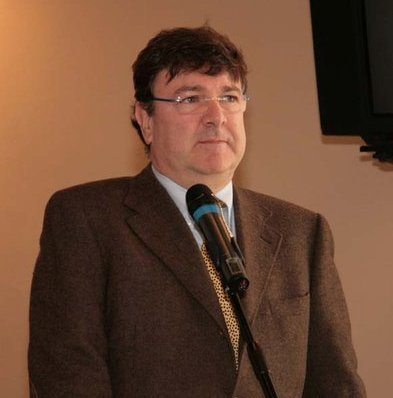
Paolo Zamboni, the originator of the unproven idea that multiple sclerosis is caused by occluded blood vessels.
Peter Lipson reported Monday about new research suggesting that multiple sclerosis may be caused by venous blockage. He correctly characterized some of the hype surrounding this story as “irrational exuberance.”
This is a phenomenon all too common in the media – taking the preliminary research of an individual or group (always presented as a maverick) and declaring it a “stunning breakthrough,” combined with the ubiquitous personal anecdote of someone “saved” by the new treatment.
The medical community, meanwhile, responds with appropriate caution and healthy skepticism – “this looks interesting, let’s see some more research.” There is a reason for such a response from experts – experience.
We have been here before – lithium for ALS
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease that results in the death of motor neurons, leading to weakness and ultimately paralysis or death. There is currently only one proven treatment for ALS, a drug called riluzole, and its effects are modest – prolonging tracheostomy-free survival by 2 months on average. So new treatments are welcome, to say the least, and there is ongoing research looking for possible treatments.
In February of 2008 I wrote about a preliminary study by Italian researcher, Francesco Fornai, in 44 patients with ALS, showing a dramatic improvement in outcome. This research followed a mouse study that also showed significant improvement.
Press reporting about this “breakthrough” research resulted in patients with ALS and their families contacting me and other neurologists asking how they could get treated.
Meanwhile, the reaction of the ALS research community was cautious but hopeful. It was felt that this preliminary research deserved further study, but was not enough to conclude that lithium was effective or to start treating patients with it.
The North East ALS Consortium (of which I am a member, although I did not participate in this study), based upon Fornai’s research, performed a randomized controlled multi-center trial of lithium in ALS. The results were dead negative – so negative that the trial was stopped early due to futility.
Here we have animal studies and preliminary human trials showing a dramatic improvement, and a follow-up larger and better controlled study showing zero effect. How do we reconcile these results?
Simple – preliminary data is unreliable, by definition. Most new ideas in medicine do not pan out. And as a result (and as John Ioannidis has taught us) most published studies are wrong. What are reliable are later, larger, more definitive trials, and specifically a consensus of results in the peer-reviewed literature after a question has had time to simmer and mature.
Zamboni and CCSVI
It should therefore be no surprise at all that the medical community is once again taking a cautious approach to preliminary research published by a single researcher claiming dramatic results from a revolutionary new idea. As Peter discussed, Dr. Paolo Zamboni, a neurosurgeon, believes he has found a cause and a cure for multiple sclerosis (MS) – a neurosurgical one.
Just like with lithium and ALS, his idea is an interesting one, and his preliminary data deserved to be taken seriously – which means replicating his research and doing follow up studies. He claims that patients with MS – 100% of the MS patients he has studied, but none of the controls – have blockages in the veins that drain blood from the brain. These blockages lead to blood backing up in the brain, which causes iron deposits, which results in inflammation and MS.
At this point there are many possibilities. It’s possible Dr. Zamboni is the victim of confirmation bias (I am always suspicious of 100% results) and his new condition – chronic cerebrospinal venous insufficiency or CCSVI is an illusion.
It is possible he has found a real pathological marker for MS but what he is seeing is the result of MS, not the cause of it. Inflammation is known to follow the venous system in MS, but there are explanations for this that have to do with the immune system in the central nervous system. Perhaps chronic inflammation from MS causes sclerosis in the veins and the blockage that Dr. Zamboni is finding.
If this is true then it is possible that the venous sclerosis is playing no or only a minimal role in MS pathology, and fixing them by opening them up with balloon angioplasty is of no benefit. It is also possible that even though the venous changes are cause by auto-immunity in MS, once they form they worsen the clinical syndrome, and treating CCSVI in MS will improve outcome, even if it does not cure the underlying cause driving the disease.
And it is possible that Dr. Zamboni has discovered the, or an, underlying cause of MS – that CCSVI is actually the primary driver of the disease. Or perhaps it just triggers the auto-immune response, but once triggered it is self-sustaining.
This is a huge range of possibilities, and it is definitely premature to come to the most extreme conclusion among them. We need time for the MS community to pick over Zamboni’s claims and research. While we do not know what ultimately causes MS, we have decades of high quality research characterizing its pathophysiology. How does this research square with Zamboni’s claims? Let’s wait and see.
Zamboni’s basic claims need to be replicated. And if warranted, clinical studies need to fully characterize the risks and benefits of any procedure to address alleged CCSVI. Perhaps it only has benefit is a sub-population of MS. Maybe it makes the disease worse. We won’t know until quality studies are done.
I am not holding my breath, just as I wasn’t with lithium for ALS, but I will certainly follow the research. I would love for Zamboni to be correct – if we can essentially cure MS with a one-time procedure that would be a huge boon to MS patients and save billions.
Help – the media is not being irresponsible!
The most absurd reaction to Zamboni’s research came from The Huffington Post. As Peter reported, Erika Milva wrote a rambling piece suggesting that the cautious responses of American media, MS societies, and the medical community were due to being risk-averse and the omnipresent (in the fantasies of many) Big Pharma conspiracy.
Milva could not understand why the media was not irresponsibly jumping over this story and hyping it, as some of the foreign press has. So I guess she decided to make up for this with maximal hysteria of her own.
But there is no mystery here. Zamboni’s claims are radical, and therefore by definition improbable. But more importantly, they are preliminary. That doesn’t mean they are wrong – it just means we do not yet know. Let’s wait for some quality research.
And that is one of the primary differences between science-based medicine and everything else – basing treatments on evidence, withholding judgment until reliable evidence is in, and not overreacting to every pilot study that pops up.
I will let you know in a couple of years how Zamboni’s claims have turned out.

