indicated by the fact that this decline set in actually in the nineteenth century before diphtheria antitoxin began to be used generally, and continue progressively even before preventive immunization became widespread. The death rate among children up to 10 years of age in New York City was 785 per 100,000 in 1894, declining to less than 300 in 1900; and in 1920, when active immunization of school children began, it fell below 100…Certainly, the downward course of diphtheria morbidity and mortality has at least been accelerated by preventive immunization (Rosen, 1993, pp. 312-314).
From Rosen, as with smallpox, diphtheria may well have mutated to a more benign form, though still lethal for many, and antitoxin and finally a vaccine ended its reign.
Syphilis and sequaelae
According to Wikipedia:
Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum subspecies pallidum. The signs and symptoms of syphilis vary depending in which of the four stages it presents (primary, secondary, latent, and tertiary). The primary stage classically presents with a single chancre (a firm, painless, non-itchy skin ulceration) but there may be multiple sores. In secondary syphilis a diffuse rash occurs, which frequently involves the palms of the hands and soles of the feet. There may also be sores in the mouth or vagina. In latent syphilis, which can last for years, there are few or no symptoms. In tertiary syphilis there are gummas (soft non-cancerous growths), neurological, or heart symptoms.
Syphilis is transmitted primarily by sexual contact or during pregnancy from a mother to her fetus; the spirochete is able to pass through intact mucous membranes or compromised skin. It is thus transmissible by kissing near a lesion, as well as oral, vaginal, and anal sex. Approximately 30% to 60% of those exposed to primary or secondary syphilis will get the disease.
Condom use reduces the likelihood of transmission during sex, but does not completely eliminate the risk. Congenital syphilis in the newborn can be prevented by screening mothers during early pregnancy and treating those who are infected.
Syphilis can be effectively treated with antibiotics (Wikipedia. Syphilis; see also: CDC. Syphilis).
Syphilis differs from the other diseases in Humphries comparison. It is the only one that depends on “intentional”, avoidable behaviors.
Jabbour writes:
Around the turn of the twentieth century, syphilis was a public health disaster in the United States of America. Because of the lack of official reporting of cases to public authorities, estimates of its incidence are difficult to obtain; however, the figure has been estimated conservatively at ten percent to fifteen percent of the general population from about 1900 to 1920, although its occurrence was presumed to be higher among men than women. Furthermore, since it is transmitted primarily through sexual contact, syphilis was a huge stigma that all individuals wanted to avoid. When people did contract the disease, they were therefore inclined to hide it from the public so as to avoid being permanently branded by their communities. Because of the disgrace associated with syphilis, the topic was generally avoided by the public and the media, such that a veil of secrecy came to conceal it.
Syphilis represented a unique public health challenge because it carried with it a huge stigma and because it was transmitted by sexual contact [my emphasis] (Jabbour, 2000).
With the advent of penicillin in 1943, syphilis became curable. “A rarity in the interplay of antibiotics and bacteria, penicillin has remained effective in the treatment of T. pallidum since its introduction, and it continues to be an efficacious first line therapy (Willeford, 2016).”
The American Sexual Health Association was founded in 1913 to fight prostitution and the venereal disease epidemic through public education on sexually transmitted disease and working to break down the social stigma attached to venereal diseases. During both World Wars they were instrumental in breaking up prostitution rings targeting military personnel (Wikipedia. American Sexual Health Association). In 1960 it changed its name to American Social Health Association and continues to this day. Various groups developed programs, including textbooks, “to shape and tame ‘the native capacities’ of impoverished children into socially acceptable, monogamous heterosexuals” (Egan, 2009).
An example of an excellent early medical book is Vedder’s 1918, Syphilis and Public Health. The book includes statistics, methods of transmission, and “Methods that May Be Taken by the Individual to Prevent Genital Infection [and] Public Health Measures”. An excellent book on the history of syphilis in the U.S. since 1880 is: Allan M. Brandt (1987). No Magic Bullet: A Social History of Venereal Disease in the United States Since 1880 (Enlarged Edition). Oxford University Press.
Malaria
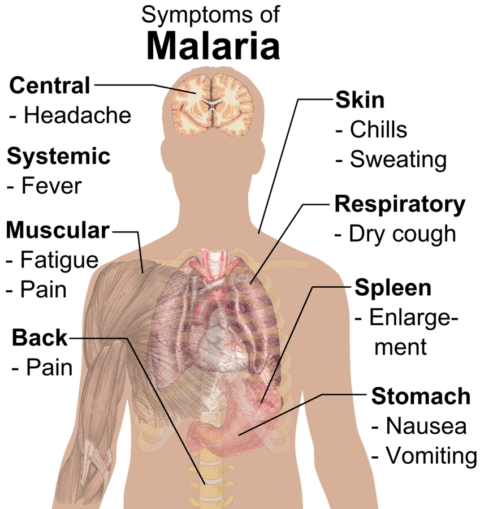
Mikael Häggström Wikipedia. Malaria
According to Wikipedia:
Malaria is a mosquito-borne infectious disease affecting humans and other animals caused by parasitic protozoans (a group of single-celled microorganisms) belonging to the Plasmodium group. Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches. In severe cases it can cause yellow skin, seizures, coma, or death. Symptoms usually begin ten to fifteen days after being bitten.
The risk of disease can be reduced by preventing mosquito bites through the use of mosquito nets and insect repellents, or with mosquito control measures such as spraying insecticides and draining standing water. Several medications are available to prevent malaria in travellers to areas where the disease is common.
The classic symptom of malaria is paroxysm—a cyclical occurrence of sudden coldness followed by shivering and then fever and sweating, occurring every two days (tertian fever) in P. vivax and P. ovale infections, and every three days (quartan fever) for P. malariae. P. falciparum infection can cause recurrent fever every 36–48 hours, or a less pronounced and almost continuous fever.
Malaria has several serious complications. Among these is the development of respiratory distress, which occurs in up to 25% of adults and 40% of children with severe P. falciparum malaria. Although rare in young children with severe malaria, acute respiratory distress syndrome occurs in 5–25% of adults and up to 29% of pregnant women.
Malaria in pregnant women is an important cause of stillbirths, infant mortality, abortion and low birth weight, particularly in P. falciparum infection, but also with P. vivax.
Although P. falciparum traditionally accounts for the majority of deaths, recent evidence suggests that P. vivax malaria is associated with potentially life-threatening conditions about as often as with a diagnosis of P. falciparum infection.
Symptoms of malaria can recur after varying symptom-free periods.
Methods used to prevent malaria include medications, mosquito elimination and the prevention of bites. There is no vaccine for malaria. The presence of malaria in an area requires a combination of high human population density, high Anopheles mosquito population density and high rates of transmission from humans to mosquitoes and from mosquitoes to humans. If any of these is lowered sufficiently, the parasite will eventually disappear from that area, as happened in North America, Europe and parts of the Middle East. However, unless the parasite is eliminated from the whole world, it could become re-established if conditions revert to a combination that favors the parasite’s reproduction (Wikipedia. Malaria; see also: CDC. Malaria).
Though many articles and papers emphasize the public health contribution to the decline of malaria in the United States (e.g., Andrews, 1950; Andrews, 1963; Wikipedia. National Malaria Eradication Plan; CDC. Elimination of Malaria in the United States (1947-1951); Sledge, 2013), Gerard Grob, Professor of the History of Medicine at Rutgers University, paints a slightly different historical picture, emphasizing economic policies:
The disappearance of malaria did not follow the introduction of any public health measures or novel medical therapies. Indeed, the fact that the disease established such a firm foothold in the United States at all was surprising; malaria, after all, was a tropical disease. Settlement patterns near waterways, disruption of drainage patterns, and agricultural practices, however, combined to create optimum conditions for the spread of the disease by providing mosquitoes with ideal breeding sites. In the South the Anopheles quadrimaculatis was the primary vector. This mosquito breeds in still water, prefers an alkaline pH, and has an affinity to live in buildings rather than the wild.
At the beginning of the Great Depression of the 1930s, the areas with high malarial morbidity and mortality rates included parts of South Carolina, Georgia, Florida and Alabama, the Mississippi Delta region, and the portion of the Red River Valley near the junction of Oklahoma, Arkansas, Louisiana, and Texas. In many of these places human environmental modifications proved crucial. The experience of the Mississippi region is instructive. This area was devoted to cotton cultivation and provided an ideal environment for mosquito breeding because of the multiplicity of ponds of still water than followed the receding of river floods in the spring season. Agricultural laborers tended to live close to the fields, and provided a reservoir of infected and susceptible persons…Generally speaking, malaria had long since disappeared in most urban sites.
