I’m sorry, did I break your concentration?
As so often happens at Science Based Medicine, the inspiration for today’s post comes from a reader of the blog, seeking evidence-based advice and references after receiving conflicting (and perhaps even contradictory) information from other sources. On one hand, it saddens me when people get bad advice from health care professionals or elsewhere, whether it’s from their “regular” doctor, an “alternative” practitioner, or from Dr. Google; on the other hand, the fact that well-meaning patients are seeking out science-based recommendations through Science Based Medicine is encouraging and emphasizes the important role this blog serves.
The email that was referred my way was written by a man who is considering having a tooth extracted in the hopes that it will alleviate some general health issues he is having. He writes:
May I request that you write an article refuting the claims made in the book “Toxic Tooth — How a Root Canal Could Be Making You Sick”?
The purpose of my request is that I am considering getting a root canal pulled out.
After an initial back and forth where I told him that I’d look into it and to meanwhile not do anything hasty, he related his general symptoms (all correspondence reprinted with permission):
My personal information is I am a ** year old male, and I have a lot of fatigue. MDs are not able to tell me why. I have a TSH of 12. MDs are not able to tell me the root cause. I have Monocytes of 13, normal range is 4-13, this means I have an infection. This makes me wonder if maybe that root canal is the cause of that infection.
To translate (very superficially and simplistically): His TSH (Thyroid Stimulating Hormone) level is elevated. TSH is a hormone released from the pituitary gland and helps regulate the thyroid hormones which are involved in the body’s cellular metabolism. Normal values are in the 0.3–3.0 µIU/mL in an adult, and an elevated TSH usually means that the patient has an underactive thyroid (hypothyroidism). On rare occasions, it can indicate the presence of a thyroid tumor or other uncommon issues. His monocyte level is a bit elevated as well, which could mean the presence of a chronic infection or perhaps an auto-immune disease, but that lab value alone is not enough to make that call. But I’m just a dentist; what do I know?
Could his fatigue and abnormal lab values be attributed to the presence of his endodontically treated tooth (i.e. a tooth that has had root canal therapy)? Let’s look into the science of it and come back to that question at the end of my article.
This particular fellow seems to have done some research. His email went on to give me a link to a Mercola article where the author of the aforementioned book was interviewed and claimed that root canal therapy consistently leaves bacterial by-products behind, resulting in chronic infection with serious systemic sequelae. To the lay person, these claims can be very convincing and seem frightening, and inadvisable decisions (such as having perfectly healthy teeth extracted) can result from believing these dubious assertions. I am very grateful this person emailed us with his inquiry. He isn’t feeling well, is presumably doing his due diligence (although I question that he only sent me links from alternative medicine sources and not from science based sources), and wants to make the right health care choices so that he can begin to feel better. But what is the right choice and why?
If you’ve ever sat in the dental chair with that lovely powder blue paper bib clipped around your neck and have been told you need a root canal, you know how sphincter-puckering that news can be. After all, root canal therapy is right up there with kidney stones, epidural-free childbirth, and bank bail outs in the pain and agony department, or so the story goes.
I am going to over-simplify and over-generalize here, so please forgive me. If you want greater detail on pulp (i.e. nerve) pathology and the intricacies about the procedure itself, you can read about it here. I just want to give you the basics so that you will have a context from which to understand the false and fraudulent claims that are being made.
Normal tooth anatomy
Before we can cover tooth pathology and subsequent treatment (as well as treatment options), we have to review the anatomy and physiology of a healthy tooth.
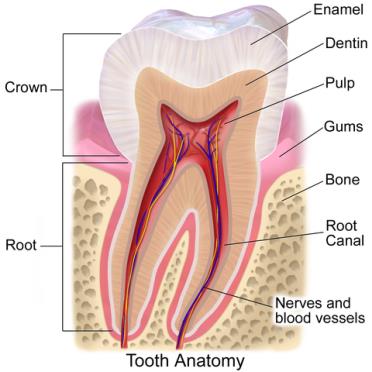
Source: Blausen.com staff. “Blausen gallery 2014”. Wikiversity Journal of Medicine. DOI:10.15347/wjm/2014.010. ISSN 20018762
As you can see in the above diagram, the part of the tooth that you can see, called the clinical crown, is covered by enamel, an extremely hard, mostly inorganic material that protects the tooth and allows you to chew just about anything. Under this 1-1.5mm protective shell is the dentin (or dentine if you’re outside the US) which is softer and contains tubules that radiate outward from the pulp (or nerve). These tubules contain fluid and cellular extensions of the pulp. The core of the tooth is the pulp, which contains blood vessels, nerve tissue, and other cells. The part of the pulp that travels down the root to connect with the systemic nerves and blood supply is called the root canal.
