I’ve reached the age in my life where my joints have started making odd noises – all of a sudden my knees sound like Rice Krispies, which WebMD reassures me is clearly imminent osteoarthritis. At least I’ll have company, as osteoarthritis (OA) affects nearly everyone, once you get old enough. It’s the most common form of arthritis, and treatments are focused on reducing symptoms, as osteoarthritis is incurable. Anti-inflammatory drugs like ibuprofen and naproxen are commonly used to treat the pain associated with OA. They can be effective, but there are also safety concerns with the use of anti-inflammatory drugs. Non-steroidal anti-inflammatory drugs (NSAIDS) have been linked to about 30% of drug-related hospital admissions, and it’s estimated that 12,000-16,000 Americans die annually as a result of gastrointestinal bleeding caused by NSAIDs. They can also cause significant kidney damage in up to 5% of users. Drugs like acetaminophen (Tylenol) are also used commonly but the efficacy of acetaminophen has been questioned, and this drug can be fatal in overdose. With questions about the safety and efficacy of commonly-used drugs to treat OA, there is persistent interest in the use of supplements and other forms of alternative medicine, perhaps based on the perception that these products are safer and potentially as or more effective than “conventional” therapies. A recent paper in the journal Rheumatology summarizes the conclusions of systematic reviews and randomized controlled trials of a variety of herbal products and dietary supplements, and is a helpful guide to inform self-selection and decision-making.
Understanding osteoarthritis
Osteoarthritis is a common debilitating condition of synovial joints. These joints make up most of the movable articulations of the body and are characterised by an articular capsule and synovial lining that surrounds the fluid-filled synovial cavity. This fluid functions somewhat like motor oil, acting as the joint’s lubricant. The opposing ends of the two articulating bones are lined by cartilage which acts like a shock absorber and reduces friction between bones. If you sample a piece of cartilage and observe it under a microscope, you’d see cells called chondrocytes bathing in a matrix composed of collagen fibers, a substance rich in proteoglycans and elastin fibers. Now these proteoglycans are themselves composed of a protein bound to glycoaminoglycans (GAG) – a chain of repeating carbohydrates compound (e.g., hyaluronan). The role of proteoglycans is to act as binding force in articular tissue. GAGs include chondroitin, heparin, and keratan.
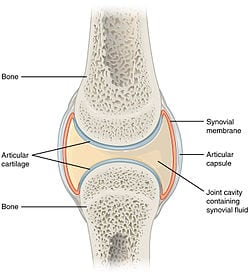
Source: Wikipedia
Although its cause is not well understood, osteoarthritis seems to be caused mostly by articulation “wear and tear”, such that nearly everyone by age 70 has some degree of OA. Other factors for OA include genetic inheritance, behavior influences, and obesity. Chronic pain in the knee, hip, fingers and of the lower back are typical symptoms of osteoarthritis. After injury (e.g., trauma or repetitive joint overuse), changes start to occur in the joint itself. First, cartilage cells start to change their metabolism and cause an overall depletion in proteoglycan that leads to damage to the collagen matrix. Then the cartilage swells and loses its ability to absorb joint pressure. As a consequence of cartilage loss, the bone surfaces of the articulation start to wear off which result in deformed bone structures of the joint. Pain from OA is activity-related, with onset during or just after joint use, and then gradual resolution. In the early phase of the condition, pain is episodic and happens after a day or two of overuse of the affected articulation. In severe OA, pain can be continuous. Occasionally, morning stiffness can occur, typically resolving within 30 minutes. While some patients may have physical changes in the joint – particularly joint space narrowing – that can be seen on x-rays, a diagnosis of mild to moderate OA is usually based on a physical examination only. If you’re older than 25, have persistent joint pain in a few joints, and morning stiffness, it’s probably osteoarthritis.
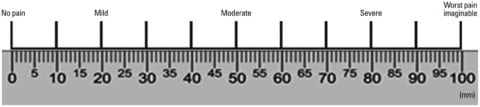
The important and measurable outcomes in OA are global pain as measured by a visual analog scale (VAS), pain function as measured by the WOMAC or the Lequesne Index, and occasionally, joint space narrowing (JSN) as measured using x-ray imaging. As the physical changes seen on x-rays do not accurately predict the severity of symptoms, most trials use pain outcomes as clinically important outcomes to evaluate.
