Myocarditis 101
With recent reports of myocarditis after vaccination in young people after the mRNA vaccines, it is worthwhile to reexamine the risk/benefit ratio of these vaccines in this population. First let’s start with what is known about myocarditis in this population.
Myocarditis is inflammation of the heart muscle, and pericarditis is inflammation of the pericardium (outer lining of the heart). It can be caused by a wide variety of infectious agents, toxins, or as part of an autoimmune condition. It typically presents with chest pain and shortness of breath. Patients typically have ECG abnormalities and elevated serum troponin levels, a marker of cardiac injury. Myocarditis is more common in young men and can be quite serious depending on the underlying cause.
How has the COVID-19 vaccine affected children and young adults?
The CDC conducted a risk-benefit analysis and reported data from two vaccine-safety monitoring systems: The Vaccine Adverse Event Reporting System (VAERS) and the Vaccine Safety Datalink (VSD). Each of these two databases has their own strengths and weaknesses. According to the CDC, “VAERS accepts all reports from everyone regardless of the plausibility of the vaccine causing the event or the clinical seriousness of the event”. This makes VAERS useful to rapidly detect potential vaccine side-effects that may be rare. But anyone can file a report, and even in the case of well-intentioned reports, it is not possible to establish cause and effect. Antivaxxers abuse this database frequently, as David Gorski has described many times. Of course, many side effects go unreported as well. My children felt tired for a day after their vaccines and had sore arms. I didn’t report this to VAERS. However, most clinicians would know to report a serious outcome like myocarditis, and I find it unlikely that there is a very large number of young people with the condition going undetected by the CDC.
In contrast to VAERS, the VSD surveys nine participating integrated healthcare organizations covering 12 million people. It is a public health surveillance activity that “Monitors a limited set of prespecified vaccine safety outcomes”. It is “Designed to detect statistically significant associations and statistical signals (values above specified statistical thresholds), which do not necessarily indicate a safety problem”. This database is not public as it contains confidential patient information.
Each of these databases has collected information on myocarditis after the mRNA vaccine. Based on data from VAERS, after approximately 300 million doses of the mRNA vaccine, the following numbers were reported:
- 1,226 total myocarditis cases.
- 267 myocarditis cases were reported after the first dose. The median age was 30 years and 66% were male. The median time to symptom onset 4 days.
- 827 cases after the second dose. The median age was 24 years and 79% were male. The median time to symptom onset was 3 days.
- 132 cases after occurred after an unknown dose.
The risk of myocarditis increased with decreasing age and was more common in males. According to VAERS reports:
- For males age 12-17 years, the risk after the second dose is 66.7 per one million, or 1 in 14,992.
- For males age 18-24 years, the risk after the second dose is 56.3 per one million, or 1 in 17,761.
- For males age 25-29 years, the risk after the second dose is 20.4 per one million, or about 1 in 49,019.
From the VSD, the rate of myocarditis was reported as a group for people age 12-39 years only and only goes through June 5th, perhaps before many adolescents received their second vaccine dose. According to VSD reports:
- For people age 12-39 years, the risk after the second dose is 12.6 per one million, or 1 in 79,365.
- For males age 12-39 years, the risk after the second dose is 32.0 per one million, or 1 in 31,250.
- For females age 12-39 years, the risk after the second dose is 4.7 per one million, or 1 in 212,765.
Most importantly, the outcomes for these cases has been favorable thus far. Most cases of myocarditis can be successfully treated with pain and anti-inflammatory medications. Some have required no treatment at all. The CDC reviewed 484 preliminary reports from people 29 year or younger detected via VAERS. Of these 323 met the definition of myocarditis and/or pericarditis and 148 are under review. Of these 323 cases:
- 309 (95.6%) were hospitalized.
- 295 (95.4%) have been discharged.
- 218 (79%) recovered without symptoms.
- 5 (1.5%) were lost to follow-up.
- 9 (2.9%) remain hospitalized, two in the ICU.
In their report of 29 confirmed cases from VSD:
- 22 (75%) were admitted to the hospital for a median of 1 day (range 0-13).