If the nerve is irreversibly damaged (by tooth decay or trauma, for example), it will “die” and become necrotic. Eventually the space where the pulp used to dwell will be colonized by bacteria, causing the dreaded “abscessed tooth.”
Root canal procedure
Ok, now we find ourselves with an abscessed tooth. Again, there are other reasons and scenarios where endodontic therapy may be needed, but this serves as a good primer, as the process is pretty much the same in most situations. So you’re sitting in the chair, powder blue paper bib clipped around your neck, sphincter puckered, ready for the dreaded procedure.
In a nutshell, here’s what happens next: your tooth is numbed up, and your dentist prepares your tooth for the root canal by drilling out any decay and gaining access to the pulp chamber (the “core” where the live pulp used to be). Having gained access, your dentist will identify the canal(s) that traverse down the root and commence to cleaning and shaping them out with small metal files. These files are typically nickel-titanium these days, and can be either hand held or rotary files (i.e. in a handpiece). Think of them as specialized bottle washers that go down to the end of each canal to remove the necrotic debris, bacteria, and other gunk that’s in there. During the procedure, the dentist will irrigate the tooth and canals with a disinfectant, usually sodium hypochlorite (household bleach), to help remove the debris and kill any remaining bacteria that are present within the tooth. When all this is completed, he or she then seals the canals with a synthetic rubber-like material called gutta percha in order to prevent recurrence of the abscess. Sometimes antibiotics and/or pain medications are prescribed to assist with post-operative care.
Within a short period of time, the tooth feels normal again, and after being restored with a filling or crown, it can function normally with an excellent success rate, which is estimated at around 90% according to one systematic review.
What happens when a root canal goes south on you? Sometimes the tooth can fracture beyond repair, especially if it doesn’t have a crown on it (for most cases on back teeth; often front teeth don’t need crowns), resulting in extraction. In other situations, the tooth itself can become re-infected, causing a new abscess. This can be detected and diagnosed based upon clinical signs and symptoms, x-rays, and other diagnostic tests. When this happens, the tooth needs to be treated as quickly as possible to prevent pain, the spread of infection (including cellulitis and sepsis, both of which can be life threatening), and/or compromising the health of adjacent teeth. In many cases, these endodontic flare-ups can be retreated and the tooth be saved; other times the tooth is lost.
Risks, costs, and alternatives
Believe it or not, root canal therapy isn’t for everyone or every tooth. Like every medical and dental procedure, there are pros and cons, risks, and costs involved. First and foremost, root canals ain’t cheap. Fees vary, but you can expect to pay $800-1,500, depending on geographic location as well as which tooth it is (a single-rooted front tooth is easier to treat and thus less expensive than its multi-rooted wisdom toothed counterpart). Insurance often picks up a sizable percentage of the fee, so that can be factored in if you happen to have good dental insurance.
Some of the risks of endodontic treatment include:
- If the damage is too extensive, the tooth may be not be able to be saved, even if the abscess is eliminated.
- Although rare, it is possible for the files to perforate the side of the root, or a file may separate (break) inside the tooth. Both of these complications can be managed, but worsen the long term prognosis of the tooth.
- Undetected fracture in the root can lead to failure of the procedure, resulting in the loss of the tooth.
- Other rare complications such as an allergic reaction to materials being used, local anesthetic, etc.
Sometimes, a root canal isn’t practical, even if the prognosis is excellent. For example, if a tooth is in the very back of your mouth, and it has no opposing tooth to bite against, many people choose not to spend the time and money to save a tooth that is non-functional. If a patient has multiple other needs, or isn’t able or willing to maintain his or her dental work with good oral hygiene, good dietary habits, and regular preventive dental visits, then sometimes it’s not advisable to spend the time and money on a tooth that very likely will be lost in a short time anyway.
So what are the alternatives to root canal therapy? What happens if there is a fracture or an abscess, but the patient is either unable or unwilling to undergo root canal therapy, or if root canal therapy is contraindicated, or the prognosis is poor? Sadly, extraction is the only alternative in cases like this. Infections won’t spontaneously resolve, even with antibiotics, until the source of the infection is removed. This can be by just removing the dead, infected nerve with a root canal (as described above), or removing the whole tooth. We as dentists hate it when a patient loses a tooth, but sometimes that is the prudent thing to do, whether it is for biologic, pragmatic, or financial reasons.
The first option a patient has, believe it or not, is to do nothing. While for most people, most of the time, replacing a missing tooth is the best thing to do from a function, comfort, and cosmetic standpoint, it’s not necessary. Most people typically get by just fine with all, some, or none of their teeth. That being said, there can be consequences to not replacing a tooth, such as other teeth around the missing tooth shifting or tilting into the empty space.