A new review of the evidence
This new paper, published in Rheumatology and entitled “Which supplements can I recommend to my osteoarthritis patients?, is from Xiaoqian Liu and colleagues. The researchers sought out randomized controlled clinical trials and systematic reviews for commonly recommended supplements and “complementary” medicines. Eight systematic reviews and nine RCTs were identified, meaning a total of 16 products were included in the review. The researchers estimated the treatment effect size based on the standardized mean difference where an SMD of up to 0.3 was considered small, 0.3 to 0.8 was moderate, and >0.8 was considered large. The minimum clinically relevant difference was estimated at 0.37 which correlates with a difference of about 9mm on a 100mm pain scale. We use the terms “clinically important” or “clinically relevant” to try to distinguish between changes that are meaningful to patients, and those that are likely not. For example, if you rate your pain a 70 today and a 66 tomorrow, that’s not likely to be clinically meaningful.
The researchers also utilized the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to rate the quality and strength of the evidence, which you’ll see below. A bubble diagram provides a simplified summary of the evidence suggesting which products may be effective and which should be avoided. The bigger the bubble, the higher the rating.
The results
Here’s a summary of what the review found.
Marine omega-3 fatty acids
Fish oils (e.g., cod liver oil), krill oil and products like green-lipped mussel extract have been studied for 6-26 weeks with no evidence of effectiveness, based on low-quality evidence.
Glucosamine
Harriet Hall has written about glucosamine regularly. Despite extensive investigation, glucosamine hasn’t been shown to have any convincing meaningful effects, a finding made by this review team as well. This non-effectiveness is consistent across the different forms of glucosamine (sulfate vs. hydrochloride). Glucosamine, however, appears safe.
Chondroitin sulfate
This is another supplement that Harriet Hall recently revisited. This review noted that a Cochrane review found superiority to placebo, but the clinical significance was unclear. Another, subsequent systematic review concluded that chondroitin had no clinically important effects. It was found to be safe, however. The review also noted that combination glucosamine + chondroitin is also ineffective in terms of reducing joint pain or functional impairment in knee pain over six months.
Vitamins D and E
Four studies have evaluated vitamin D supplementation for treating OA. The durations ranged from 1-3 years with doses ranging from 800-2000IU per day to 50-60000IU per month. No clinically meaningful effect on pain or function has been shown.
Vitamin E has also been evaluated at doses of 500IU for 6 months to 2 years, with no effect on symptoms but it was associated with a higher risk of bleeding.
Collagen
Collagen is a protein, and it’s claimed that consuming it will decrease cartilage degeneration by promoting collage synthesis. When we consume collagen, usually in the form of food, the long chain proteins are broken down during digestion to their original amino acids. There are inconsistent signs of benefit and of unclear clinical importance with collage hydrolysate. Undenatured collagen (derived from chicken sternum cartilage) has been evaluated in two clinical trials for 90-180 days and has been shown to be more effective than glucosamine + chondroitin, or placebo.
Willow bark extract
This is akin to impure, raw aspirin (acetylsalicylic acid) as the raw ingredient of willow bark (salicin) was later used to develop ASA and other anti-inflammatory drugs. A systematic review gave conflicting results in OA, and other trials have shown no effect. (Whether or not this is due to the inconsistent presence of active ingredients is always a question I have with these products.) Adverse effects include gastrointestinal effects, and if this is truly just a raw, unstandardized NSAID, we should expect the same cardiovascular side effects as well.
MSM (Methylsulfonylmethane)
While in-vitro testing suggests that MSM may have inflammatory effects, and MSM is very popular as a supplement, the treatment effects are promising, but not convincing. One systematic review found positive “but not definitive” evidence of a treatment effect compared to placebo. A second systematic review found modest to large treatment effects when used for 12 weeks, though the quality of the evidence was low. Optimal dosing isn’t clear, and the product can cause mild gastrointestinal discomfort.
Avocado and soybean extracts
Avocado/soybean unsaponifiables (ASU) (i.e. extracts) are made of one-third avocado oil and two-thirds soybean oil. Low quality evidence suggests that ASU might have moderate effects in the short-term, but these effects were not observed with more rigorous evaluations. ASU seems to be as well tolerated as a comparable placebo.
Turmeric /curcumin
I’ve written about this product before, which has promising anti-inflammatory effects. The main pharmacological challenge with curcumin seems to be that the product is poorly absorbed. Manufacturers have come up with several different formulations (e.g., nanoparticles, liposomes) but there’s not a lot of high-quality evidence to go on. Like other supplements, what appear to be large treatment effects are complicated by overall poor quality evidence. While curcumin seems to be well tolerated, this is one supplement that may cause interactions with prescription drugs like anticoagulants (“blood thinners”).
Boswellia serrata
Boswellia is a gum resin extract from the frankincense tree. Several potentially active ingredients have been identified with anti-inflammatory effects. Three studies have evaluated two different Boswellia products in knee OA that found clinically meaningful treatment effects on pain and disability improvement. However, the quality of that evidence was evaluated to be low. While it appears to be well tolerated, it has been reported to cause abdominal pain, fever, and weakness.