- 2 (5.7%) were admitted to the ICU.
- All were discharged home.
- Nearly all follow-up visit notes indicated resolution of symptoms at the time of follow-up.
- Of those that had follow-up, the ECG, echo, lab testing, most had returned to normal or baseline.
Other studies also report a good prognosis. A study of 7 teenagers ages 14-19 years noted that all “resolved their symptoms rapidly”. During a “clinician call” with the Infectious Disease Society of America and the CDC, it was noted that these patients were admitted for cardiac monitoring and all were hemodynamically stable, something that seems true for almost all cases so far. Two studies (Larson et al and Rosner et al) of 15 adult men with vaccine-induce myocarditis reported favorable outcomes. Another case series reported on 23 men age 20-51 years in the military with myocarditis, after more than 2.8 million doses of the vaccine. All patients had significantly elevated troponin levels, which is evidence of cardiac injury. Fortunately, “All patients received brief supportive care and were recovered or recovering at the time of this report”. 16 had recovered fully, while 7 had “chest discomfort” at the time of the report.
Doctors who have treated and authored case series on these patients agree on the favorable outcome so far. Dr. Pei-Ni Jone, a pediatric cardiologist said, “The good news is, all these children recovered”. Dr. James de Lemos, a professor of medicine, said, “They’ve all done well” and all recovered clinically after spending “just a couple of days” in the hospital. Most were not very sick or required ICU care. Affected people may be advised to limit vigorous activity for 3-6 months and long-term monitoring will continue. A warning about myocarditis is now part of the FDA Fact Sheet about the vaccine, which is of course necessary.
In summary, the highest risk is for vaccine-induced myocarditis is in males ages 12-17 after the second vaccine dose, though it is not a common event. According to a statement by the American Heart Association, “The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination”. The vast majority of affected individuals are admitted to the hospital, though for a brief time. Though some people were monitored in the ICU, almost all cases have recovered without symptoms or seem on the road to recovery. Vaccine-induced myocarditis is rare and serious, permanent consequences seem rarer still.
This is all very good news, but care should be taken to not minimize these cases by focusing on the low rate and good outcomes, as is often done with the effects of the virus on young people. A rare outcome multiplied by millions of people can add up to a non-trivial number. Myocarditis is potentially a very serious, even fatal, condition. It’s serious anytime a young person gets admitted to the hospital, even if they leave after a few days feeling well, as most seem to do. Affected individuals may have felt quite sick, and it must have been a very scary experience for them and their families. It is also not a small thing to for a young person to have to avoid vigorous activity for 3-6 months. Though there is every expectation that these people will continue to remain well, this is not guaranteed, and they will have to be monitored over time. Additionally, more cases will come to light as awareness of the condition grows, some with potentially less favorable outcomes.
How has COVID-19 affected children and young adults?
Now lets’ look at how COVID-19 has affected young adults and children. According to data from the CDC, the number of confirmed cases is:
- 0-4 years: 576,162
- 5-17 years: 2,805,814
- 18-29 years: 6,088,943
As this represents confirmed cases and is likely a substantial underestimate of the true number of infections, the CDC has made the following estimates for COVID-19 cases:
- 0-4 years: 4,466,773
- 5-17 years: 22,203414
- 18-49 years: 55,616,991
- Assuming that people ages 18-30 years account for an equal share of the cases, this translates to about 21.5 million infections for this age group.
The CDC reports the following deaths:
- 0-4 years: 155 (1 in 29,000 cases)
- 5-17 years: 316 (1 in 68,000 cases)
- 18-29: 2636 (1 in 8,150 cases)
- 316 of these deaths occurred after 4/1/21
Multisystem inflammatory syndrome in children (MIS-C) is a serious condition affecting the GI tract, skin, and heart caused by COVID-19 (discussed by Clay Jones over a year ago). Importantly, MIS-C can cause myocarditis. As of June 2, 2021:
- 4,018 MIS-C cases had been reported to the CDC, though this may be a substantial undercount as many cases have gone unreported.
- 36% of cases were in persons aged 12–20 years.
