Ed. Note: Harriet Hall was injured in a fall in Australia earlier this month. While she recovers, we are running guest posts in her regular Tuesday slot for as long as our supply of guest posts lasts. (Hint: If you ever thought of submitting a guest post and want a shot at your guest post being published on a Tuesday, now’s the time.) We wish Harriet well and hope she recovers sufficiently to resume blogging soon.
The definition of “functional food,” (also called a “nutraceutical”) is “a food containing health-giving additives and having medicinal benefit.”
But aside from providing calories and maybe some added fiber or protein, there are very few nutraceuticals that have been proven to do anything. Ok, maybe there’s that yogurt that helps Jamie Lee Curtis poop (still not proven). Vitamins are good if you’ve got a bona fide deficiency, but aside from that, you’re better off just eating healthy foods, some foods you enjoy (hopefully those categories overlap a bit), and ignoring the hype.
In fact, nutraceuticals aren’t allowed to say they do anything besides vague structure-function claims. Things like: “Supports Strong Bones,” or “May Help Boost Your Immune System,” or “My Sister Swears By This Thing,” and so on. They sound good, and can be convincing to the uninformed consumer, but are essentially meaningless.
So, while attending the Academy of Nutrition and Dietetics’ annual Food & Nutrition Conference & Expo (better known as FNCE, or #FNCE), I was surprised to see a food product in the expo hall making a claim to this effect: “Benecol can reduce your cholesterol in two weeks.”
This is a very specific claim.
Benecol is sold in numerous forms, but can be found in grocery stores as a brand of margarine. It represents a specific group of functional foods known as plant sterols and stanols, which are unique in the supplement world because they actually do what they say they do.
In trials, when added to the diet, two grams of plant sterols or stanols per day lower LDL cholesterol an average of 8-10%. There are some caveats to this:
- Stanols/sterols seem to work best as part of a food with fat.
- Better results have been seen when intake is spread throughout the day rather than all at once.
So why, you might wonder, aren’t they in more common use? This is what I pointedly asked the Benecol representative at the Expo hall. She shook her head, wide-eyed. It seemed to be a mystery, even to the Benecol people.
But I think I’ve figured it out.
First: Do plant sterols & stanols lower cholesterol? How?
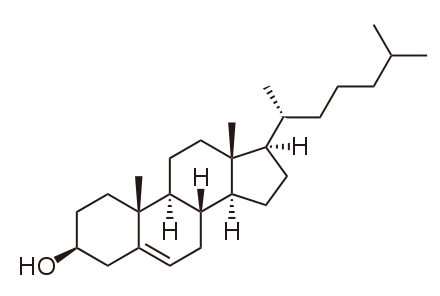
As it turns out, it is well established that plant sterols (and stanols – plant sterols that are saturated at the 5 α- ring position) interfere with the absorption of cholesterol in the small intestine, effectively lowering plasma cholesterol. And there seems to be a proportional response: In those with higher LDL cholesterol, plant sterols have a stronger effect.
Plant sterol β-sitosterol (the double bond in the ring structure = unsaturated)
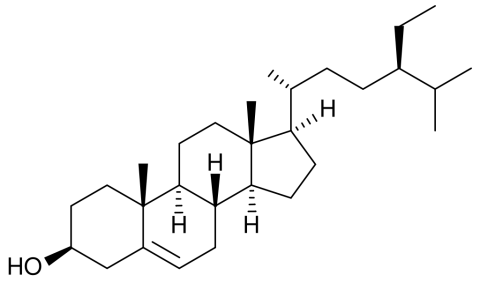
Plant stanol β-sitostanol (no double bond = saturated)
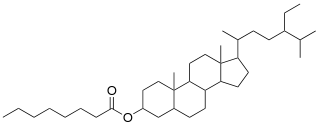
On the left side of the diagram you can see that the alcohol group (-OH) has been replaced by an ester (O-C=O). This is how plant stanols (and sterols) are incorporated into Benecol.
These molecules resemble cholesterol, but all the extra carbons at the end (all the branches in the diagram) make the sterols and stanols much more difficult for the body to absorb.
Are they beneficial?
While scientists have understood the effects of plant sterols since the 1950s, it is less clear whether they would have an impact on clinical endpoints (ie development of cardiometabolic disease). This is because the resources it would take to do a definitive RCT on the effects of the sterols are prohibitive. In a review in Mayo Clinic Proceedings, Katan, et. al noted that:
… with a 6% reduction in total cholesterol (corresponding to a 9% reduction in LDl cholesterol), close to 50,000 postmenopausal women might need to be randomized and followed up for 9 years to show the expected reduction of 14% in CHD at a power of 86%.
However, many experts agree that the use of sterols is indicated based on the beneficial effects of sterols on surrogate markers, i.e. LDL cholesterol. Dr. Alice Lichtenstein, Director of the Cardiovascular Nutrition Laboratory at the Jean Mayer Human Nutrition Center on Aging, had this to say:
My assessment of the evidence is that if a food/drug/lifestyle behavior lowers LDL cholesterol there will likely be a benefit on health outcomes. Sterols and stanols clearly lower LDL cholesterol, hence, one would predict a benefit.
This is in line with a review by AbuMueis and Jones in Current Atherosclerosis Reports:
It is estimated that a 10% reduction in serum cholesterol level produces a reduction in CHD of 50% at age 40 years, 40% at age 50 years, 30% at age 60 years, and 20% at age 70 years. Therefore, the degree of placebo-adjusted reduction in LDL-C levels caused by plant sterols is of clinical importance.
