Longtime readers of Science-Based Medicine and my not-so-secret other blog probably know that I’m not a fan of the specialty known as “integrative oncology.” My reasons are basically the same as the reasons why I detest “integrative medicine,” only subspecialized (like oncology), so to speak. Basically, “integrative medicine” integrates quackery with medicine, and integrative oncology integrates quackery into oncology. Given that I’m a cancer surgeon, I tend to take an even dimmer view of the latter than of the former, if only because it hits me where I live. For instance, when “integrative oncology” starts appearing at symposia at major cancer meetings, with nary a skeptical word showing up in the panel discussions afterwards, I despair. Unfortunately, the credulity that allows modalities like acupuncture, reiki, intravenous high dose vitamin C, and various other unproven and disproven treatments to find their way into academic medical centers has spawned a related phenomenon, quackademic medicine, or the study and acceptance of quackery in academic medical centers. The most prominent example of this latter phenomenon occurred in September, when the University of California at Irvine accepted a $200 million gift from Susan and Henry Samueli to build and staff a college devoted to integrating quackery into its component departments and promoting “integrative medicine.” Never mind the homeopathy.
Integrative oncology has become so established that it has its own professional society, the Society for Integrative Oncology (SIO). Not surprisingly, I’m not a fan of SIO, and SIO isn’t exactly a fan of me, either. I’ve related the story before, but let’s just say that the SIO was not pleased at my 2014 article in Nature Reviews Cancer discussing how integrative oncology is not evidence-based (to say the least), given its embrace of naturopathy. In brief, the SIO didn’t like how much verbiage I devoted to homeopathy in the article, pointing out that homeopathy is indeed not evidence-based and that no integrative oncologist worth his or her salt would ever use it. I pointed out that you can’t have naturopathy without homeopathy. After that, I asked how the SIO can reconcile its quite correct rejection of homeopathy with the fact that it admits naturopaths as members, that two of its recent past presidents have even been naturopaths, and that you can’t have naturopathy without homeopathy. It’s baked into the naturopathic curriculum, and it’s part of the naturopathic licensing exam. Moreover, one of the naturopaths who co-authored the SIO’s breast cancer clinical guidelines ran a clinical trial on homeopathy. That same naturopath, by the way, was a co-author on the update to those guidelines published just this year. The SIO never learns.
This time around, though, the reason the SIO caught my attention was this Tweet by Dr. Sheila Garland, re-Tweeted by Dr. Jun J. Mao, immediate past president of the SIO (but still president at the time he re-Tweeted this):
The beginning of a new era in evidence-informed integrative oncology research/practice that puts the person first #SIO2017 @Integrativeonc https://t.co/cmAMrCujjy
— Dr. Sheila Garland (@SNGarlandPhD) November 13, 2017
This Tweet touted what is now the “official” definition” of “integrative oncology” recently laid down by the SIO:
Official definition of Integrative Oncology! Spread the word! #SIO2017 We are research based! #cancerresearch pic.twitter.com/oeNsn9B1Jk
— Jodi MacLeod (@write4wellness) November 13, 2017
It turns out that this definition had just been published by Witt et al in the November issue of JNCI Monographs, just in time for the SIO annual meeting last week. When I saw it, my first reaction was to e-mail my fellow SBM bloggers with a link and this image:
So let’s take a look.
The process of defining “integrative oncology”
My first reaction (besides possessiveness) when I saw the article by Witt et al, A Comprehensive Definition for Integrative Oncology was: What? The organization has existed for nearly 15 years, and in all that time it hasn’t yet managed to define what it’s about until now? My second reaction was: What on earth does this definition actually mean? It is about as boring, generic, and—shall we say?—vague a definition of anything as I’ve ever seen. Take a look:
Integrative oncology is a patient-centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments. Integrative oncology aims to optimize health, quality of life, and clinical outcomes across the cancer care continuum and to empower people to prevent cancer and become active participants before, during, and beyond cancer treatment.