- The estimated incidence of MISC-C is 1 in every 3,164 SARS-CoV-2 infections.
- 60%–70% of patients with MIS-C are admitted to intensive care, 1%–2% die
As I discussed in a previous article, an accurate count of the hospitalizations for young people is difficult to obtain. There are many ways in which hospitalizations can be undercounted, as not all hospitalizations are reported to government agencies. According to some studies, hospitalizations have also been overcounted by up to 45%, as incidental infections have been included in many tallies. One study, which excluded incidental COVID-19 infections, found the hospitalization rate for COVID-19 in teens was triple that of the flu. Regardless of the exact number, at a minimum, tens of thousands of children have been hospitalized due to COVID-19. Quite plausibly, this number is well over 100,000 people, especially if young adults under 30 years are counted. Children with underlying risk factors such as obesity are at the highest risk of hospitalization. A consistent finding in several studies of hospitalized children is that some can be quite sick. In two studies (Kim et al and Havers et al) one-third need ICU level care and 5-6% need to be intubated. This is an important distinction that must be considered when comparing hospitalizations from COVID-19 with those from vaccine-induced myocarditis.
Of course, COVID-19 can affect children who are not ill enough to be hospitalized. Even among the vast majority of children who do fully recover, some were nonetheless quite really sick for a long time. Estimates from the UK are “that 12.9% of UK children aged 2 to 11, and 14.5% of children aged 12 to 16, still have symptoms five weeks after their first infection”. Another study found that 4.4% children had illness duration ≥28 days, while 1.8% of children experienced symptoms for ≥56 days. While these rates are relatively low, when multiplied by the millions of children who have had COVID-19, this results in a large number of really sick children. Extrapolating these numbers to the US, it means that 500,000 children have had symptoms for two months or more. Other studies fortunately, found lower rates of persistent symptoms.
There are currently more questions than answers as to how COVID-19 might affect children over the long-term, but we should be humble and consider the virus may have complications that we cannot appreciate now. Though the clinical implications are not clear, a study from the UK recently found evidence of brain injury on imaging. Importantly, this study compared scans from people before and after their infections.
What does COVID-19 have in store for children and young adults?
Pandemics are moving targets and the past is at best a rough guide for the future. Predicting the future has made fools of many thus far, especially those who declared herd immunity had arrived months ago in the US. There are factors that make the future for young people more optimistic and factors that make it more pessimistic. In trying to tease these out, I will do some “back of the envelope” calculations and estimates.
On the optimistic side of the ledger, 46.1% of Americans have been fully vaccinated. The CDC estimates that there have been 114.6 total million infections, or that 34% of Americans have been infected. This immunity (both from the mRNA vaccines and virus) seems to be long-lasting, though only time will tell for sure. As there is likely considerable overlap between these two groups, perhaps 70% of Americans have immunity to COVID-19 at this point, though no one knows the exact number. This will form a significant barrier that will prevent COVID-19 from overwhelming cities and hospitals again, especially as the most vulnerable people are the most protected. COVID-19 cases have fallen to a low-point since the start of the pandemic, as have deaths and cases of MIS-C. This is great news. The vaccines work wonderfully, and COVID-19 hospitalizations and deaths occur essentially only in unvaccinated people today, which is not great news.
On the negative side of the ledger, the US is still averaging over 10,000 cases and nearly 300 deaths per day, numbers that seem low only because they are compared with much higher numbers from six months ago. 53.9% of Americans have not been fully vaccinated, and 18 states have vaccinated 40% or fewer of their residents. Among the 18,000 COVID-19 deaths in May, only 150 were in fully vaccinated people. Again, the vaccines really work. The number of vaccine doses delivered daily in the US has steadily decreased since its peak in mid-April. Currently, the USA is averaging only about 900,000 doses per day, and despite great outreach efforts and incentives, the number is likely to continue to decline. Likely the vaccine curve has already peaked for young people most at risk for myocarditis as well. Many people simply do not want to be vaccinated. Many of these people will be hard to convince and they are often not taking steps to prevent themselves from getting infected. According to news reports from rural Missouri,
Nobody’s wearing masks or practicing social distancing. They believe right-wing media’s lies that COVID is “just like the flu” or “vaccines are experimental” or “it’s all a Democrat hoax.” They’re following Trump’s notion that masks make men look “weak.”