Although drainage projects and the use of insecticides became more common after 1900, neither played decisive roles in the disappearance of the disease. Faust, a leading authority…indicated that improving economic conditions may have played an important role.
More recently Margaret Humphreys has emphasized the critical role of population movements. During the 1930s people moved from urban area with high unemployment rates and returned to abandoned hacks in the countryside; many of these were located adjacent to stagnant water. The migration of infected persons further assisted the spread of the disease. By the end of the decade, however, the situation was reversed; outmigration from the southern countryside was characteristic. New Deal agricultural legislation encouraged large-scale farming and mechanization, which in turn depopulated rural areas and hastened the growth of towns and cities outside the infective zone. As the number of infected persons declined, the ability of mosquitoes to spread malaria diminished correspondingly. The malaria parasite, in other words, depended on frontier conditions of poverty and proximity to water. As rural southern poverty diminished, the parasite disappeared (Grob, 2002, pp. 185-6; see also: Barreca, 2007; Faust, 1945; Humphreys, 1996).
As can be seen from the Table 1 above, by 1946 the incidence of malaria in the United States had plummeted. Also note the continuous decline in mortality for malaria from the figure below:
Figure 4: Morbidity and mortality rates for malaria in all States reporting cases and deaths, 1920 to 1940 (Chart 3 in Andrews, 1963).
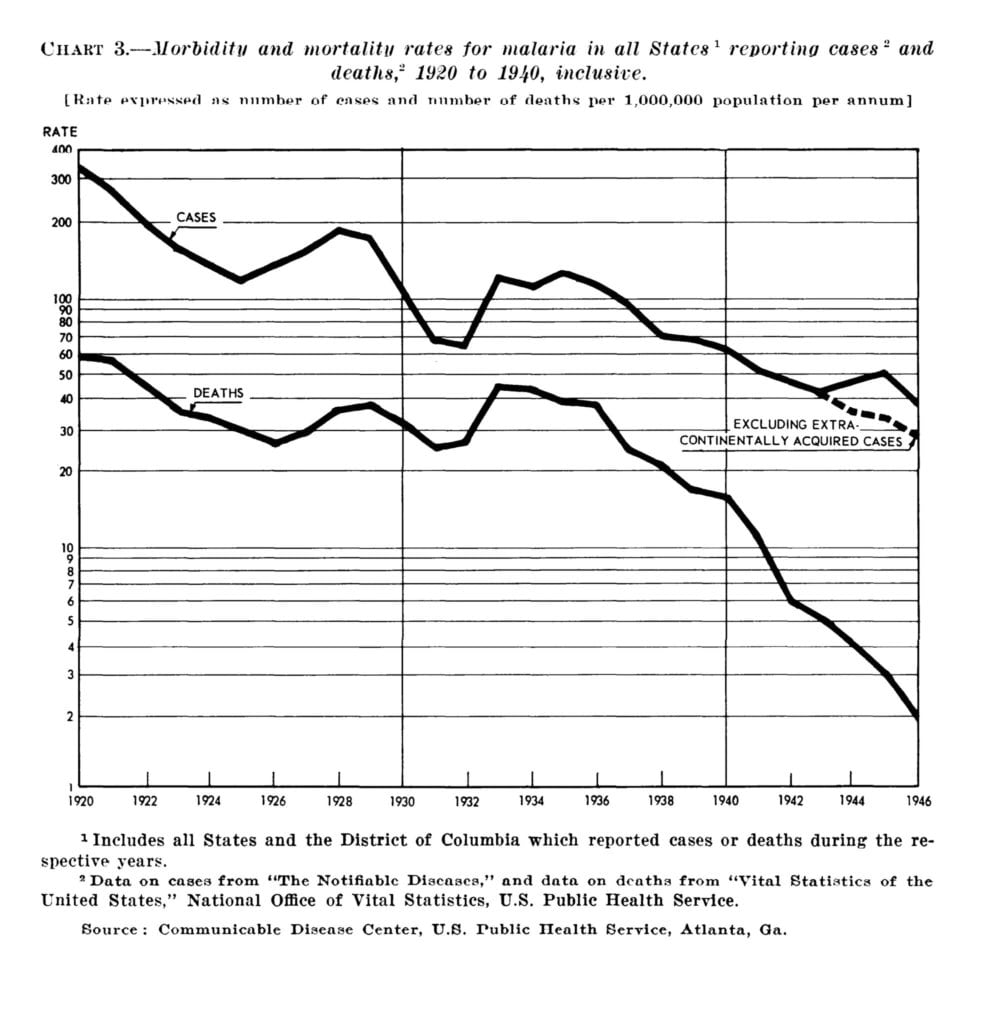
And, for example: “Today deaths resulting from malaria naturally acquired in the United States are probably considerably less than 10 per annum, as contrasted with nearly 5000 annually during the period 1933-1935 (Faust, 1951).
Malaria, a mosquito-borne disease, showed an exponential decline in both morbidity and mortality for the first half of the 20th Century, and was basically eliminated in the United States by the end of World War II through economic policies and public health measures.
Poliomyelitis
According to the CDC Pink Book Chapter on Poliomyelitis:
Poliovirus is a member of the enterovirus subgroup…Enteroviruses are transient inhabitants of the gastrointestinal tract.
There are three poliovirus serotypes (P1, P2, and P3). There is minimal heterotypic immunity between the three serotypes.
The virus enters through the mouth, and primary multiplication of the virus occurs at the site of implantation in the pharynx and gastrointestinal tract. The virus is usually present in the throat and in the stool before the onset of illness. One week after onset there is less virus in the throat, but virus continues to be excreted in the stool for several weeks. The virus invades local lymphoid tissue, enters the bloodstream, and then may infect cells of the central nervous system. Replication of poliovirus in motor neurons of the anterior horn and brain stem results in cell destruction and causes the typical manifestations of poliomyelitis.
Clinical Features
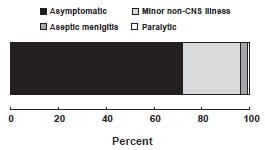
The incubation period for nonparalytic poliomyelitis is 3-6 days. For the onset of paralysis in paralytic poliomyelitis, the incubation period usually is 7 to 21 days.The response to poliovirus infection is highly variable and has been categorized on the basis of the severity of clinical presentation.
Up to 72% of all polio infections in children are asymptomatic. Infected persons without symptoms shed virus in the stool and are able to transmit the virus to others.
Approximately 24% of polio infections in children consist of a minor, nonspecific illness without clinical or laboratory evidence of central nervous system invasion. This clinical presentation is known as abortive poliomyelitis, and is characterized by complete recovery in less than a week. This is characterized by a low grade fever and sore throat.
Nonparalytic aseptic meningitis (symptoms of stiffness of the neck, back, and/or legs), usually following several days after a prodrome similar to that of minor illness, occurs in 1%–5% of polio infections in children. Increased or abnormal sensations can also occur. Typically these symptoms will last from 2 to 10 days, followed by complete recovery.
Outcomes of poliovirus infection:
Fewer than 1% of all polio infections in children result in flaccid paralysis. Paralytic symptoms generally begin 1 to 18 days after prodromal symptoms and progress for 2 to 3 days. Generally, no further paralysis occurs after the temperature returns to normal. The prodrome may be biphasic, especially in children, with initial minor symptoms separated by a 1- to 7-day period from more major symptoms. Additional prodromal signs and symptoms can include a loss of superficial reflexes, initially increased deep tendon reflexes and severe muscle aches and spasms in the limbs or back. The illness progresses to flaccid paralysis with diminished deep tendon reflexes, reaches a plateau without change for days to weeks, and is usually asymmetrical. Strength then begins to return. Patients do not experience sensory losses or changes in cognition.
Many persons with paralytic poliomyelitis recover completely and, in most, muscle function returns to some degree. Weakness or paralysis still present 12 months after onset is usually permanent.
Paralytic polio is classified into three types, depending on the level of involvement. Spinal polio is most common, and during 1969–1979, accounted for 79% of paralytic cases. It is characterized by asymmetric paralysis that most often involves the legs. Bulbar polio leads to weakness of muscles innervated by cranial nerves and accounted for 2% of cases during this period. Bulbospinal polio, a combination of bulbar and spinal paralysis, accounted for 19% of cases.
The death-to-case ratio for paralytic polio is generally 2%–5% among children and up to 15%–30% for adults (depending on age). It increases to 25%–75% with bulbar involvement.
TransmissionPerson-to-person spread of poliovirus via the fecal-oral route is the most important route of transmission, although the oral-oral route is possible.