In actuality, I was more interested in what was left out of this definition than what was in it, but I’ll get to that near the end of this post. First, I want to look at the process by which the authors developed this definition, as described in the article, which is open-access for those of you who want to read it yourselves. Before I get into the process, let’s look at some of the authors, who are big names in the world of integrative oncology. The lead author, Dr. Claudia Witt, is Professor and Chair of the Institute for Complementary and Integrative Medicine at the University of Zurich and University Hospital Zurich, as well as part-time Professor of Primary Care and Community Medicine at the Center for Integrative Medicine University of Maryland School of Medicine. Dr. Jun J. Mao is, of course, president of the SIO and Chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center. Dr. Lorenzo Cohen is someone whom we’ve met before, when he gave a talk at the American Society of Clinical Oncology (ASCO) meeting in 2014. He’s the Director of the Integrative Medicine Program at The University of Texas MD Anderson Cancer Center. Linda Balneaves is a nurse and the current president of SIO, having succeeded Dr. Mao at the SIO annual meeting last week. I also can’t help but note that one of the co-authors, Heather Greenlee, is a naturopath and has served as president of the SIO in the past as well.
In other words, these are indeed heavy hitters and the leadership of the SIO.
Let’s look at their justification for seeking this definition. After regurgitating the usual “complementary and alternative medicine” (CAM) blather about how patients are just “looking for “additional interventions that may help improve the efficacy of conventional cancer treatments, increase their chance of survival, and/or reduce their symptom burden associated with cancer or treatments” and “improve their quality of life during and following treatment,” Witt et al justify their search for a definition thusly:
With the integration of interventions such as acupuncture, mindfulness and yoga, and lifestyle counseling into major cancer centers in North America (eg, MD Anderson and Memorial Sloan Kettering Cancer Center), the term “integrative oncology” has become increasingly used. “Integrative” better represents the process of care that is provided in centers where patients are receiving these types of interventions in addition to their conventional cancer treatments. With the establishment in 2003 of the Society of Integrative Oncology (SIO), a nonprofit multidisciplinary professional organization, the term “integrative oncology” was further legitimized and began to be widely used. However, the term “integrative” is also used in other contexts. An example is the Berlin School of Integrative Oncology at the Charité Medical School in Berlin (2), which is an initiative of the German federal and state governments that aims to educate young scientists and physicians in oncology in an interdisciplinary, translational research context. Although the term “integrative oncology” is rarely used in such an educational context, having totally different meanings for the same term can generate confusion. Adding to this complexity is the growing attention to the notion of integrated care programs in oncology, in which numerous cancer specialties (eg, medical oncology, radiation oncology, surgical oncology, genetics, plastic surgery) work together to provide comprehensive patient care (3).
Furthermore, even in settings in which the term integrative oncology has been used to refer to the combination of complementary medicine therapies with conventional cancer treatments (4), the term has been defined in many different ways (5,6). Because of this lack of consensus, it has been difficult to communicate what is meant by “integrative oncology” to oncologists and other health professionals, as well as to key stakeholders, such as patients, administrators, and health policy makers. The aim of this project was to use a systematic approach to develop a comprehensive and acceptable definition for “integrative oncology.”
Actually, I’ve always rather suspected that this confusion is a feature, not a bug, related to the use of the word “integrative.” After all, integrative oncology, like integrative medicine, is a brand, not a specialty. It rebrands what should be considered perfectly fine science-based modalities, such as nutrition, lifestyle interventions, and the like, as somehow “alternative” or “integrative,” and then “integrates” quackery like acupuncture, reiki, functional medicine, and even homeopathy with them, to give the quackery the appearance of scientific legitimacy. No, I don’t think SIO is doing this intentionally; its leadership consists of true believers. But it is contributing to quackademic medicine and the integration of quackery into oncology. In any event, the word “integrative” is, as mentioned above, used to describe science-based endeavors, such as integrative biology. In this context, the word “integrative” connotes interdisciplinary study, a very different meaning than when the word “integrative” came to replace the term CAM to describe adding pseudoscience to medicine.
Indeed, use of the word “integrative” to describe medicine or the subspecialty of oncology connotes more than interdisciplinary patient care and research. It connotes the embrace of “alternative” treatment modalities as well. The term “CAM” still had the word “alternative” in it and the word “complementary” connoted that CAM was subsidiary to medicine, “complementary,” the icing on the cake, if you will. In other words, it’s not necessary, and science-based medicine is the real medicine. The adoption of the word “integrative” to rename CAM as “integrative medicine” was clearly intended to remove the implication that CAM was “complementary” and not as good as real medicine, in order to advance the narrative that integrative medicine is the “best of both worlds,” while also borrowing from the cachet of various “integrative” scientific disciplines as being multidisciplinary. Again, I don’t think SIO is out to deceive. Rather, the belief of the SIO leadership in the validity of integrative oncology has led them down this road, probably without even realizing it.