Some governors have worked to undermine vaccine efforts, forbidding state agencies or private business from requiring vaccines as a condition of entry. This includes large states, namely Florida and Texas. Sadly, low vaccine rates will prevent many states from reaching the herd-immunity threshold, which will likely be higher than previously thought due to the Delta variant. COVID-19 is spreading in states with low vaccination rates:
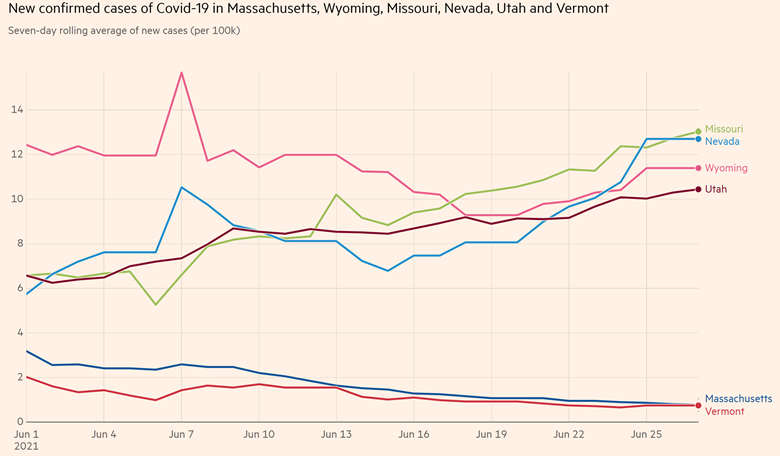
COVID-19 case rates are climbing in Missouri, Nevada, Wyoming, and Utah, in comparison to the declining rates in highly vaccinated Massachusetts and Vermont
Of course, herd immunity is not a state-level phenomenon, and the degree of immunity can vary greatly from neighborhood to neighborhood even within a city. Moreover, young people tend to travel and congregate together.
Most concerning is the emergence of the Delta variant (discussed by Steven Novella last week), which seems up to 60% more contagious than even other COVID-19 variants, which were themselves more contagious than the original virus. According to news reports from Australia, infections have occurred after “encounters of roughly five to 10 seconds between people walking past each other in an indoor shopping area in Sydney in at least two instances”. Queensland’s chief health officer, Dr. Jeannette Young said “with the Delta variant, we’re seeing very fleeting contact leading to transmission. At the start of this pandemic, I spoke about 15 minutes of close contact being a concern. Now it looks like it’s five to 10 seconds that’s a concern. The risk is so much higher now than it was only a year ago”. Obviously this is not scientific proof. Hopefully we’ll know more definitive information about this soon, but several cities in Australia recently announced a lockdowns as a result of this variant. Similar lockdowns are being imposed in several Asian and African countries where this variant is surging. Some American cities that seemed to be through the worst are again encouraging masks.
Outbreaks of the Delta variant have affected children in highly vaccinated countries such as Israel and the UK. It accounts for about 20% of new infections in the US, more than twice what it was two weeks ago. According to some reports, “It is responsible for half of new cases across a swath that includes Missouri, Iowa, Kansas, Nebraska, Colorado, Montana, North Dakota, South Dakota, Utah and Wyoming”. This variant seems to cause worse outcomes as well. According to data from Scotland, the hospitalization rate is nearly twice as high due to the Delta variant and it was most commonly found in younger people. Fortunately, the vaccines still offer solid protection, especially against severe disease requiring hospitalization.
Some who opposed the Emergency Use Authorization for the mRNA vaccine for children counted on high vaccine update in adults obviating the need for the vaccine in young people. Unfortunately, this was always more of a hope than a plan. Though COVID-19 cases are at a low-point today, a similar dip was observed last summer before the nightmare that engulfed the US in the late fall and winter. The current decrease in hospitalizations is due to immunity in older people, not younger people. Indeed, according to the CDC, “COVID-19 associated hospitalization rates have remained stable in adolescents and young adults”.