Temporal Pattern
Poliovirus infection typically peaks in the summer months in temperate climates. There is no seasonal pattern in tropical climates.
Communicability
Poliovirus is highly infectious, with seroconversion rates among susceptible household contacts of children nearly 100%, and greater than 90% among susceptible household contacts of adults. Persons infected with poliovirus are most infectious from 7 to 10 days before and after the onset of symptoms, but poliovirus may be present in the stool from 3 to 6 weeks (CDC. Pink Book. Poliomyelitis; see also: CDC. What Is Polio?; Sutter, 2018; Wikipedia. Poliomyelitis).
While the other diseases discussed above were on the decline, polio was on the rise. Trevelyan (2005):
A disease originally considered mildly contagious is now regarded as very contagious—almost as much as measles …From an endemic disease it has tended to become epidemic and is now a common and periodic scourge and incidentally an item of great public interest. Poliomyelitis is one of the important emergent viral diseases of the twentieth century. From an apparently rare clinical condition—occurring only sporadically or in small outbreaks prior to the late nineteenth century— poliomyelitis had, by the 1940s and 1950s, emerged as an epidemic disease of global proportions.
While faecal contamination (of fingers, eating utensils, milk or foodstuffs) is considered to be the more common means of transmission, [droplet spread from the pharynx, a corridor of spread used by other childhood diseases like chicken-pox, diphtheria, measles, and rubella] is a critical second strand in the person-to-person propagation of the disease. Indeed, among older populations, and where high standards of sanitation are maintained, droplet spread may be the predominant route of poliovirus transmission. Finally, we note that, in contrast to some other diseases that involve faecal-oral transmission (notably, cholera), contaminated water supplies are not a prerequisite for major epidemics of poliomyelitis.
Infection with poliovirus is overwhelmingly subclinical, with the estimated ratio of inapparent to severe (paralytic) infections ranging up to 850:1. There were thirty-nine polio epidemics in the U.S. between 1910- 1971 (Trevelyan, 2005, pp. 35-36; see also: Smallman-Raynor, 2006).
[Note that the Trevelyan article and especially the Smallman-Raynor book cover in detail the history and geography of polio epidemics in the United States]
Swimming pools, chlorine, and polio
As I mentioned in the introduction, during polio season my mother didn’t allow me to go to the municipal swimming pool. Turns out, mother knows best, at least, sometimes. Chlorine does kill the polio virus, though not immediately. However, the chlorine must come in contact with the virus and if one child infected with the virus is leaking fecal matter in a swimming pool, only virus particles at the surface of the fecal matter can be reached by the chlorine, so other children can easily swallow the microscopic polio-infested bits of fecal matter. One study of polio virus particles, not fecal matter, concluded: “Complete inactivation of enteric viruses (beyond the limit of detection) was not achieved by the usual conditions for bacterial disinfection of water supplies …The results suggest that inactivation of enteric viruses in water at pH 7, 25 C, requires a minimum free residual chlorine concentration of 0.3 ppm for contact periods of at least 30 minutes” (Kelly, 1958). And actual studies from water samples from swimming pools found that chlorine had been effective at killing bacteria; but not viruses (Keswick, 1981; see also: Bates, 1977; Payment, 1985; Sinclair, 2009).
In other words, what worked for typhoid, a bacteria, didn’t work for polio, a virus.
Polio epidemics, incidence, morbidity (paralysis), and mortality
Humphries graph above, Figure 1, and Table 1 from the Bureau of the Census also above give the incidence of poliomyelitis from 1912-1969/70. However, to repeat what I wrote above:
It is not the incidence of a disease that is most relevant, otherwise all the diseases included in Humphries graph pale compared to the common cold and even food poisoning, which an estimated 1 in 6 Americans (48 million people) get every year, resulting in 128.000 hospitalizations, and 3,000 deaths (CDC. Burden of Foodborne Illnesses). What is important are:
- Degree of suffering
- Disability
- Mortality
- Mode of transmission
- Factors affecting the above (e.g., public health measures)
Prior to 1951, reported polio cases were not separately characterized as paralytic versus non-paralytic. Humphries argues in her chapter that even the classification of these cases is suspect, lacking laboratory confirmation, and changing criteria for defining paralysis. In Part 2, I will discuss in more detail criteria for classifying cases, both clinical and laboratory, and differential diagnoses. For this paper, my focus is on Humphries claim: “Given what a low-incidence disease it was, how did polio come to be perceived as such an infamous monster? This is a question worthy of consideration, especially in light of the fact that the rate was far less than other common diseases (Humphries, p. 213).” Keep in mind that whatever Humphries claims, at the time both doctors and the public believed the data and, as Parts 2 and 3 will show, they were right. As I will discuss in this paper and in Part 2, the fact that some cases were misdiagnosed is not questioned, something one finds in all aspects of medicine; but the vast majority of cases reported as polio were polio!
Polio mortality
First, let’s look at deaths, something even Humphries can’t claim were misdiagnosed.
Figure 5: gives the death rates for polio per 100,000 population from 1910-1975 (from Isabella B, 2015).
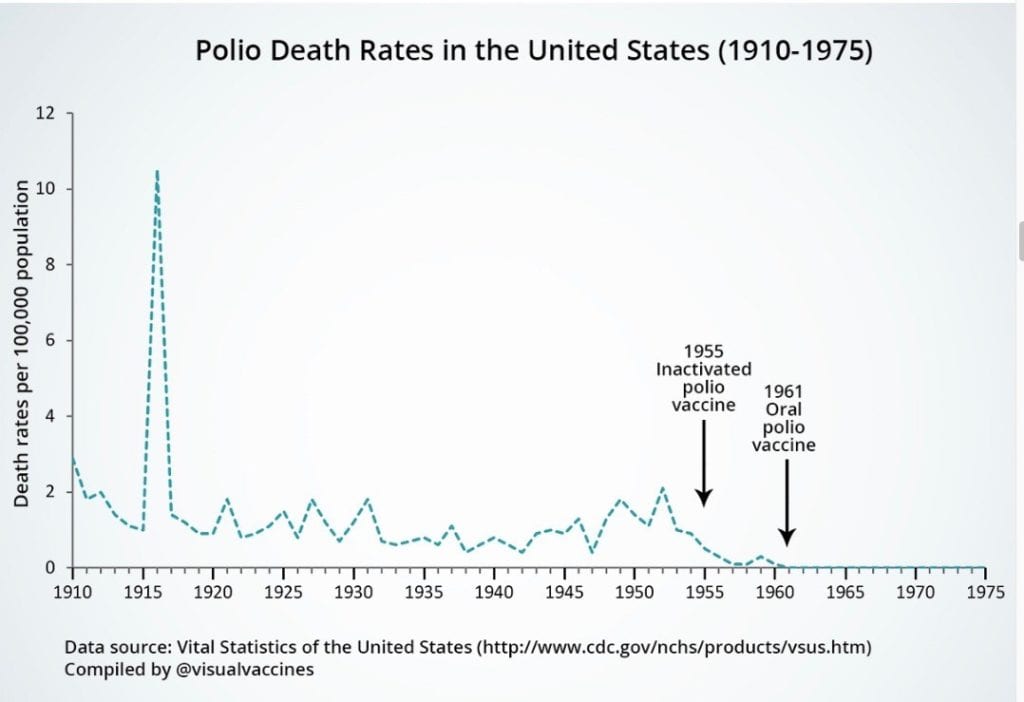
Table 4. The following table from the CDC Pink Book Appendix E allows one to compare death rates from several of the diseases used in Humphries comparison graph. The table also includes paralytic cases separately starting in 1951. Appendix E only listed total cases for 1951-1953, so I added in parentheses the number of reported paralytic cases (Post-Polio Health International).
