You may have heard about a recent abstract submitted to the American Heart Association sowing doubt in regards to the safety of the COVID vaccinations based on the results of a blood test. I as a pediatric and adult congenital cardiologist, am here to advise you that this abstract doesn’t mean what you think it means. To understand the context behind this abstract, several puzzle pieces of knowledge are required.
Levels of evidence
While the American Heart Association is one of my professional organizations, whose members are mainly cardiologists and cardiac surgeons, not everything they produce is the highest level of evidence, and this has always been this way. For anyone who has not attended an AHA scientific session, you will hear cardiologists debate the most controversial topics in the field and get very passionate about their sides of the argument. If you have never experienced cardiology before, you would rightly wonder whether these cardiologists know anything at all about their work. What you will not hear though, is a cardiologist able to overturn cardiac physiology or fundamental principles in the field. For example, we will always have newer ways to treat coronary artery disease, however it is an absolute impossibility for anyone to overturn the fact that aortic valve stenosis will eventually need to be treated if it is severe enough. The fact that a big atrial septal defect in a teenager needs to be fixed, will never be overturned. The best kinds of new insights about cardiology will take into account existing knowledge while expanding our knowledge about areas of the heart that aren’t as well studied. The things discussed at scientific conferences are uniquely the topics that are at the fuzzy edge of the known and unknown.
How do we sort out what evidence is best? The levels of evidence that we rely upon in cardiology are similar to the levels of evidence in other clinical fields:

Picture credit: Golden & Bass, 2013
An abstract falls in the “Case Series and Case Reports”/”Expert Opinion” category. An abstract can be created by anyone who wants to introduce their research project, and it has the lowest peer review requirement. I, as a lowly first year cardiologist, can also produce an abstract about anything that I want to write about. It takes considerably more teamwork, with peer review, to write something like a clinical practice guideline or a meta-analysis of randomized controlled trials.
Plaques and heart attacks: Some basic considerations
It is known in cardiology that having high cholesterol strongly influences your risk of heart attack, however, there is not a 1:1 relationship. There are people out there who control their cholesterol very well, and still suffer from heart attacks. Conversely, I have personally seen children with severely elevated cholesterol who do not have heart attacks. There is an inherent difference in plaques (the actual lesions that cause heart attacks when broken); some are more prone to fall apart and create a heart attack (a “vulnerable plaque”), and some are more stable, leaving the people with these plaques mostly unaware of their presence. Considerable effort has been devoted to figuring out why some plaques are more dangerous, and others less so. The current state of the science of the vulnerable plaque focuses on using different types of imaging to identify them in the arteries of the heart, using artificial intelligence and fluid dynamics. This debate is still an area of much research to this day, and the latest research has in fact discovered that most vulnerable plaques when ruptured, do not create heart attacks. Further, plaques that rupture and heal may actually contribute to coronary narrowing rather than themselves generating heart attacks. For all these reasons, the science of detecting which plaque will create the heart attack is still advancing.
What is the PULS test?
The world of laboratory science has put forth many blood tests to try to identify the more dangerous plaques, and one of these is the PULS (in some journals referred to as CADPA). It is a relatively new lab test by GD BiosciencesTM designed to test several proteins naturally present in the body with a goal of improving risk-based stratification of patients with coronary artery disease (the classic heart attack).
The biomarkers measured by the PULS test include:
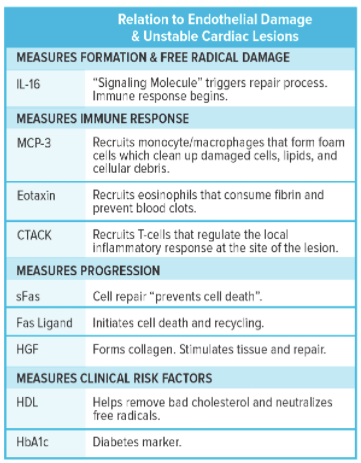
Picture credit: GD Biosciences
A score is then compiled that estimates the risk of heart attack in the patient. While the score is the subject of some promising research, and draws its validation from seminal studies in Cardiology (ADVANCE, Orentreich, PMRP-Marshfield, and MESA), it is not standard of care in every cardiology office because more validation is required before it can be elevated to the level of a clinical practice guideline. A clinical guideline is the highest level of guidance for cardiologists that informs items such as the sequences of medications used to treat a brand new heart attack or how to place a heart stent.