Given the low vaccine-uptake in large swaths of the country and the emergence of the Delta variant, it seems inevitable that the virus will continue to spread, particularly among the unvaccinated for the foreseeable future. If the Delta variant becomes dominant in the US, as it seems poised to do, only the most isolated young people or those surrounded almost entirely by vaccinated people will remain unexposed. Less contagious viral strains infected 33% of Americans in a year. It seems implausible a large percentage of unvaccinated young people will be able to avoid the virus for years to come. As such, I suspect that most everyone will gain immunity to COVID-19 eventually. It’s just a question of whether it’s through the vaccine or virus.
And many young people remain vulnerable. There are about 125 million Americans under the age of 30 years. Subtracting out the 10 million who have been vaccinated and the nearly 50 million who have virus-induced immunity, this means that about 70-80 million Americans under the age of 30 years remain vulnerable. Of course, the Delta variant is unlikely to be the last variant, and it’s not implausible a variant may arise that is significantly more dangerous to young people.
“The vaccines are safe and effective, and they prevent COVID-19 illness”
The CDC calculated:
Among adolescent boys ages 12 to 17 the researchers estimated that, for every one million second dose vaccinations, 5700 covid-19 cases, 215 hospital admissions, 71 intensive care unit admissions, and two deaths would be prevented. Against this there might be an estimated 56 to 69 cases of myocarditis.
Obviously these numbers will change over time as the pandemic evolves. In my opinion, the evidence clearly shows that based on current knowledge, vaccinating people over the age of 12-years is still significantly safer than leaving them vulnerable to the virus.
After the CDC’s presentation on vaccine-induced myocarditis, multiple medical organizations have come out in favor of vaccinating adolescents and young adults. A statement signed by the Department of Health and Human Services (HHS), Centers for Disease Control and Prevention (CDC), American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Obstetricians and Gynecologists (ACOG), American College of Physicians (ACP), American Heart Association, American Hospital Association (AHA), American Medical Association (AMA), American Nurses Association (ANA), American Public Health Association (APHA), Association of Public Health Laboratories, Association of State and Territorial Health Officials (ASTHO), Big Cities Health Coalition, Council of State and Territorial Epidemiologists, Infectious Diseases Society of America, and National Association of County and City Health Officials (NACCHO) said:
The vaccines are safe and effective, and they prevent COVID-19 illness. They will help protect you and your family and keep your community safe. We strongly encourage everyone age 12 and older who are eligible to receive the vaccine under Emergency Use Authorization to get vaccinated, as the benefits of vaccination far outweigh any harm. Especially with the troubling Delta variant increasingly circulating, and more readily impacting younger people, the risks of being unvaccinated are far greater than any rare side effects from the vaccines. If you get COVID-19, you could get severely ill and be hospitalized or even die. Even if your infection is mild, you or your child could face long-term symptoms following COVID-19 infection such as neurological problems or diminished lung function.
The World Health Organization and multiple other countries have similarly decided to vaccinate teens including Belgium, Canada, Spain, Italy, France, Germany, Singapore, The Philippines, Hungary, and Dubai, to name a few. Israel, which first identified the cases of myocarditis and also reported a higher rate than the US (1 in 3,000 to 1 in 6,000 males ages 16 to 24), has also decided to vaccinate people over the age of 12 years. Israel too noted that “95% are considered to be mild cases”. After new outbreaks with the Delta variant, health authorities there recommended that all 12-15-year-olds be vaccinated, after previously saying it was a matter of the parent’s preference. Dr. Galia Barkai, director of the Pediatric Infectious Diseases Unit at Sheba Medical Center, said about this decision,
We were gathering information regarding myocarditis, we were waiting for more children to get vaccinated in other countries such as in the United States. There were days with no COVID-19 cases in Israel. I tend to think that being more conservative was the right decision, and now things have changed.
Some Israelis are now wondering if their government was too slow to vaccinate children ages 12-15 years.