Reported cases and deaths from vaccine preventable diseases, united states, 1950-1982
| Measles | Diphtheria | Pertussis | Polio (paralytic)
†Total reported cases From 1951, MMWR separated paralytic and nonparalytic cases. Before 1951, MMWR included both as Total Cases. |
|||||
| Year | Cases | Deaths | Cases | Deaths | Cases | Deaths | Cases | Deaths |
| 1950 | 319,124 | 468 | 5,796 | 410 | 120,718 | 1,118 | 33,300† | 1,904 |
| 1951 | 530,118 | 683 | 3,983 | 302 | 68,687 | 951 | 28,386†
(10,037) |
1,551 |
| 1952 | 683,077 | 618 | 2,960 | 217 | 45,030 | 402 | 57,879†
(21,269) |
3,145 |
| 1953 | 449,146 | 462 | 2,355 | 156 | 37,129 | 270 | 35,592†
(15,648) |
1,450 |
| 1954 | 682,720 | 518 | 2,041 | 145 | 60,886 | 373 | 18,308 | 1,368 |
| 1955 | 555,156 | 345 | 1,984 | 150 | 62,786 | 467 | 13,850 | 1043 |
| 1956 | 611,936 | 530 | 1,568 | 103 | 31,732 | 266 | 7,911 | 566 |
| 1957 | 486,799 | 389 | 1,211 | 81 | 28,295 | 183 | 2,499 | 221 |
| 1958 | 763,094 | 552 | 918 | 74 | 32,148 | 177 | 3,697 | 255 |
| 1959 | 406,162 | 385 | 934 | 72 | 40,005 | 269 | 6,289 | 454 |
| 1960 | 441,703 | 380 | 918 | 69 | 14,809 | 118 | 2,525 | 230 |
| 1960 | 423,919 | 434 | 617 | 68 | 11,468 | 76 | 988 | 90 |
| 1962 | 481,530 | 408 | 444 | 41 | 17,749 | 83 | 762 | 60 |
| 1963 | 385,156 | 364 | 314 | 45 | 17,135 | 115 | 396 | 41 |
| 1964 | 458,083 | 421 | 293 | 42 | 13,005 | 93 | 106 | 17 |
| 1965 | 261,904 | 276 | 164 | 18 | 6,799 | 55 | 61 | 16 |
| 1966 | 204,136 | 261 | 209 | 20 | 7,717 | 49 | 106 | 9 |
| 1967 | 62,705 | 81 | 219 | 32 | 9,718 | 37 | 40 | 16 |
| 1968 | 22,231 | 24 | 260 | 30 | 4,810 | 36 | 53 | 24 |
| 1969 | 25,826 | 41 | 241 | 25 | 3,285 | 13 | 18 | 13 |
| 1970 | 47,351 | 89 | 435 | 30 | 4,249 | 12 | 31 | 7 |
| 1971 | 75,290 | 90 | 215 | 13 | 3036 | 18 | 17 | 18 |
| 1972 | 32,275 | 24 | 152 | 10 | 3,287 | 6 | 29 | 2 |
| 1973 | 26,690 | 23 | 228 | 10 | 1,759 | 5 | 7 | 10 |
| 1974 | 22,094 | 20 | 272 | 5 | 2,402 | 14 | 7 | 3 |
| 1975 | 24,374 | 20 | 307 | 5 | 1,738 | 8 | 13 | 9 |
| 1976 | 41,126 | 12 | 128 | 7 | 1,010 | 7 | 10 | 16 |
| 1977 | 57,345 | 15 | 84 | 5 | 2,177 | 10 | 19 | 16 |
| 1978 | 26,871 | 11 | 76 | 4 | 2,063 | 6 | 8 | 13 |
| 1979 | 13,597 | 6 | 59 | 1 | 1,623 | 6 | 22 | 1 |
| 1980 | 13,506 | 11 | 3 | 1 | 1,730 | 11 | 9 | 2 |
| 1981 | 3,124 | 2 | 5 | 0 | 1,248 | 6 | 10 | 0 |
| 1982 | 1714 | 2 | 2 | 1 | 1,895 | 4 | 12 | 0 |
As can be seen from the table, the number of deaths from polio was substantially higher from 1950-1956 than any of the other disease. Perhaps, as from 1953, Humphries doesn’t consider 3,145 deaths from polio, mainly children, of any importance? Note that I will discuss in Part 2 how these cases were confirmed to be polio. Note also from the table above that number 2 in number of deaths from 1950 on was measles, with a high of 683 in 1951, just a minor blip on the screen according to Humphries, to repeat what she wrote: “In the case of measles, the death rate had declined by almost 100 percent. You would never know it today, but the dreaded measles was no longer a major issue in the Western world by the time vaccines were deployed (p.174).”
Polio morbidity/paralysis
Though as discussed above, “fewer than 1% of all polio infections in children result in flaccid paralysis and most did eventually regain some or complete mobility;” however, given the large number infected during epidemics, there were still a substantial number of victims paralyzed. In addition, as polio doesn’t affect the sensory nerves, many suffered intense pain and months to years to recover (e.g., Sass, 1996; Seavey, 1998; Silver, 2007).
Humphries writes:
The practice among doctors before 1954 was to diagnose all patients who experienced even short-term paralysis (24 hours) with “polio.” In 1955, the year the Salk vaccine was released, the diagnostic criteria became much more stringent. If there was no residual paralysis 60 days after onset, the disease was not considered to be paralytic polio. This change made a huge difference in the documented prevalence of paralytic polio because most people who experience paralysis recover prior to 60 days. Dr. Greenberg said:
The change in 1955 meant that we were reporting a new disease, namely, paralytic poliomyelitis with a longer-lasting paralysis. Furthermore diagnostic procedures have continued to be refined. Coxsackie virus and aseptic meningitis have been distinguished from paralytic poliomyelitis. Prior to 1954 large numbers of these cases were mislabeled as paralytic poliomyelitis. Thus, simply by changes in diagnostic criteria, the number of paralytic cases was predetermined to decrease in 1955-1957, whether or not any vaccine was used (Humphries, p. 219).
Note that from Figure 6 below, even with Greenberg’s adjustments, there remained a substantial number of paralytic cases, e.g., 1951 (7,000), 1952 (14,000). Note the black portion of each bar.
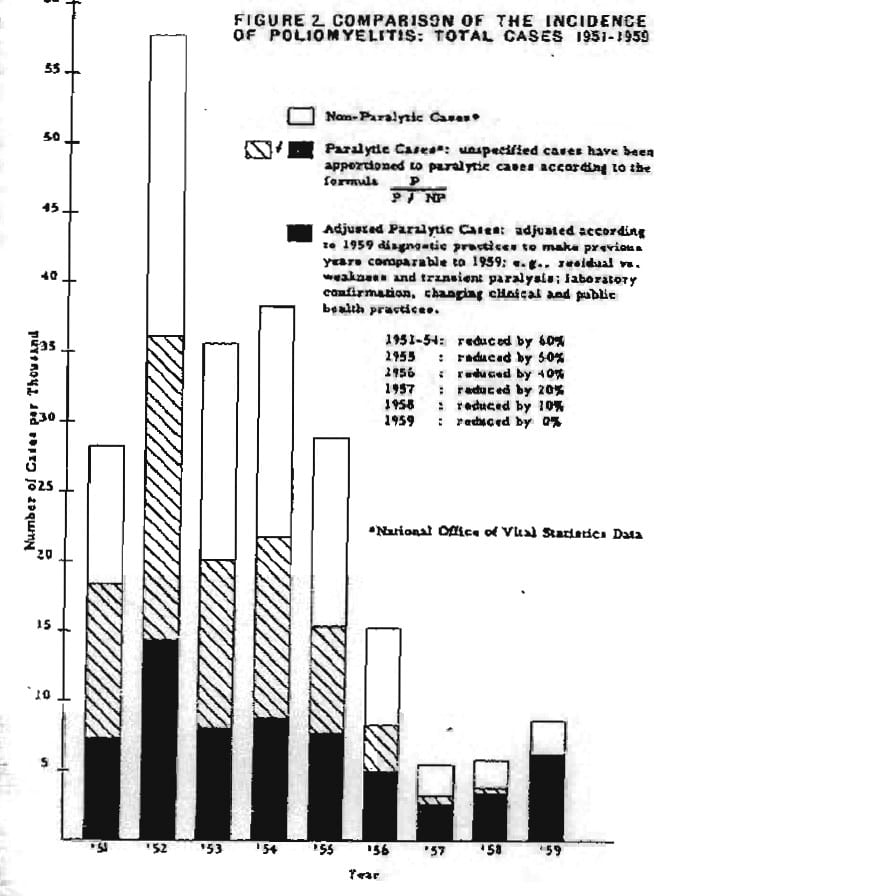
Figure 6: Dr. Greenberg’s chart showing what the incidence, total cases of paralytic polio would have been in former years if the diagnostic criteria of 1959 had been used (from Ratner, 1960, p. 5).
Humphries goes on to write:
As a case in point on how much paralytic disease thought to be polio was not at all associated with polioviruses, consider the well-documented Michigan epidemic of 1958. This epidemic occurred four years into the Salk vaccine campaign. An in-depth analysis of the diagnosed cases revealed that more than half of them were not poliovirus associated at all [AND then quotes from the paper] In a large number of paralytic as well as nonparalytic patients poliovirus was not the cause (Humphries, p. 219).
