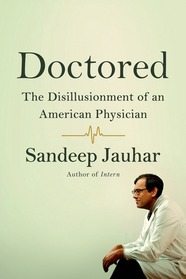
Sandeep Jauhar wrote Doctored: The Disillusionment of an American Physician to express his frustration with the modern system of medical care in America. I found the book profoundly disturbing. If his experience is representative, I can understand why so many people have been criticizing doctors for only caring about money. His experience was so different from mine that I wondered if I had led a sheltered life as a military physician and was oblivious to what was going on in the civilian world. After further reflection, I think Jauhar is unduly pessimistic. Whatever the opposite of rose-colored glasses is, he’s wearing them.
His personal experience of medicine
Dr. Jauhar is a cardiologist who works in a large teaching hospital, where he had been hired to develop a program for patients with heart failure that would implement the most up-to-date medical knowledge and provide the best possible medical care. After long, grueling years of school, residency, and fellowship, he is elated to have finally finished his training and started a job where he can accomplish something good. But he soon sinks into despair. He is appalled by the realities of life as an attending physician, the many ways in which the “system” interferes with his efforts to provide the best care to patients, the unethical behavior of other doctors, and his inability to support his family.
His family, which soon includes two children, is living in a one-bedroom apartment; and even so, he can’t make the rent payments without large cash infusions from his wealthy father-in-law. To supplement his income, he moonlights by working for doctors in private practice; but he is abusively treated by unethical, money-grubbing employers who are gaming the system to make money by doing unwarranted tests and procedures. He envies his brother, an interventional cardiologist in private practice who is making big bucks doing procedures; but he is unwilling and unsuited to engage in the kind of politics that his brother is constantly obliged to use to keep up the flow of referrals (schmoozing with other doctors and fawning on them). By the end of the book, Jauhar has moved to suburbia and his wife has returned to work, so there is finally a prospect of making ends meet.
I just couldn’t relate to this. I have never encountered a doctor who didn’t make a living wage, although I have heard of a few who unwisely tried to live beyond their means. As an Air Force physician I earned considerably less than my colleagues in private practice, but I always had more income than I needed to maintain a comfortable lifestyle. He doesn’t say what his salary is. According to a 2011 survey, the average salary of a hospital-employed cardiologist was $254,000. I find it hard to wrap my mind around the idea that a large teaching hospital would pay a subspecialist so little that he would be unable to pay the rent on a one-bedroom apartment. He seems to be protesting that doctors in general are making too much money while protesting that he doesn’t make enough. Something just doesn’t add up.
Unwarranted pessimism
In a book review in The Wall Street Journal, Dr. Thomas Stossel says:
Dr. Jauhar also invokes what I term “the great American medical guilt trip”: the fact that we spend far more on health care for allegedly worse health outcomes, including higher mortality, compared to other countries. This self-flagellation is an apples-to-oranges comparison of vastly different geographies, social structures and cultures. After subtracting homicides and automobile fatalities, the mortality discrepancies largely disappear.
He also points out that Dr. Jauhar’s view of the past is too rosy. Jauhar compares today’s doctors to a mythical, highly respected, noncommercial medical “knighthood.” Dr. Stossel says he was there and can attest that no such nobility existed. And he points out that in Jauhar’s specialty, death from heart disease is 60% lower today than in the 1950s. He also points out that despite the statistics Jauhar offers on physician discontent, medical school applications rose by 38% between 2003 and 2013. There is a lot wrong with modern medicine, but there is a lot right, too.
The problems he cites are not hopeless
Rather than just complaining, why didn’t Jauhar offer constructive criticism from his privileged point of view as an insider? A lot of the problems that frustrate him are far from insoluble; they have been identified and efforts are already underway to correct them. Here are some of them:
Patients are transferred without records, so doctors don’t have all the information and have to repeat tests that have already been done. (This is a minor glitch that should be trivially easy to fix in this age of information and Internet communications.)
Patients see a number of specialists who don’t communicate with each other. They don’t have a primary doctor who knows them and cares about them as a person. (That’s the reason I specialized in family medicine; it is feasible for a primary care provider to take responsibility for all the patient’s medical care, coordinate referrals, put the specialists’ recommendations into context with the patient’s over-all needs and personal preferences, and translate medicalese for the patient and family.)
Insurance companies overwhelm doctors with paperwork and long telephone battles to get necessary tests and treatments authorized. (This kind of problem is typical of any bureaucracy and there are several conceivable remedies: a single payer national health insurance, competition between insurance companies with survival of the less obstructionist ones, better utilization of ancillary personnel to take the burden off doctors, etc.)
Medical residents are required to go home after a certain number of hours, and continuity of care is lost. (The previous longer hours had the drawback of sleep-deprived doctors endangering patients. The best balance to achieve both training goals and patient welfare goals is still being worked out and impassioned debates are ongoing in medical journals.)
Procedures are reimbursed, but time spent talking to patients is not. (It could be. Reimbursement scales are constantly being revised, and they could be revised to support the goal of doctors spending more time with patients, which both doctors and patients want.)
Terminal patients in hopeless situations are kept alive when it would be kinder to let them go. (It’s often the patient’s family who insists on “doing everything possible.” It would help to have more discussions with healthy patients and their families about advance directives, and time spent on these discussions could be reimbursable.)
A lot of unnecessary tests and treatments are ordered. (The medical profession is self-critical about this issue, and is constantly trying to improve the situation with initiatives like Choosing Wisely, consensus recommendations, policy statements from professional organizations, etc.)
Unethical doctors are gaming the system to make more money in disregard of patient welfare. (We have medical boards that ought to be dealing with such abuses. In practice, they are not doing a very good job. They tend to mostly target cases of drug abuse or sexual misconduct and tend to give substandard care a mere slap on the wrist — just think of the Texas medical board’s ineffective response to Burzynski’s obvious misconduct — but surely there are things we could do to make boards more effective. Isn’t it the responsibility of every doctor to notice when other doctors are using substandard and unethical practices, to confront them directly, to report them, to speak out, to stop referring patients to them? Peer pressure might accomplish a lot.)
Conclusion
The book is an affecting, well-written human-interest story of one man’s experience, but the picture it paints is darker than it needs to be. He admits he suffers from depression and has been getting counseling; I suspect his depression has clouded his perceptions. Some of what he describes represents a typical human trajectory in any lifetime and any job. We grow up. The ideals of youth run into the obstacles of adult reality. We have to earn a living now as best we can, and we don’t have the option of holding out for some ideal job that may not even exist. Aspirations of the perfect succumb to compromises with the possible. “I would never do that!” is replaced by “I had to do it!” Campaign promises are shipwrecked on the political realities of office. Black and white becomes gray and nuanced. A father’s absolute intolerance of abortion changes to reluctant approval of at least one case when his own teenage daughter is raped. We learn that the world doesn’t work the way we wish it would. We adapt. We learn to live with the things we can’t change while we try to change the things we can.
Whatever its faults — and I don’t deny that it has a great many — the medicine of today is better than the medicine of the past and far better than any alternative. Best of all, we are not sitting on our laurels: medicine is self-critical and constantly working towards even better medicine. We could adopt Jauhar’s pessimism and wring our hands in despair or we could be cautiously optimistic and get to work. He has identified a number of problems. That’s only the first step. Now it’s up to all of us to take the next step and look for solutions.