So how did Witt et al go about constructing their definition? Enter the mixed methods research design and Delphi method. This amused me, because it wasn’t so long ago that naturopathic oncologists used this very method to try to define priorities in naturopathic oncology. If you want the details of how the Delphi method works I discussed them in deconstructing the nonsense that naturopaths laid down about their quack specialty using the Delphi method. The CliffsNotes version is that the Delphi method entails a using a group of experts to answer a question. The experts anonymously reply to questionnaires and subsequently receive feedback in the form of the statistical representation of the group response, after which the process repeats itself until something resembling a consensus is arrived at. The way Witt et al did this is described:
A two-round Delphi process was then employed to further refine and gain consensus regarding the new definition. In the first round, the revised definition was distributed via an online survey (software SoSciSurvey [7]) to SIO board members as well as to a convenience sample of experts. The experts—oncologists, integrative oncology clinicians, and/or researchers from North America, Europe, and Asia—were contacted by the SIO board members. Based on first round feedback, the definition was revised and distributed again through an online survey to the full membership of SIO, with subsequent ratings and comments used to inform the final version of the definition. Data from both surveys were analyzed using descriptive statistics. Content analysis (8) was applied to the open-ended responses to identify any themes or concepts.
So, after this literature search and Delphi method, what did Witt et al find?
Defining “integrative oncology”
As a result of their literature search and two-round Delphi process, Witt et al found many definitions of “integrative medicine” and “integrative oncology” in the literature, which resulted in the following thematic suggestions:
- evidence-based/evidence-informed/evidence-guided/using best available evidence (14 of 20);
- accompanying conventional cancer treatment (18 of 20);
- addressing outcomes such as well-being, body, and mind-spirit, as well as physical, psychological, and spiritual quality of life (seven of 20);
- focused on health and not only on medicine (three of 20);
- provided by a team of health care providers/multidisciplinary/interdisciplinary (four of 20);
- patient-centered/personalized, individualized/whole person (two of 20).
The writing group, which consisted of “members with different professional/disciplinary backgrounds (ie, medical oncology, radiation oncology, surgical oncology, nursing, patient advocacy, psychology, psycho-oncology, epidemiology, integrative medicine, health policy),” added these additional suggestions:
- type of interventions (mind-body therapies, natural products, lifestyle changes);
- beyond provision of health care (information, translation of evidence, identification of beliefs, values and preferences, empowerment).
The initial definition of integrative oncology developed by the group thus read:
Integrative oncology is a patient-centered (theme 6), evidence-informed (theme 1) approach to health care (theme 4) that uses mind-body therapies, natural products, and lifestyle modification (theme 7) as adjunct to conventional cancer treatments (theme 2) and is ideally provided by a multidisciplinary team of care providers (theme 5). Integrative oncology aims to increase well-being of mind, body, and spirit (theme 3) and to provide patients with skills enabling them to help themselves during and beyond cancer treatment (theme 8).
After the two rounds of Delphi method, though, the group perceived that some changes were required:
Overall, the comments on the second Delphi survey were positive, but the suggestions were quite heterogeneous. Two-thirds of suggestions focused on what were perceived to be missing interventions, and it became clear that therapies such as acupuncture and massage were not well represented in the definition. As a consequence, the definition was revised using the umbrella term “mind and body practices,” which is used by the National Center for Complementary and Integrative Health in the United States. This term includes mind-based techniques such as meditation and hypnosis, as well as manual techniques such as acupuncture and massage (9). One respondent mentioned that “health care” encompassed a broader area than integrative oncology, and the decision was made to be more focused and to use the term “cancer care” in the revised version. Another respondent also suggested that the phrase “approach to cancer care” could be misleading and not specific enough as a field of care or medical specialty. Integrative oncology is more than just an approach to overall cancer care; it has been the focus of a professional organization for more than 10 years and is an established field in its own right. During the review process, it was noted that cancer prevention was not included in the definition. Because the ultimate goal of many integrative oncology behaviors is cancer prevention and control, the definition was modified to include prevention.