Let’s look at the actual data from the Michigan study; but first, according to Brown (1960):
An additional correlation of clinical and laboratory information was made possible by the fact that 550 of the patients in the Detroit area were examined for muscles weakness 60 days after onset of disease. The results are presented in table 7 [Table 5 below] in terms of the degree of paralysis two months after infections, and they are arranged according to the clinical diagnosis at the time of admission to hospital and according to the results of laboratory tests carried out on specimens from these patients. It is obvious that most of the 308 patients considered to be nonparalytic on admission were also classified in that category two months later. Virus was isolated from only one-half of those among whom ECHO and Coxsackie viruses were equally responsible with poliovirus for the infections. Among the 242 patients originally diagnosed as paralytic, 187, or 77% were confirmed by laboratory tests to have poliomyelitis. The vast majority of these (84%) were found to have residual paralysis 60 days after onset of the illness, and it is of interest that 83% of these paralytic patients were unvaccinated and only four, or 2.5%, had received three doses of vaccine.
Table 5: Correlation of Laboratory Findings of Poliomyelitis with Muscle Examination Performed 60 Days from Onset of Illness (from Table 7 in Brown, 1960).
| Original diagnosis | Laboratory diagnosis | Results of muscle examination, No. | |||||
| Type | No. | Type | No. | NP* | P1a | P2b | P3c |
| Nonparalytic | 308 | Polio | 66 | 56 | 4 | 1 | 3 |
| ECHO | 53 | 52 | 1 | . . . | . . . | ||
| Coxsackie | 41 | 40 | . . . | 1 | . . . | ||
| Negative | 148 | 143 | 5 | . . . | . . . | ||
| Paralytic | 242 | Polio | 187 | 29 | 49 | 67 | 42 |
| ECHO | 2 | . . . | 2 | . . . | … | ||
| Negative | 53 | 20 | 11 | 15 | 7 | ||
* NP = non paralytic b P2 = significant paralysis
a P1 = minor involvement c P3 = sever paralysis or death
In Part 2, I will discuss in more depth changing definitions of paralysis, labs, and differential diagnoses; but as should be clear from the above:
- Even with Greenberg’s adjustments, there was a significant number of cases of paralysis.
- While Humphries, based on the introduction to Brown’s paper, stated, “An in-depth analysis of the diagnosed cases revealed that more than half of them were not poliovirus associated at all,” the introduction doesn’t separate the paralytic cases from the non-paralytic ones, while for the paralytic cases, the paper actually states that 77% were laboratory confirmed to be poliomyelitis and 84% of these had residual paralysis 60 days later. So, rather than “more than half of them were not poliovirus associated,” 77% were and 65% had paralysis 60 days later, based on criteria used by Greenberg. Didn’t Humphries read the entire paper? In addition, as Brown states: “Antibody determinations were possible on 185 of the 292 patients from whom poliovirus had been isolated,” so, for the cases that were not lab confirmed, this does not mean that they were not caused by poliomyelitis (Brown, 1960, p. 109).
So, Humphries displays a callous disregard for the significant number of cases with long-term paralysis and, based on her use of the Brown paper, her credibility is highly questionable!
Humphries probably missed that Greenberg, in discussing the incidence of paralytic polio up to 1957 also stated:
The present increase, I believe, is caused by a long-term, increasing trend in the incidence of the condition or disease we now call paralytic poliomyelitis. Without doubt, the increasing trend has been reduced to some extent by the Salk vaccine…If there were no other vaccine, complete vaccination of all susceptible persons in the population with Salk vaccine would be justifiable (Ratner, 1960, p. 89).
Humphries probably missed that Greenberg later chaired the Committee for the Study of Poliomyelitis Vaccines finding:
The development of vaccines against poliomyelitis has been a major achievement of modern preventive medicine. It might seem remarkable that United States policies in regard to poliomyelitis vaccination are being reexamined in view of the extraordinary success of the present program. Recently, serious questions have been raised about the present policy that advocates the use of the live attenuated oral poliovirus vaccine (OPV) to the virtual exclusion of the killed, or inactivated poliomyelitis vaccine (IPV). This policy has been in effect since 1962 when the decision was made to change from the use of IPV even though paralytic disease had decreased dramatically in the eight years since its introduction [my emphasis].
In considering the available data with particular reference to the experience in countries where only IPV has been used, the committee concluded that when properly used, either vaccine is highly effective both in preventing disease and in reducing circulation of wild virus in the community.
Both IPV and OPV are remarkably safe vaccines, although as indicated, rare cases of vaccine-associated paralytic disease occur in OPV recipients and their contacts.
The committee urges the United States to set the following goal:
To achieve more than 90 percent immunization status—as other countries have already done—as soon as possible. When this goal is achieved, contact cases will virtually disappear. Within five years aim for no less than 80 percent immunization status; in 10 years, for no less than 90 percent immunization status (Greenberg, 1977, pp. 1-11; see also: Nightingale, 1977).
So, with further data, based on the criteria for paralysis that Greenberg used to adjust the earlier data, where he concluded the vaccine reduced the incidence of cases, with additional data, his original conclusion not only was right, but proved even more valid. How did Humphries miss this?
Just to be clear, the changed definition of paralytic cases explained by Greenberg did eliminate a substantial number of cases of paralysis, as many as 30,000 during the first half of the 1950s; but a significant number of paralytic cases remained and in the following years, based on the revised definition, following the introduction of the vaccine, these numbers continued to decline until there were none, so, whatever some claim, the evidence for the effectiveness of the vaccine is substantial and undeniable.
And finally, Bruno makes a compelling case that the total number of people infected with the virus, even some with mild paralysis, was actually underestimated. And as discussed below under the subheading, Post-polio syndrome, the polio virus did result in severe neuron damage in many of these cases. Bruno writes:
Patients Did Not Present for Diagnosis. Failure to present for diagnosis may have resulted from symptoms being very mild or not being seen as indicative of poliovirus infection and from patients, especially those who were poor, not having access to or being financially unable to travel for medical care.
Paralytic Polio Was Underdiagnosed. Studies document the underdiagnosis of paralytic polio. Shaw and Levin reported that “mild degrees of muscle weakness may be easily overlooked” if manual muscle testing were employed without a functional assessment of strength.
Polio Cases Were Not Reported. Although diagnosis may have been more accurate and reporting to public health authorities more likely at city hospitals, the number and severity of polio cases during the epidemics may have prevented overwhelmed physicians from reporting the occurrence of polio, especially NPP, to local public health authorities…Furthermore, the Centers for Disease Control did not separately tabulate cases of nonparalytic and paralytic polio until 1951 and did not require the reporting of polio cases until the late 1950s (Bruno, 2000).
And Humphries continues her callous dismissal of the cases of paralytic poliomyelitis:
Wild poliovirus was never the big killer or paralyzer the public was led to believe it was through the many frightening images shown repeatedly in the 1950s. Dr. Lennette, a well-respected virologist and pioneer of diagnostic virology with the California Department of Health, said in reflection on September 1987:
Actually, economically the disease wasn’t very important. Secondly, not many cases were seen in this country. There weren’t too many people paralyzed from polio in any one neighborhood, so it never made much of an impact (See also Graph 12.1.) (Humphries, p. 224).
For a little perspective, according to the National Cancer Institute, “Among children ages 0 to 14 years, it is estimated that 10,270 will be diagnosed with cancer and 1,190 will die of the disease in 2017 (National Cancer Institute, 2017). For Cerebral Palsy, according to the Texas Adoption Resource Exchange: “About 8,000 babies and infants are diagnosed with the condition each year. In addition, some 1,200-1,500 preschool age children are recognized each year to have cerebral palsy (Texas Adoption Resource Exchange, 2018). And as discussed below, approximately 4,531 new cases of Muscular Dystrophy are reported in the U.S. per year. According to the National League of Cities: “The most recent data from the U.S. Census Bureau (2007) counted 39,044 general purpose local governments, which includes 19,492 municipal governments, 16,519 township governments and 3.033 county governments (National League of Cities, 2018). Obviously, depending on one’s definition of neighborhoods, the number would be larger than the number of local governments. So, the likelihood of one, let alone more of any of the above in a neighborhood is small. Yet, many Americans were and are aware of them and support efforts, both research and care.
Humphries omits the paragraph preceding her quote from Hughes:
Yes, there were more people who went into the field because Roosevelt was dramatizing his incapacities—not intentionally—but he was dramatizing in the sense that, whenever he got up to get to the podium to speak, it was quite an effort on his part. He was really handicapped. And this gave people some awareness of what the disease was all about [my emphasis] (Hughes, 1982, p. 22).