Pycnogenol
Pycnogenol is an extract of the maritime pine made up of a concentrate of plant polyphenols, and is claimed to have anti-inflammatory effects. Three studies (of moderate quality) that have evaluated the supplement have found large and clinically meaningful effects for pain and disability. No serious side effects have been reported.
Rose hip
Rose hip is another herbal remedy which has anti-inflammatory properties. It has been studied against placebo in three studies with a duration of 3-4 months. A meta-analysis found small to moderate short-term effects for pain reduction, and a subsequent RCT found no effects. Rose hip was as well tolerated as placebo.
Making sense of the studies
Based on their review, the authors do not recommend omega-3 fatty acids, vitamins D and E, willow bark extract, collagen hydrolysate, glucosamine, chondroitin, combinations of glucosamine and chondroitin, and rose hip. Based on the review, Boswellia serrata extract and pycnogenol appear to demonstrate the most clinically important effects. They also note that while curcumin and MSM demonstrated clinically important effects, the quality of that evidence was low. The authors comment that the overall evidence base remains limited by poor-quality studies, often of short duration, with many sponsored by manufacturers (particularly small studies that showed large effects), noting the following priorities for future research:
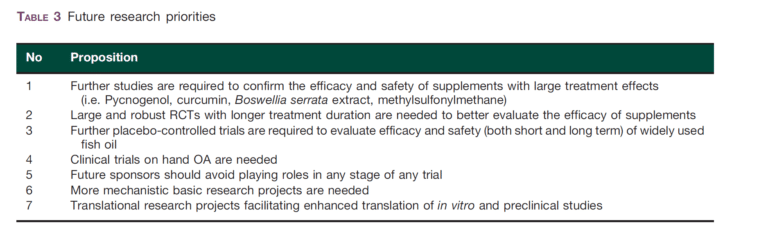
They summarize the evidence, and their overall evaluation, in this figure:
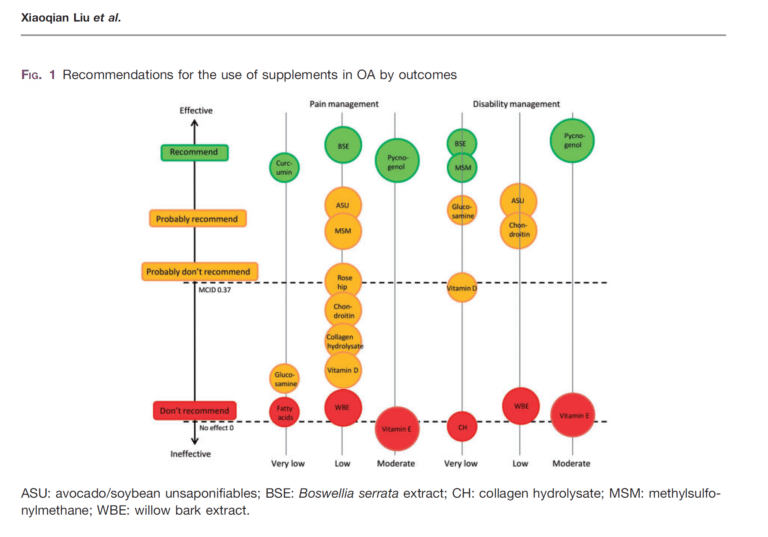
The authors conclude that in those with osteoarthritis who are enthusiastic about using supplements, short-term trials of the pycnogenol, curcumin, Boswellia serrata extract, or MSM could be attempted, and should be discontinued after 4-6 weeks if no obvious benefits are noted. Importantly, drug-supplement interactions are not always well understood or well documented, and any supplement should be used with caution (and preferably, consultation with their pharmacist) if being combined with prescription or non-prescription drugs. There are also the very real concerns about supplement quality and batch-to-batch consistency, which complicates evaluations of risk and determining whether or not they work.
Making sense of supplements for osteoarthritis
Given the ubiquity of osteoarthritis and the lack of really good treatment options, it’s worth noting what has been shown to work: Ongoing exercise and weight loss (where appropriate) is backed by moderate-to-high quality evidence and a moderate effect size. This is a benefit that is comparable to anti-inflammatory drugs, but without the cost or the side effects. There are also topical anti-inflammatory drugs, which appear to provide meaningful benefits without the typical NSAID-related side effects.
For those who have exhausted the established options, supplements may look appealing and some may be worth a short-term trial. It’s important to remember that with studies of supplements and drugs alike, as the quality of evidence improves, the treatment effects often diminish or disappear. Still, based on the existing evidence, for your own evaluation it seems reasonable to try products for which there is the best evidence. This is an area where the evidence continues to emerge, so if you’re experiencing OA, cautious skepticism about the “latest and greatest” supplement seems to be reasonable.