I’ve discussed before how quackery like the theatrical placebo known as acupuncture has mysteriously been subsumed into “mind and body practices”. Personally, I’ve always suspected that this was to hide the quackery of acupuncture with more benign modalities (such as massage) that, whether medically they can treat anything, generally do no harm, and can certainly feel good, thus improving quality of life. After all, given that the rationale in traditional Chinese medicine for acupuncture is that sticking the needles into specific “meridians” can redirect the flow of qi (life energy) for healing effect, acupuncture could easily be classified as a form of energy healing.
To the degree that integrative oncology sticks with science- and evidence-based tests and treatments, my main objection to it is that it’s not necessary. Nutrition, exercise, and other lifestyle-based interventions are already a part of science-based medicine. I like to cite, for instance, evidence-based recommendations for the treatment of hypertension and type II diabetes, both of which emphasize, except for severe cases, dietary modifications, exercise, and weight loss as the first interventions to attempt before placing the patient on medications.
To paraphrase Harriet Hall, what is good about integrative oncology (or medicine) is not unique to it. Continuing the paraphrase, unfortunately, what is unique to integrative oncology is not good, and the SIO definition obscures or neglects to mention these unique (and not good) aspects.
What the SIO left out
If you read the full article, it should become very apparent that its authors want desperately to convince the reader that integrative oncology is completely evidence-based. Sure, the SIO admits naturopaths and even elects them as the organization’s president from time to time, never mind that all naturopaths are trained in The One Quackery To Rule Them All, homeopathy, and that the vast majority of naturopaths routinely prescribe homeopathic remedies, which, even the SIO concedes, are rooted in pseudoscience.