If a patient wants to replace one or more missing teeth, there are three broad options that he or she can consider. Because this post isn’t about how to restore mouths, I’ll just give a brief overview with even briefer pros and cons of each:
- Removable partial denture. Pros: cheapest option, no surgery or “grinding down” of other teeth. Cons: It’s a prosthesis, taken in and out. Not as strong, comfortable, or natural looking.
- Fixed bridge. Pros: Natural looking (when porcelain or zirconium), “permanent”, strong. Cons: More expensive, you have to prepare (grind down) the teeth on either side of the space. More difficult to clean under.
- Implant and crown(s). Pros: Natural looking, no preparing of adjacent teeth. Cons: More expensive, surgical procedure, more time consuming.
When a root canal becomes a woo-t canal
I apologize for that long and boring preamble, but it was necessary so that I could set the table for the rest of this article; namely to outline some of the fear-mongering and outright misinformation that some alternative sources (including dentists and physicians, sadly) are posting online and elsewhere. Unfortunately, because of the plethora of bad information as well as frequent cross referencing and circle-jerking type linking, often this pseudo-dental information pops up at the top of search engines, confusing the lay public and directing them down paths where they should not go. As a science based dentist who fights “Dumb Disease and Truth Decay” (thank you Evan Bernstein for that horrible, horrible pun!), I want to try to set the record straight and give sound dental information so that people (in concert with the advice and counsel of their dental provider) can make informed choices based upon sound scientific evidence and which are consistent with their values, wishes, and budgets.
The overarching theme when it comes to the “alternative” or “holistic” criticism of root canals comes down to the claim that no matter how well the root canal procedure is performed, there are still bacteria and bacterial toxins left in and around the tooth, which then ostensibly continues to infect the patient, causing a host of maladies, from heart disease to diabetes to cancer. One of the authors (Dr. Thomas Levy) of the above referenced book Toxic Tooth — How a Root Canal Could Be Making You Sick stated in an interview that “there can be few things as catastrophic as a root canal.” Considering that an estimated 15 million root canals are performed each year, I’m surprised that people who have had root canals (including me 20 years ago) haven’t all dropped dead. That doesn’t sound catastrophic to me. Unlike the way I described the root canal procedure above, Dr. Levy (a cardiologist, not a dentist) described the procedure as one where the “life force” of the tooth is removed and then is subsequently “embalmed.” Dr. Hal Huggins, the notorious “Father of Quack Dentistry” who lost his license for “gross negligence and other professional misconduct” for promising patients that taking out their amalgam fillings would cure their MS and other diseases, compares an abscessed tooth to a ruptured appendix. “If you have a ruptured appendix, are you going to fill it with wax and crown it?” asks Dr. Huggins incredulously. Even Mercola says that after a root canal, “(u)nder the stresses of oxygen and nutrient deprivation, these formerly friendly organisms morph into stronger, more virulent anaerobes that produce a variety of potent toxins. What were once ordinary, friendly oral bacteria mutate into highly toxic pathogens lurking in the tubules of the dead tooth, just awaiting an opportunity to spread.” The only thing this statement informs us of is Sloppy Joe’s total lack of even a basic understanding of microbiology or physiology.
Let’s talk about some of the main anti-root canal memes circulating around.
First, we’ll start off with a doozy that has been circulating around the World Wide Woo for some time. Several alternative medicine peddlers have this headline plastered across their pages:
97% of Terminal Cancer Patients Previously Had This Procedure
Of course, they are talking about root canals, and I don’t even know where to begin in trying to debunk this claim. NOTHING about it is even remotely accurate or true. (If you have a strong stomach and want to read the entire article, do so at your own peril by clicking here.) Suffice it to say that there is no scientific literature that even hints to this conclusion. In fact, one study showed that people who had a history of tooth decay and endodontic treatment actually had a reduced risk of head and neck squamous cell carcinoma, for what that’s worth. Allegedly, a “Dr. Robert Jones” studied this phenomenon, and his research is what is passed around and cross linked. The problem is, no one really seems to know who this mysterious Dr. Jones is or what his primary research says, if it was ever published. Searches on PubMed and Google Scholar yielded nothing. If any of our astute readers could let me know where to find him or his work, I’d greatly appreciate it! Even Snopes weighed in on it and seems as baffled as I am about it. I think we can all agree to dismiss this ludicrous claim out of hand; it’s not worth the virtual paper it’s written on.