So, Americans, even if not in their neighborhoods, were reminded of just how serious a condition paralytic poliomyelitis was as with other “low incidence” childhood diseases and disabilities. Keep in mind that from the 1916 epidemic on many neighborhoods had witnessed first-hand paralytic poliomyelitis. In Part 2 I will address whether FDR actually had polio or Guillain-Barré; but at the time people believed it and through the March of Dimes, the suffering many children were experiencing.
So, polio, with 7,000 documented cases of paralysis (see above) or more, should be dismissed as unimportant, I wonder which one of the above and many other disabilities and diseases affecting mainly children, given their “low incidence,” does Humphries also think we should ignore?
To summarize
Figure 1 from Humphries compares apples to oranges. Typhoid fever, caused by a bacterium, was basically eliminated by clean water and other public health measures. Malaria, a mosquito-borne protozoan, was ended in the US by mainly economic changes together with public health measures. Syphilis is still a problem because it depends on human behavior. Diphtheria began its decline, perhaps based on mutating to a more benign form, with, first, an anti-toxin and then a toxoid vaccine contributing to its further decline. Deaths from measles, a virus, were significantly reduced, reaching an asymptote of an average of 450 per year during the 1950s; but with a substantial amount of suffering, 45,000 hospitalizations, and up to 250 permanently disabled children. Smallpox deaths were reduced to under 1% in the United States, except imported cases, by a variant of the virus, although variola minor still entailed quite a bit of suffering, and, as long as variola major reigned in much of the world, the risk to Americans neither vaccinated nor exposed to variola minor still existed. Whooping cough (pertussis), caused by a bacterium, was reduced and almost eliminated in the United States by vaccines. In addition, while Humphries figure uses incidence, I think most people would care more about the degree of suffering, deaths, and disabilities. And ALL of the above, except syphilis began declining, some as early as the late 19th century. Though deaths from pertussis, measles, and diphtheria continued from the end of World War II into the early 1950s, they were lower than earlier and continued their decline, while polio was on the ascendance, including both deaths and disability. Despite changing definitions of paralytic poliomyelitis and errors in misdiagnosis, the majority of cases were correctly diagnosed and, actually, the total number of cases of those infected with polio virus was more than likely underestimated.
Why did the American people view polio with such fear
According to Oshinsky:
The disease reached its peak at the height of the cold war, when a national crisis often took the form of a crusade. And this particular crisis, an epidemic targeting defenseless children, grew to increasingly dramatic proportions in an increasingly suburban, family-oriented society preaching ever-higher standards of protection for the young. How ironic, how unfair, that polio seemed to target the world’s most advanced nation, where new wonder drugs like penicillin were readily available and consumers—mainly housewives—worked overtime to eliminate odors and germs.
No disease drew as much attention, or struck the same terror, as polio. And for good reason. Polio hit without warning. There was no way of telling who would get it and who would be spared. It killed some of its victims and marked others for life, leaving behind vivid reminders for all to see: wheelchairs, crutches, leg braces, breathing devices, deformed limbs (Oshinsky, 2005, pp. 4-5).
And Williams writes:
Polio outbreaks were smaller than the epidemics of classic scourges such as cholera and plague; but they came into their own while these time-honored killers were being seen off…The contrast between extinct threats and the new curse coming into its ascendancy appeared particularly stark from the 1930s onwards. Tried and tested public health measures were powerless to prevent polio. And this in turn made the sudden and unpredictable strike of polio, deep into the heart of homes that were now safely barricaded against other infections, all the more terrifying.
There was also the thorny problem of what polio might leave behind. Polio was not like other diseases such as diphtheria and whooping cough, with an all-or-none outcome for the battle for a child’s life. If the victims of those diseases survived, then everything was soon back to normal, and the episode could be safely written off as horrific, but history. By contrast, polio only rarely made a clean kill. Parents, family, friends and schools could move on after the death of a child, but it takes a special kind of residence to cope with the emotional, physical and financial cataclysms of helping a child in a wheelchair or an iron lung to live a full and rewarding life. During the 1930s and 1940s, many parents were torn apart by those stresses, and many more prayed desperately that they would never be put to the test.
The great American epidemic of 1916 concentrated its wrath on the East Coast…Its impact far outlived the seven month attack. Anything that could bring New York City to its knees was bound to leave lasting scars on the American psyche, and the sheer magnitude of the assault was shocking, with 9,000 cases and 2,500 dead between July and December in the Metropolis alone (Williams, 2013, p.116).
One can actually find similar sentiments regarding polio much earlier as expressed by Ruhräh in 1917:
A disease may be feared on account of its causing death, but a disease which permits the patient to live in an enfeebled conditions is even more dreaded and its occurrence in a community makes a much deeper impression (Ruhräh, 1917, p. 97).
The March of Dimes
According to Humphries:
The March of Dimes campaigns …were …designed to impact human fear and emotion (Humphries, p.224).
Many doctors of the 1940s were aware that the pitchmen of the National Foundation for Infantile Paralysis (NFIP) and March of Dimes were responsible for the expanded terror that swept the nation (Humphries, p. 244).
According to Oshinsky:
Polio’s special status was due, in large part, to the efforts of a remarkable group, the National Foundation for Infantile Paralysis [the formal name for the March of Dimes], which employed the latest techniques in advertising, fund raising, and motivational research to turn a horrific but relatively uncommon disease into the most feared affliction of its time.
[However] This dread did not begin with the National Foundation. A growing pattern of epidemics—the worst occurring in 1916—had already drawn …notice in the press (Oshinsky, 2005, p. 5).
As explained above by Oshinsky and Williams, the fear of polio was already there, and, despite Humphries emphasis on incidence, the cases of death and, especially, the all-too-visible paralysis were on the increase.
The March of Dimes wasn’t the first private organization to seek funding for a disease. In 1904, the National Association for the Study and Prevention of Tuberculosis was founded; but an even earlier version, the Pennsylvania Society for the Prevention of Tuberculosis was founded in 1892. In 1907, the Association began their Christmas Seal campaign to raise money (Wikipedia. American Lung Association). “Christmas seals are labels placed on mail during the Christmas season to raise funds and awareness for charitable programs (Wikipedia. Christmas seal). Another, the American Sexual Health Association, was established in 1914.
This was a time before the U.S. Government became actively involved in funding a broad range of medical programs, though as early as the 1790s, the Marine Hospital Service provided care for sick and disabled men in the U.S. Navy and in the late 1870s, Congress allocated funds to investigate the causes of epidemics like cholera and yellow fever (Wikipedia. National Institutes of Health). And few people had medical insurance.
According to Rose:
During its first 20 years, the Foundation assisted over 335,000 individuals with polio in a patients aid program that covered medical, hospital, and rehabilitation expenses…Covered expenses included payment for physician services, inpatient and outpatient hospital costs, the transport of polio patients (local transport to hospitals and the Military Air Transport Services, or MATS, organized through the US Air Force), home care (including nursing care), orthopedic devices, and home medical equipment. Rehabilitation expenses often involved long-term home care and carried over from year to year beyond the addition of new cases…The Foundation claimed that it was “the only voluntary health agency in the US which conducts a nationwide program of financial assistance to patients in meeting the costs of care of a single disease.”
It is important to recall the direct aid to communities besides personal aid that might have been beyond the scope of personal appreciation by individual recipients. From the outset the NFIP had organized systematic epidemic relief in concert with public health authorities involving the dispatch of physicians, nurses, and epidemiologists to affected areas, with medical equipment and supplies, to cope with local polio epidemics. It had supported the helping professions intrinsically involved with after care: nursing, physical therapy, and occupational therapy (Rose, 2016, pp. 156-158).
And according to Van Riper:
[It] launched a vast training program for physical therapists … [AND] in 1946 came the establishment of equipment depots, strategically located throughout the country, from which apparatus, such as iron lungs, rocking beds, and hot pack machines, could be promptly shipped into epidemic areas (Van Riper, 1955, p. 141).
Table 6 (from Van Riper, 1955, p. 141):
Funds Provided by the National Foundation for Infantile Paralysis, 1938-1955
| Project | Amount | ||
| Research | $22,600,000 | ||
| Virology and epidemiology | $18,300,000 | ||
| Prevention and treatment of after-effects | $4,300,000 | ||
| Education | $22,700,000 | ||
| Professional education | $19,600,000 | ||
| Public education | $3,100,000 | ||
| Prevention | Including gamma globulin and vaccine | $22,500,000 | |
| Clinical studies and medical care | Including support of respirator centers | $9,500,000 | |
| Patient care | $203,600,000 | ||
As can clearly be seen in Table 6, only about 16% went to research and vaccine development, thus, approximately 84% to care, education, and equipment.