The core of medicine is the balancing of benefit and risk
The core of medicine is balancing risk and benefit. It’s a debatable question at exactly what age the benefits of vaccination exceed the risks, and the answer to this question will evolve as the pandemic evolves. Reasonable people can disagree about the exact age where the vaccine is likely to cause more problems than it prevents. No one is proposing vaccinating newborns and every reasonable person favors vaccinating older adults.
Some have reasonably proposed that the risk/benefit ratio for young people could be improved by giving just one mRNA injection or spacing out the interval between injections. In one study, one dose of the Pfizer mRNA vaccine was 83% effective at reducing hospitalizations with the alpha variant and 94% against the Delta variant, though the confidence intervals were very large (62-93% for the alpha variant and 46-99% for the delta variant) indicating great uncertainty about the true number. Of course, as previously noted, young people can suffer from COVID-19 without being sick enough to be hospitalized. It’s not clear whether these strategies will improve the safety of the vaccine while still reducing the risk of the virus to young people. Unfortunately, the Delta variant will likely move faster than science’s ability to adequately evaluate these approaches, but they deserve serious consideration. Additionally, the CDC’s position that the very small number of people who had myocarditis after the first vaccine dose should still consider getting the second vaccine dose seems very questionable at best.
For some, however, this near unanimity of opinion in medical organizations and governments favoring vaccination in young people is an invitation to distinguish themselves by reflexively opposing this consensus. Those who opposed vaccines in adolescents even before myocarditis cases became apparent are now using this side effect to justify their opposition. Some red flags to look out for are articles that:
- Only describe the risk of COVID-19 to young people as “low” or “rare” without specifying the exact of number of deaths or the number of cases of MIS-C. Astonishingly, I’ve read multiple articles on COVID-19 and children by respected doctors that do not even mention these rare, but catastrophic outcomes.
- Mention that pediatric hospitalizations may have been overcounted, without mentioning that they might have been undercounted.
- Do not mention that at a minimum COVID-19 has hospitalized tens of thousands of children/young adults and that quite plausibly this number is well over 100,000 people.
- Equate hospitalizations due to vaccine-induced myocarditis with hospitalizations due to COVID-19. As stated previously, hospitalizations due to COVID-19 are typically much more severe, with many needing ICU-level care and some needing mechanical ventilation.
- Confidently assert the vaccine-induced myocarditis rate is much higher or more dangerous than we currently know without providing compelling evidence as to why.
- Speculate on the potential long-term effects of vaccine-induced myocarditis while simultaneously minimizing or not acknowledging the potential long-term effects of the virus itself, including viral-induced myocarditis associated with MIS-C.
- Fail to acknowledge that the vast majority of cases of vaccine-induced myocarditis have fully recovered or seem likely to do so.
- Mention that several countries, such as the UK, are not vaccinating adolescents currently, without mentioning that these countries plan to do so in the near future and are outliers in countries with abundant vaccines.
- Confidently assert that relatively untested alternatives, such as a single injection or spacing out injections, have been definitively shown to be safer and as effective as the current two-dose vaccine schedule.
- Confidently speak as if the pandemic is “essentially done” for young people or that they can be protected simply by increasing vaccination in adults, as if this is a trivial task given the previously described vaccine hesitancy.
- Ignore the implications of the highly contagious Delta variant, which unvaccinated people may have to avoid for years to avoid getting infected.
- Don’t acknowledge that vaccine hesitancy/refusal is a significant, likely intractable problem in much of the country, leaving tens of millions of unvaccinated children potentially exposed to the virus.
- Mention limitations with VAERS without noting that other vaccine-safety monitoring databases exist, namely VSD, and that the myocarditis rates are similar between the two.
- Portray vaccination of young people primarily as a means to benefit adults by creating herd immunity. Everyone is clear: young people should be vaccinated to protect themselves. Perhaps one day COVID-19 vaccination will be like polio vaccination, designed to prevent a resurgence of a disease that currently poses no risk to American children. But for now, it’s just a bonus that children might not lose their mom or dad because they’ve been vaccinated.