I was reminded of this on—where else?—Twitter. I came across a post on the University of Pennsylvania’s OncoLink touting reiki in cancer care. Because the link was from 2011, I Tweeted a question to the OncoLink team. Here’s the response:
@gorskon, Reiki is a supportive therapy that can be used in conjunction with treatment. It is not promoted as an alternative to treatment
— OncoLink Team (@OncoLinkTeam) November 2, 2017
If there is a challenger to homeopathy’s title of The One Quackery To Rule Them All, reiki would be right up there. It is, as I have described many times before, a form of faith healing that substitutes Eastern religious beliefs for the Christian religious beliefs that usually undergird faith healing in the US.
But it’s not just Penn. The Dana Farber Cancer Institute has also gone all in for nonsense:
7 Ways Integrative Therapies Help Cancer Patients: https://t.co/bRHYbqhrcy pic.twitter.com/0kVQ4FKW0o
— Dana-Farber (@DanaFarber) August 26, 2017
The slideshow at the link above promotes reiki, reflexology, and acupuncture:
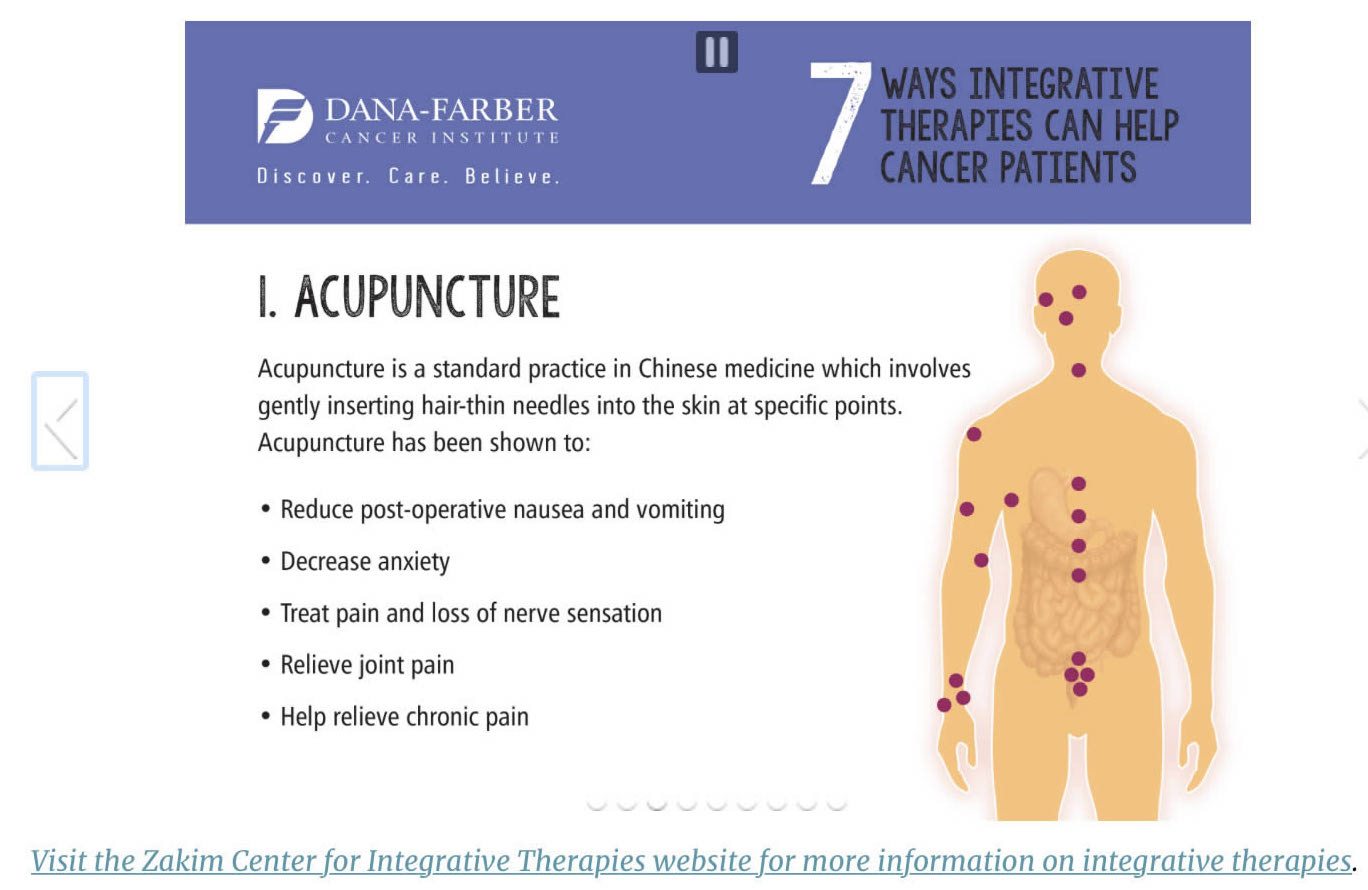
Acupuncture is nothing more than a theatrical placebo, whose action has never been convincingly shown to be greater than that of placebo controls. Yet Dana Farber Cancer Center thinks acupuncture is science-based.
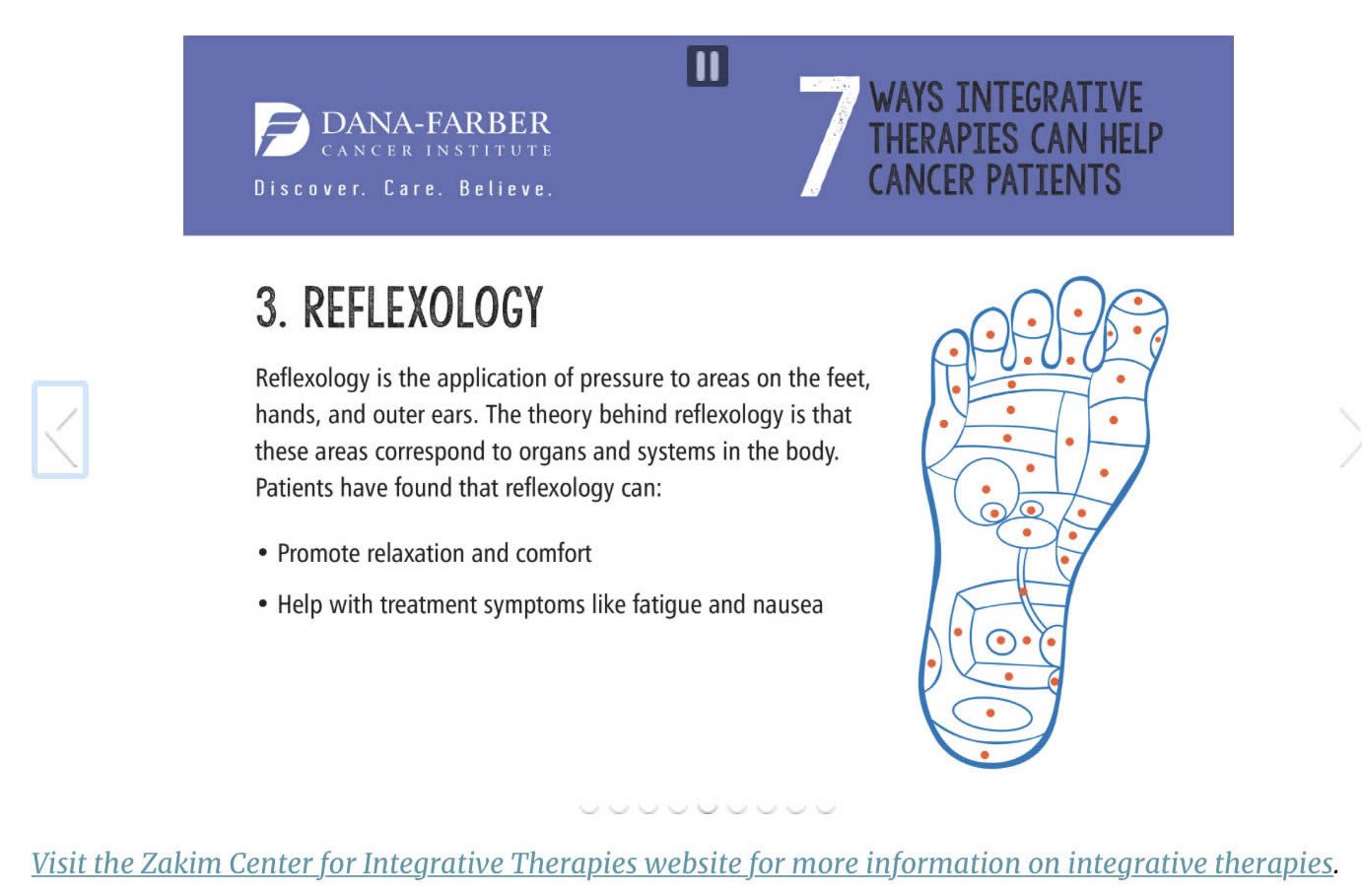
Reflexology posits the existence of physiologic or anatomic links between organs and body parts and areas on the soles of the feet and palms of the hand. Yet Dana Farber Cancer Center thinks this is science-based.
Reiki masters claim to be able to heal by channeling energy into the patient from the “universal source.” Replace “universal source” with “God” or “Jesus,” and it becomes obvious that reiki is a form of faith healing that replaces Christian beliefs with Eastern mysticisms. Yet Dana Farber Cancer Center thinks it’s science-based.