One example of the importance of the National Foundation is the major epidemic that swept through Hickory, North Carolina in 1944.
As Oshinsky describes it:
Surrounding hospitals were overwhelmed. “Like a tidal wave the plague swept through the Catawba River Valley,” Life magazine reported, “Youngsters with painful, useless limbs, some unable to swallow or scarcely able to breath, they came from mining villages up in the hills, mill towns in the valley, from outlying farms and urban centers.”
The foundation agreed to equip and staff a makeshift polio hospital, to be built by local residents…The plan was risky. It called for the people of Hickory to accept polio victims from across the state, bringing even more “germs” into a community already devoted by the disease. Epidemics produce few heroes. Indeed, as the local newspaper admitted: “Had grownups been stricken and not [our] children, everybody from the mayor to the street sweeper likely would have fled town.”
A call went out for volunteers. Hundreds showed up, “hiding the fear,” said one, “that had [us] quaking in our boots.” Merchant donated building materials made scarce by wartime rationing…Families loaned their electric washing machines and vegetables. Farmers trucked in meat and vegetables.
Orthopedic nurses arrived…and physical therapists …Most had been trained through grants provided by the National Foundation…Iron lungs, hydrotherapy tanks, and medical supplies were flown in from regional equipment depots set up by the Foundation.
Before closing its doors, the makeshift hospital had treat 454 patients…All told, the foundation spent about $400,000 during the epidemic and a far greater sum on the aftercare of the survivors (Olshinsky, 1905, pp. 69-71).
Just to repeat what Humphries wrote: “Given what a low-incidence disease it was, how did polio come to be perceived as such an infamous monster? This is a question worthy of consideration, especially in light of the fact that the rate was far less than other common diseases (Humphries, p. 213).”
A low incidence relative to many other disease, yes; but incidence is not the important factor, suffering, disability, and death are. For Humphries, after Greenberg’s adjustments for determining paralysis, after Brown’s laboratory analyses distinguishing polio case from others, what remained were a significant number of deaths and even more so, the ever-present specter of an ever increasing number of disabled children. Without the National Foundation, how would they have been cared for?
As a child, some of my favorite movies were with Dean Martin and Jerry Lewis. Starting in 1966, Jerry Lewis hosted a Labor Day Muscular Dystrophy Association Telethon that I remember well. The Muscular Dystrophy Association was founded in 1950 with hopes of gaining the American public’s interest. As the Wikipedia article shows, the amounts raised were substantial with several years exceeding $60 million dollars (Wikipedia. The Jerry Lewis MDF Labor Day Telethon).
According to Wikipedia:
Muscular dystrophy (MD) is a group of muscle diseases that results in increasing weakening and breakdown of skeletal muscles over time. The disorders differ in which muscles are primarily affected, the degree of weakness, how fast they worsen, and when symptoms begin. Many people will eventually become unable to walk. Some types are also associated with problems in other organs.
Prognosis depends on the individual form of MD. In some cases, a person with a muscle disease will get progressively weaker to the extent that it shortens lifespan due to heart and breathing complications. However, some of the muscle diseases do not affect life expectancy at all, and ongoing research is attempting to find cures and treatments to slow muscle weakness (Wikipedia. Muscular dystrophy).
A systematic review found the birth prevalence for Duchenne muscular dystrophy ranging from 15.9 to 19.5 per 100,000 live births (Ryder, 2017). During the first half of the 1950s, the United States had an average of 4 million births (Infoplease, 2018), thus, an average of 708 new cases of Duschenne’s muscular dystrophy per year, Currently, the total number of cases of the main types of muscular dystrophy in the United States is 51,300 with Duchenne’s comprising 8,000 of them (encyclopedia com, 2018). So, the total is approximately 6.4 times Duchenne’s, thus, extrapolating to the 1950s would give us approximately 4,531 cases per year. Lower than paralytic polio cases; but a substantial number.
Since Humphries obviously doesn’t approve of the March of Dimes, I wonder how she feels about the Jerry Lewis Telethon and other Associations raising money for a variety of medical conditions? Perhaps, she doesn’t think the public should be contributing to them, given their “low” incidence?
Estimates of probability of children permanently paralyzed
Humphries writes:
The CDC defines polio’s statistical paralytic rate and estimates that it is less than 1 in 100 for some sort of permanent paralytic syndrome…Prior to vaccination, Dr. Maurice Brodie reported that only 1 in 170 children with no antibody to polio became ill during epidemics. By these two drastically different risk estimations, you can see that statistics are not set in stone, nor are they necessarily a reliable indicator of risk (Humphries, pp. 239-240; see also: Brodie, 1936).”
Unfortunately, Humphries fails to understand that at the time Brodie conducted his study it was not known that polio consisted of three identifiable serotypes, so, the antibodies used in Brodies analysis probably recognized only one of the serotypes. In other words, many of the children who tested negative may well have had antibodies to one or both of the other serotypes. In addition, Humphries fails to understand that almost ALL studies of any specific medical area will find a range of statistics. In the case of polio, for instance, it would depend on time, place, sampling scheme, sample size for any lab estimates, and, of course, which of the serotypes exist or have existed. However, whether one needed to vaccinate 100 or even 200 to prevent one case of paralysis (Number Needed to Treat (Wikipedia. Number needed to treat), given the significant number of paralytic cases depends on whether one considers so many paralyzed individuals acceptable or not, especially given the documented safety of the vaccines (e.g., see Greenberg above; Note this will be discussed in more detail in Part 2).
Far more people harmed by polio than originally suspected
To repeat from the CDC Pink Book:
Up to 72% of all polio infections in children are asymptomatic. Infected persons without symptoms shed virus in the stool and are able to transmit the virus to others.
Approximately 24% of polio infections in children consist of a minor, nonspecific illness without clinical or laboratory evidence of central nervous system invasion. This clinical presentation is known as abortive poliomyelitis, and is characterized by complete recovery in less than a week. This is characterized by a low grade fever and sore throat.
Nonparalytic aseptic meningitis (symptoms of stiffness of the neck, back, and/or legs), usually following several days after a prodrome similar to that of minor illness, occurs in 1%–5% of polio infections in children. Increased or abnormal sensations can also occur. Typically these symptoms will last from 2 to 10 days, followed by complete recovery.
Post-polio syndrome
According to Wikipedia:
Post-polio syndrome ( PPS, or post-poliomyelitis syndrome or post-polio sequelae) is a condition that affects approximately 25–50% of people who have previously contracted poliomyelitis—a viral infection of the nervous system—after the initial infection. Typically the symptoms appear 15–30 years after recovery from the original paralytic attack, at an age of 35 to 60. Symptoms include acute or increased muscular weakness, pain in the muscles, and fatigue. The same symptoms may also occur years after a nonparalytic polio (NPP) infection [my emphasis].
The most widely accepted theory of the mechanism behind the disorder is “neural fatigue”. A motor unit is a nerve cell (or neuron) and the muscle fibers it activates. Poliovirus attacks specific neurons in the brainstem and the anterior horn cells of the spinal cord, generally resulting in the death of a substantial fraction of the motor neurons controlling skeletal muscles. In an effort to compensate for the loss of these neurons, surviving motor neurons sprout new nerve terminals to the orphaned muscle fibers. The result is some recovery of movement and the development of enlarged motor units.
With age, most people experience a decrease in the number of spinal motor neurons. Because polio survivors have already lost a considerable number of motor neurons, further age-related loss of neurons may contribute substantially to new muscle weakness. (Wikipedia. Post-polio syndrome; see also: Halstead, 1998; Halstead, 2011; Horowitz, 1985; March of Dimes, 2001; McComas, 1997).
Studies have found clear evidence of polio virus in sufferers of post-polio syndrome (e.g., Leparc-Goffart, 1996).
Not only those who suffered paralysis, going through often long painful therapies, who appeared to have regained somewhat normal mobility, eventually only to develop post-polio syndrome; but a number of those, who following an acute episode of polio, even those asymptomatic, also developed post-polio syndrome. As discussed by Bruno:
Many clinicians, even some who treat polio survivors, believe that individuals who had nonparalytic polio (NPP) cannot develop postpolio sequelae (PPS), which include fatigue, muscle weakness, joint and muscle pain, cold intolerance, and difficulty sleeping, swallowing, and breathing and which occur more than 30 yr after acute poliovirus infection. The common wisdom is that NPP is synonymous with “abortive polio,” in which the poliovirus caused a flu-like illness but did not enter the central nervous system (CNS) and, therefore, neither damaged nor killed neurons. Autopsies, of course, were not performed on humans diagnosed with NPP to determine if there was damage to the CNS. However, there is significant circumstantial evidence that NPP was associated with CNS damage. For example, it was reported in 1953 that 39% of those diagnosed with NPP had measurable weakness on manual muscle testing in at least one muscle group. A 1954 study documented that 89% of polio survivors who were acutely “persuasively nonparalytic” had “very definite muscle weakness” as much as 3 yr after the diagnosis of NPP.