What is the nature of this study?
The author of the AHA abstract is a cardiac surgeon turned holistic health practitioner, and based upon review of his website and this abstract he appears to frequently do PULS blood tests. He tested samples of some patients’ blood using PULS before and after vaccination, and compared the results. The actual data analysis, based even upon review of the abstract, is unclear. The PULS data from two patients are presented in the abstract, and the author concludes that the cardiac risk of the patients is therefore elevated. He also recommends that people take aspirin and quercetin to mitigate their post-vaccination risk of cardiac issues.
What are the methodological flaws of the study?
In this type of study, at the bare minimum, a statistical analysis of the subjects and comparison to controls is expected, to see if the intervention (in this case the vaccine) created an effect that can be demonstrated to be different from people who did not receive the experimental intervention. This was not explicitly demonstrated anywhere in the abstract. An abstract is the most basic level of science that can be submitted to the American Heart Association, so this appears to have flown under the radar of peer review (abstracts are subjected to a relatively low level of peer review). If the author intends for readers to understand the risks of COVID-19 versus vaccination, the more complete thing to do is to compare the much bigger, and much more deranged, immune response of COVID disease to the immune response to COVID vaccination. There were also no efforts to compare the immune response in COVID vaccination to the response shown in classical adult booster vaccines such as influenza or pneumonia. Most importantly, if you run a test designed to search for inflammation after a procedure designed to generate temporary inflammation, you will find inflammation. Macrophages, T cells, eosinophils, and collagen remodeling are expected responses after any infection. He also stated that aspirin and quercetin might benefit the user if taken after vaccination. There is no evidence provided in the study to show they decrease your inflammatory markers after vaccination. Furthermore, the PULS test was never validated with vaccinations.
Members of the antivax ecosystem will never tell you this – the only way they can promote their views is to take studies out of context and overstate the risks. There is no evidence that will change their minds. Rather, they look for any shred of evidence that validates their pre-existing biases and ignore nuance, context, or contradictory evidence. By contrast, a responsible clinician or scientist is prepared to change their mind once sufficient evidence arises to challenge existing beliefs.
What is a better way to interpret this article?
Because this is so important, it bears repeating – if you run a test designed to search for inflammation, after a procedure designed to generate temporary inflammation, you will find inflammation. This is similar to saying if you drive 100 kilometers, you will expect to find the petrol tank to be lower at the end. The decreased petrol level is not an indictment on the safety of the petrol tank.
I do not wish to discount the experiences of those who have experienced genuine heart attacks after COVID vaccination because I know these people exist. However, it is crucially important to realize that the preconditions of the heart attacks were already there. One of the most common ways to discover a heart attack is through “minding your own business”, not knowing you almost had a deadly problem. One of my previous professors, who thankfully survived, discovered his coronary artery disease in this way, while shoveling snow. Coronary artery lesions are a complex interplay of atherosclerosis, inflammation, high cholesterol, stress, and genes. The vaccination did not place the coronary artery lesions in the patient. If the heart attack had happened 2 days before the COVID vaccination, it would have been deemed unrelated. Because some heart attacks have happened after COVID vaccination, it is easy to deem them related when this is not necessarily the case. Should patients find out their coronary artery status prior to COVID vaccination? This is too costly to be applied to the entire world. However, if you are interested in determining if you have coronary lesions prior to vaccination, you are welcome to do so. Know that doing this will find a lot of people with no heart artery issues.
The abstract is at best, in my opinion, potentially useful in guiding the ongoing investigations into postvaccine myocarditis, but only in the hands of trained immunologists and cardiologists. This abstract is too widely misinterpreted, and those who profit from disinformation are only too happy to use this work to advance their cause. A basic rule of research is to not overstate your conclusions when your project doesn’t have the data to support those conclusions. This abstract as submitted, essentially wants to show vaccines have more risk than was previously reported. This has been repeatedly demonstrated to be false by many centers. The abstract also fails to take into account that patients with coronary artery disease are amongst those who suffer the worst outcomes if they experience COVID. On this basis alone – people with heart failure and coronary artery disease in fact, need COVID vaccination the most (this is a known comorbidity increasing severity of COVID disease). Only hearing about the risks is an unbalanced assessment. Discussions of vaccine safety must always place the risks into the context of the very significant benefit they provide to adults, even (or especially) those with pre-existing coronary artery disease.