Of course, I’ve pointed out how oblivious the SIO is to the modalities that are really being “integrated” into oncology through integrative oncology just through the obliviousness of the SIO leadership to what naturopathy really is. As I’ve said before, if the SIO were really serious about being evidence-based, it would immediately purge itself of all naturopaths. It’s not, though. Its leadership up in the ivory towers of medical academia can delude themselves into thinking integrative oncology is totally evidence based, because they manage to ignore the quackery that is “integrated” along with the lifestyle-, exercise-, nutrition-, and meditation-based modalities to which they love to point.
I can’t help but point out a few more examples of the quackery that goes along with integrative oncology. At UC-Irvine and the Cleveland Clinic, there’s homeopathy. At the University of Arizona Cancer Center, there was reiki, at least until a faculty member whose child developed cancer and was treated there made a stink. There’s also more energy medicine quackery, this time in the chemotherapy suite, at Georgetown University, as well as cupping, which is also pure quackery. There’s functional medicine at the Cleveland Clinic, George Washington University, University of Kansas, and, well, seemingly almost everywhere at any medical center with an integrative medicine program. If you want an idea of how bad functional medicine is, just check out this case report of functional medicine used for a patient with inflammatory breast cancer. This is what integrative oncology really involves.
It is also this quackery that the SIO definition of “integrative oncology” does its best to obscure or ignore. If the SIO is truly serious about being science- and evidence-based, it needs to speak out strongly and now against naturopathy and the various forms of quackery that have found their way into academic medical centers, of which, I assure you, the above is but a small sampling. It won’t, though. The quackery is why integrative medicine and oncology exist in the first place. Without the quackery, CAM (or integrative medicine or oncology) becomes completely unnecessary as a field.

