If you’ve ever experienced the pain of a charley horse, then you’ll have an idea of what about half of all adults over the age of 60 experience – nocturnal leg cramps. A nocturnal leg cramp can occur in the leg or foot, and is a painful and sudden tightening of a muscle that can last from seconds to minutes, and can recur in the night. Not surprisingly, nocturnal leg cramps can interrupt and impair sleep and while these cramps don’t cause permanent injury, they can lead to decreased quality of life from the pain and sleep impairment. Despite the frequency with which these leg cramps occur, very little is known about what causes them and what anyone can do to prevent them. Consequently, there are an enormous number of medicinal, folk, and alternative remedies that are used and endorsed by both health professionals and patients alike. And a recent survey has shown that most people are treating leg cramps with remedies that are useless, dangerous, or useless and dangerous. What’s the best approach when there’s no decent evidence?
The causes of nocturnal leg cramps are not well understood. The cramp itself is due to the repetitive firing of motor units in the muscle but what triggers the contraction is not known. While often attributed to electrolyte imbalances or dehydration, there seems to be no relationship between the two. Many drugs are associated with reports of leg cramps (even drugs used to prevent leg cramps), but there’s very little evidence to show that any actually cause them.
Unless an underlying medical cause has been identified for nocturnal leg cramps, the approach to idiopathic cases focuses on reducing their frequency and severity. The acute management of a leg cramp is the most immediate concern, and usually stretching the muscle is enough to stop the cramp. Stretching to prevent leg cramps is the most commonly recommended non-drug approach, and while stretching has been studied in clinical trials, the evidence is mixed, with controlled trials (sham stretching) reducing the observed effectiveness of this approach.
Perhaps not surprisingly there are an enormous array of supplements and remedies used to prevent leg cramps. A recent survey of treatments used by 632 older adults with leg cramps in medical practices in Alsace, France illustrates the variety of approaches in use. This was a questionnaire-based study that evaluated if patients had nocturnal leg cramps, if they used any therapies, and what those therapies were. Of the 632 patients, 133 (20%) were using drug- or non-drug treatments to treat about 3 episodes of cramps per month. I’m not going to review the statistical analysis in any detail as I think the breadth of what is studied is what is interesting, rather than their absolute ranking. Here’s the list of treatments used:
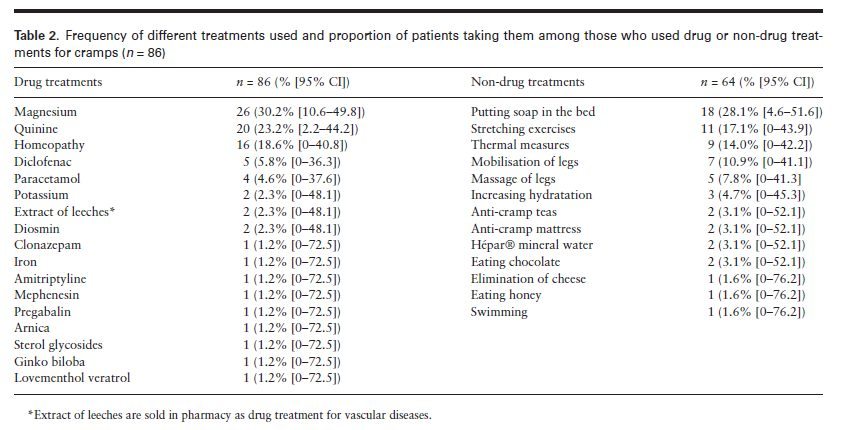
It’s quite the list. Magnesium is number one, despite evidence that it is no better than placebo.
Quinine is number two, which perhaps reflects cultural differences, as quinine use for leg cramps has dropped elsewhere as a result of FDA action against its use. Quinine seems to have some effectiveness against leg cramps, although the evidence is of mixed quality. But what is well known is that quinine can cause fatal allergic reactions as well as a host of other toxicities, even after a single dose. After the FDA issued a warning about quinine and implemented new prescribing requirements in 2010, usage dropped 99% in the USA.
Again, perhaps representing cultural and geographic trends, homeopathy was reported as number three. Not much can be said about the elaborate placebo that is homeopathy, but perhaps the best that can be said is that it doesn’t have the potential to kill you, unlike quinine. (Amazingly, a homeopathic leg cramp “remedy” has been endorsed as the official cramp relief sponsor of the Boston Marathon.) The rest of the treatments identified by patients in this sample range from anti-inflammatory drugs to antidepressants and even to extract of leeches, a French remedy that has yet to receive FDA approval.
Among the non-drug treatments, what appears to be a folk remedy (soap in the bed) is #1, followed by an array of approaches that seems to be endorsed or accepted by most of the treatment guidelines that exist: stretching, mobilization, heat and massage all tend to be recommended, usually with the caveat that there is little good evidence to show that they are effective.
Choosing wisely when there’s no good evidence
While nocturnal leg cramps affect millions, there’s little good information available to guide patients or health professionals in choosing treatments. The wide number of approaches that are used reflects the reality that nothing really works effectively, so any benefits perceived are more likely to be random variations in their occurrence rather than actual cause and effect. The absence of evidence is frustrating, given how common and debilitating nocturnal leg cramps can be. This doesn’t appear to be a big area of research, so we are likely to be in this situation for the foreseeable future.
When faced with a lack of good evidence for any treatment, we should then focus our attention on safety. Non-drug measures like massage and stretching would seem to have the lowest risk, even lower than supplements like magnesium or vitamins. Given the poor quality control pervasive in the manufacturing of herbal remedies, and given the lack of evidence they work, they would appear to also present an unfavorable risk-benefit ratio. Only when non-drug treatments have been tried, and only when leg cramps are truly disruptive to quality of life, would it seem that drugs (or supplements) would be worth test. Until better evidence emerges, it seems many of us will continue to struggle with preventing and treating nocturnal leg cramps.