The other two phenomena associated with root canals are not as far out as the above cancer scare association, and deserve mentioning. The first centers around the term NICO. No, I’m not referring to the German actress/model/singer who sang on the Velvet Underground’s amazing debut album; rather, I mean Neuralgia-Inducing Cavitational Osteonecrosis, which is decidedly less cool than the Velvet Underground. NICO is a small area of necrotic (dead) bone, which creates small spaces in the jaw. They are difficult to diagnose, can create atypical pain patterns, and tend to recur. While the cause of NICOs is still unknown, they are sometimes associated with old extraction sites, trauma, and have been linked with autoimmune and clotting disorders. That being said, the American Association of Endodontists (AAE) have stated in their position paper that “(d)ue to its indefinite disease characteristics with unclear etiology and pathogenesis, there have been growing doubts regarding whether NICO is a distinct disease entity.”
The reason I bring up NICOs is that, even if it turns out to be a real “thing,” the alt-medders have co-opted the term in much the same way as chiropractors have co-opted the term “subluxation”, which is a real thing in medicine, but is meaningless in the context of chiropractic philosophy. The anti-root canal faction uses NICOs as a reason to eschew and condemn endodontic therapies; they claim that most if not all root canals create NICOs, which then can “seed” the body with infection and toxins. They claim that they can detect NICOs by seeing them on x-rays or by use of some E-Meter-like device which purportedly can detect them. When found, a “biologic” dentist will want to remove the NICO by curetting out the lesion, then treating with some wonder poultice like ozone or colloidal silver, in addition to chelation therapy and IV vitamin C therapy. This is, of course, invasive, risky and expensive theatre with no proven benefit. Unproven treatments for non-existent pathologies. Any reader of the SBM blog will recognize that pattern, as it applies to so much to what alternative practitioners of all stripes do on a daily basis. Even Aetna weighed in on the matter and penned a rather thorough review of NICOs and basically said there was little evidence of their legitimacy, the methods of diagnosis were unproven and suspect, and treatments would not be covered due to their “experimental and investigational” status.
There are so many areas of this topic I could talk about and would like to talk about, but to do so would require a blog post of Gorski-esque dimensions, and I just don’t have that sort of attention span. So I’ll wrap this up with a discussion of the claim that bacteria from the mouth are a cause of many systemic diseases. Jumpin’ Joe Mercola claims that root canals can cause a veritable smorgasbord of problems, including, but not limited to: heart disease, kidney disease, arthritis, joint, and rheumatic diseases, neurologic diseases (including ALS and MS) and autoimmune diseases (including lupus). That’s quite a grocery list, and he even left out cancer! Despite the typical fear-mongering found on websites like this, the link between oral pathogens and systemic disease is a valid and science based observation, and warrants further discussion. Research is ongoing, but it does appear that there is a correlation between periodontal (gum) disease and such diseases as heart disease and diabetes. Whether this is a causative link remains to be seen, but we can’t dismiss this connection summarily as pure woo propaganda. The problem is that once again, the “woolistic” dentists have extrapolated research in one area (endodontics) into another area (periodontics), then have claimed that the bacteria from root canals travel to the coronary arteries to cause the formation of atherosclerotic plaque. This tortures the existing data and takes it to places it has no business being, and that brings me to my final point.
All of the claims made in the persecution of root canal therapy state or imply that a tooth which has undergone endodontic therapy is a cesspool of residual infection, but that’s not the case. If the procedure is carried out properly, however, the infection is for all intents and purposes eliminated; any bacteria or bacterial products which may remain fall well below the threshold for causing any sort of local inflammation or infection. And if that is the case, the likelihood of it causing any systemic diseases is very low indeed. To this end, the AAE has a web page outlining the literature on root canal safety which is thorough and informative. It addresses the issues we’ve discussed here as well as many more. Please give it a good looking over if you want good information.
Conclusion: Another patient led astray
Circling back to the email I received from the man inquiring as to the possible connection of his root canalled tooth to his feelings of fatigue and abnormal lab values. After exploring the literature, but admittedly without examining him or being privy to his lab tests, I can generalize my professional opinion thus:
- If there is any correlation between his feeling of fatigue, his elevated lab values, and his root canal, then it is because his root canal is failing.
- If his root canal was failing, it most likely would be symptomatic, with pain and/or swelling present. Any dentist could diagnose that situation, and an x-ray would most likely show evidence of pathology.
- A healthy, successful root canal would not cause his issues.
- Assuming his endodontically-treated tooth was done properly and is now healthy and functional, removing it would not improve his systemic status, and now he would be left with a missing tooth to show for it.
Obviously, I can’t diagnose him or give specific information, but based upon the current scientific literature combined with my 30+ years of experience, I can tell you with a high degree of confidence that he has been led astray by alternative practitioners. It is my hope that he and others like him will not fall for the scare tactics and poor science that these purveyors of woo peddle.