And a more recent consensus document, published in Atherosclerosis in 2014, the European Atherosclerosis Society Consensus Panel on Phytosterols came to the following conclusions:
Based on LDL-C lowering and the absence of adverse signals, this EAS Consensus Panel concludes that functional foods with plant sterols/stanols may be considered
- in individuals with high cholesterol levels at intermediate or low global cardiovascular risk who do not qualify for pharmacotherapy,
- as an adjunct to pharmacologic therapy in high and very high risk patients who fail to achieve LDL-C targets on statins or are statin- intolerant,
- and in adults and children (>6 years) with familial hypercholesterolemia, in line with current guidance.
But in an unscientific survey conducted by moi (aka I asked one person who is on a statin), I learned that this person had never heard of plant sterols, let alone considered adding them to his diet. Add that to the “who knows” mystery face of the Benecol rep at the FNCE expo floor and I have an anecdata set of two people suggesting that the benefits of plant sterols are not widely used or widely known in the US.
Why would this be?
The downsides
There has been concern that higher plasma levels of plant sterols and stanols would increase cardiovascular disease risk and offset the benefits obtained from lower cholesterol. There seems to be a consensus among experts that this is largely a hypothetical risk and that even among patients heterozygous for phytosterolemia (a genetic disease where a person absorbs an unusually high percentage of plant sterols and develops atherosclerosis at an early age), plasma levels of plant sterols remain orders of magnitude lower than those homozygous for phytosterolemia even when supplementing.
There has been some concern that high sterol intake could inhibit absorption of fat-soluble vitamins – but this remains largely theoretical as well.
So why aren’t health professionals – doctors and RDs alike – more inclined to recommend plant sterol intake?
Here are my ideas:
- Plant sterols cannot replace a statin for cholesterol lowering – Phytosterols work to lower cholesterol levels up to about 10% but then plateau.For someone with hypercholesterolemia this would not cut it as a stand-alone intervention. And if a statin returns cholesterol levels to normal, it may not be necessary to recommend a plant sterol product in addition.However, they do have an additive effect when used with statins, and do not lose their effectiveness – in some patients adding plant sterols to statin therapy can have the same effect as doubling the statin dose.But, there have not been a lot of studies done on plant sterols in combination with ezetimibe, a drug that lowers plasma cholesterol by preventing absorption, similar to the action of plant sterols and stanols.
- Convenience: According to the bulk of the literature on plant sterols, the dose is most effective in a food form (fat spreads like margarine are the most studied) taken at least twice per day. If someone is eating a margarine, they need to remember to eat enough of the margarine and eat it twice per day – it sounds simple, but it would be all too easy to forget.
- Cost: Food and supplements are not reimbursed by insurance companies, so while the cost of a statin may be mostly covered by a patient’s insurance, the cost of a Benecol margarine is fully on the consumer.
- A major PR problem: Arguably, the most effective way to lower one’s cholesterol with plant sterols is by eating margarine – probably one of the most hated “fake” food products of our time.Since even the diets highest in plant sterols only hit several hundred milligrams, it is impossible to get therapeutic doses through vegetables alone. The only way to get them is in “processed food,” another term that gets a lot of unfair hate these days.
I ate it
So I did what any self-respecting nutritionist would do, I ate some. As far as taste, there is nothing to report – it tastes like a soft, buttery spread and doesn’t have a weird aftertaste. Since I am usually a butter eater, the soft texture of the stuff right out of the fridge threw me off, but once it was on my English muffin, it tasted totally normal.
But after my snack, I noticed some features that would make Benecol (or any plant sterol/stanol margarine) a less practical intervention.
In a single serving of one tablespoon, there is only half a gram of plant stanols. In order to get a full dose of two grams of plant stanols a day, I would need to eat four tablespoons of margarine. That seems like a lot, since I would need to find ways to incorporate it into every meal, or eat a double dose at lunch and dinner.
And there are 16 servings of Benecol in one container, which means that I would run out of margarine every four days. Benecol is not cheap – running between $5-6 a tub. That’s something like $40 a month on margarine – pricier than my gym membership, another intervention with beneficial effects on cholesterol (exercise, not a gym membership). Since plant sterols/stanols work by preventing cholesterol absorption when you eat them, continuous use is required to maintain cholesterol-lowering effects.
Finally, the nutrition facts panel notes that each serving of Benecol contains half a gram of trans fats, meaning that with my two grams of plant stanols, I’m also getting two grams of trans fats, a food additive we have long considered “no bueno.” Trans fats are believed to increase heart disease by raising LDL cholesterol, so it is unclear whether the net cholesterol-lowering effect of a plant stanol/sterol nutraceutical would cancel out the risk. But really, why include them? I reached out to Benecol customer service asking why they haven’t reformulated or if they were considering it, but have not heard back.
Interestingly, trans fats may have been mislabeled on earlier containers of Benecol leading to a class action suit, which was settled out of court. I reached out to Benecol to inquire about trans fat content and have not yet heard back.
The verdict?
Clinicians should feel free to recommend plant stanol/sterol products to supplement healthy lifestyle changes in preventing heart disease – there are little indications for negative effects. Consider whether you think it would be practical: If you have a patient or client with a ton of money who eats bread with butter 3+ times a day, you have an ideal candidate.
Other well-studied plant sterol-enhanced foods are yogurts and other dairy products. Overall, the efficacy of plant sterols incorporated into “fat spreads, mayonnaise and salad dressing or milk and yoghurt” reduces LDL more than sterols in other products. It should be noted that plant stanols/sterols can be taken in capsule form and also have cholesterol lowering effects. However, they still must be taken two or three times per day with meals.
Which brings us to the real problem with plant stanols; it requires daily adherence, a change in dietary habits, and consistency.
In other words, it requires the most effective and elusive of interventions: a lifestyle change.