Recent studies make clear that NPP survivors do have late onset symptoms. A population-based study of 828 polio survivors found that new muscle weakness and fatigue were reported, respectively, in 38% and 34% of those who had been paralyzed and in 14% and 21% of those who had had NPP
Therefore, “postpolio syndrome” should not be used as the generic descriptor for late onset problems in polio survivors, because its diagnostic criteria exclude those without a history of paralysis, electromyographic evidence of denervation, and new muscle weakness. (Bruno, 2000; see also: Falconer, 2000, Nee, 1995).
Table 7 (Table 2 in Bruno, 2000) gives the limitations in paralytic and non paralytic polio survivors compared with all Americans (%).
| Paralytic polio | Nonparalytic polio | All Americans | |
| Limited in life activities | 42 | 29 | 19 |
| Limited in ability or unable to perform major activities | 32 | 18 | 13 |
| Limited in ability or unable to work | 27 | 16 | 11 |
Bruno, quoting David Bodian, writes:
The average number of spinal cord neurons that are destroyed by the polio virus is almost 50%. However, nonparalytic polio may be associated with severe neuron damage in the spinal cord. What is more, some with non paralytic poliomyelitis do not have damage in the spinal cord but have characteristic damage in the brain, which is more extensive than in some who did have paralysis. All available evidence shows conclusively that every case of polio exhibits damage in the brain. The polio virus is capable of producing an encephalitis, with or without symptoms (Bruno, 2002, p. 20).
Bruno writes:
The poliovirus is remarkable in its ability to invade neurons. In the 1940s Johns Hopkins University pathologist David Bodian found that 96 percent of motor neurons were infected by the poliovirus if you had any paralysis at all! Given the ability of poliovirus to enter and damage such a large percentage of neurons, why doesn’t everyone infected with poliovirus become totally and permanently paralyzed? Bodian found that for each neuron the polio virus invades, commandeers, and destroys, its action is halted in another neuron that is then able to rebuild its severely damaged protein-manufacturing and protein-packaging factories and start functioning again. How is it that the poliovirus is stopped at least half the time? Most likely because the immune system is able to play catch-up and produce enough antibodies to attack the poliovirus before it conquers the entire nervous system.
But if on average 50 percent of all motor neurons are destroyed in anyone who had paralytic polio, why aren’t half of polio survivor’s muscles paralyzed? Bodian discovered that at least 60 % of spinal cord motor neurons associated with an individual muscle must be killed before the muscle shows any weakness at all. This means that muscles that were at one time paralyzed or muscles that have been weak, may have been operating on as few as 40 percent of their original motor neurons…What’s more, Bodian found that muscles thought to be completely unaffected by polio—muscles that had never been weak, let along paralyzed—only have 60% of their motor neurons (Bruno, 2002, p. 29).
What’s more, Bruno makes a case that, besides post-polio syndrome, that chronic fatigue syndrome may have the same pathophysiology (Bruno, 1997; Bruno, 1998).
So, the 1/100 to 1/200 ratio that describes the immediate aftermath of acute polio infection significantly underestimates the “true” extent of polio’s damage. Many cases of slight muscle weakness were missed and later those suffering from post-polio syndrome, both originally asymptomatic and symptomatic, and, perhaps, even chronic fatigue syndrome, were the result of the polio virus.
Humphries writes:
After the vaccine, there was a concerted effort to distinguish cases with poliovirus from cases without it. This was not a concern prior to 1958 when many diseases common today hid behind the name poliomyelitis. Transverse myelitis, viral or aseptic meningitis, Guillain-Barré syndrome (GBS), chronic fatigue syndrome, spinal meningitis, post-polio syndrome, acute flaccid paralysis (AFP), enteroviral encephalopathy, traumatic neuritis, Reye’s syndrome, etc., all could have been diagnosed as polio prior to 1958 (Humphries, p. 224).
As discussed above under subtitle: Polio morbidity/paralysis, after Greenberg’s adjustments for determining paralysis, and using the same criteria together with laboratory differential diagnostics in Brown’s study, a significant number of cases of paralytic poliomyelitis remained. And neither post-polio syndrome nor chronic fatigue syndrome were known entities until decades later, so how could they be diagnosed as polio prior to 1958? As I will discuss further in Part 2, as I mentioned above, though misdiagnoses exist in most, if not all aspects of medicine, a significant number of cases of paralysis were determined to have been caused by the polio virus. And, as discussed above, Humphries appears unaware that not only did the polio virus cause immediate cases of disability; but has been found to have resulted in “mild” effects on many during their lifetime and later disabilities, even those who did not initially appear to have been affected. Humphries seems unaware of just how much damage to neurons polio virus did.
Summary and conclusion
I think it obvious that Humphries presentation is defective in numerous ways and displays a callousness towards suffering:
- Humphries begins by comparing incidence rates for a number of diseases, essentially comparing apples to oranges;
- When Humphries does discuss disease incidence and deaths, she ignores the tremendous toll polio has in terms of suffering and disability, something she does as well with measles;
- Humphries ignores that all the diseases she compared with polio were either basically already eliminated or on a sharp decline at the same time polio was on the rise;
- Humphries doesn’t seem to understand the basics of estimates, that is, there is often a range; but whether 1/100 or 1/200 cases actually became paralyzed, still, when one counts up the actual number of cases of paralyses, makes little difference. And Humphries fails to understand that a 1936 estimate would have been made prior to establishing that polio was three distinct serotypes;
- Humphries dismisses that even after Greenberg’s adjustments, that 7,000 or more cases of paralysis remained;
- Humphries misuses the Michigan data, which actually found “among the 242 patients originally diagnosed as paralytic, 187, or 77% were confirmed by laboratory tests to have poliomyelitis. The vast majority of these (84%) were found to have residual paralysis 60 days after onset of the illness.” Thus, 65% had paralysis 60 days later, based on criteria used by Greenberg;
- And, though, as exemplified by Greenberg and the Michigan study, changing definitions and mistakes in differential diagnosis, Humphries ignores the fact that the actual number of people reported to have been affected by the polio virus is a significant underestimate, and that many suffered mild decrements in ability during their lifetimes, and later post-polio syndrome and, possibly, chronic fatigue syndrome.
- Humphries ignores the cultural changes in the US, having survived the Great Depression and been victorious in World War II, with many previous diseases eliminated or on the decline, with the miracle of antibiotics, starting families, confronted with an ascending disease, one that visibly affected children, unpredictable and, yes, frightening.
- Humphries opinion of the March of Dimes discounts both that people already experienced fear regarding polio and the major role the March of Dimes played in helping polio victims, help that is doubtful would have come from elsewhere. Her hostility to vaccines blinds her to the fact that the vast majority of March of Dimes funds went to patient care, training of nurses and physical therapists, and medical supplies. And, by implication, Humphries probably would dismiss various organizations soliciting funds for numerous other “low incidence” diseases and conditions; and
- Humphries ignores post-polio syndrome and, possibly, chronic fatigue syndrome, where studies have found the former and, perhaps, the latter actually a result of damage caused by the polio virus, not misdiagnosed as polio.
Though I think this paper alone makes a compelling case that Humphries lacks credibility, I like to be thorough, so I will be working on subsequent papers. As now planned: Part 2 will focus in more depth on definitions/criteria for paralysis, lab confirmation, when and what types, and differential diagnoses and the role the vaccine played in the disappearance of polio; Part 3 will focus on the Cutter Incident, vaccine-associated polio, the role of tonsillectomies and provocation from other medical injections, and claims by Humphries that DDT and arsenic played a significant role, SV40 vaccine contamination, and discuss the Central Dogma that polio resulted from improved sanitation, together with other variables that partially explain the ascendance of polio; and Part 4 will focus on treatments, including the iron lung, surgeries, immobilizations, various physical therapies, and nutritional approaches. Basically, I intend to demonstrate that Humphries is completely wrong (intentionally or not) about every point she so feebly tries to make or that she grossly exaggerates, grossly overgeneralizes, and emphasizes ancient history. Based on her approach she would basically negate most of modern medical science. Stay tuned!
Acknowledgements
For valuable feedback and suggestions, thanks to: Sandi Berman; David W. Rose, MA; Dorit Rubinstein Reiss, PhD; Steven A. Rubin, PhD.