![Lieu et al. (2015). "Geographic Clusters in Underimmunization and Vaccine Refusal". [PDF] Pediatrics, 135 (2)](https://sciencebasedmedicine.org/wp-content/uploads/2015/01/hot-zones.jpg)
Lieu et al. (2015). “Geographic Clusters in Underimmunization and Vaccine Refusal”. [PDF] Pediatrics, 135 (2)
It never ceases to amaze me how few of the parents I know think about the risk to their own children from vaccine-exempt children in their schools and communities. Even parents who do think about this rarely seem concerned enough to speak up or even discuss it with others, let alone become active in doing something about it. With the rise in vaccine-preventable disease outbreaks, including the current high-profile Disneyland measles outbreak, and the ongoing pertussis epidemic in California, the tide seems at least to be turning slightly. The dramatic impact that vaccine refusal and the resultant decline in herd-immunity can have on a community is now penetrating the public consciousness. My hope is that parental awareness and outrage grow regarding the flagrant disregard of science, common sense, and citizenship exhibited by those parents who refuse to properly vaccinate their children. My hope is that the culture of tolerance of this intolerable anti-science threat begins to turn, and that it is no longer seen as acceptable for some parents to put the safety of others at risk.
Which brings me to the focus of this post.
My wife and I recently went through the process of deciding where to send our daughter to school. We weighed the pros and cons of several schools, taking into consideration curricular philosophies, student-teacher ratios and facilities, among other things. What we didn’t compare between these schools – and couldn’t in the Commonwealth of Massachusetts – was the number of her classmates that have been appropriately vaccinated, and how many parents would be avoiding the vaccine requirements by claiming so-called “religious” exemptions. We didn’t consider or even have access to the information that would tell us the strength of the schools’ protective shield of community immunity, and therefore how protected our daughter would be from contracting dangerous, vaccine-preventable diseases. In Massachusetts, as in most states, information about school vaccination and vaccine exemption rates was not publicly available at the time. Fortunately, Massachusetts has just changed course, and is now publishing these data, though with some very significant exceptions which I will discuss below.
Probably more than any other single issue, parents are concerned about their child’s safety and the safety of their environment, whether it’s the food they eat, the air they breathe, or the cars in which they are driven. Yet when choosing where to send their child to school, the very serious and very real issue of how protected they will be by the shield of community immunity is not even on the radar for most parents. The few states that publish this information (California, Oregon, Vermont, and Washington) have done so after experiencing dramatic increases in parental vaccine hesitancy. These states also have been at the forefront of tightening the laws that mandate school vaccinations. Wider availability of this information would not only provide parents with valuable knowledge about the potential safety of their children, it would jump-start a national conversation about why this is such an important issue to begin with.
Overall, the United States does an excellent job vaccinating children against a wide array of devastating diseases that were once common causes of childhood illness, disability, and death. The nationwide immunization rate for the key preschool vaccines has held relatively steady near the target rate of 90 percent. This number is misleading, however, as it hides vast regional differences in vaccination rates. Fueled by the rapid spread of vaccine misinformation and the increasing belief in a host of vaccine myths, a growing number of parents are rejecting the recommendations of science-based medicine, choosing to alter the recommended vaccine schedule, or skip some or all vaccines completely. This rise in parental vaccine refusal and hesitancy has produced regional “hot zones” of under-immunization, placing all children at risk and leading to outbreaks of previously-contained childhood disease across the country. A high community vaccination rate (also called “herd immunity“) is necessary to prevent disease outbreaks. For most diseases the herd immunity threshold is around 90%. That means when community vaccination rates fall below this threshold, outbreaks are likely to occur. In this case, the most vulnerable in our communities are the ones most likely to suffer; those too young to be vaccinated, those who cannot be vaccinated due to health reasons, and those for whom the vaccines do not work (and of course those who are unvaccinated are also at risk, as you can’t hide in the herd). It is clear that the lower the regional vaccination rate, the more likely that region will be the source of a vaccine-preventable outbreak.
One stark example of the importance of herd-immunity is demonstrated by comparing two measles outbreaks that occurred in 2003, one in the Marshall Islands, and the other in Mexico. In the Marshall Islands, with a population of only 53,000, the immunization rate for measles was less than 90%. There were a confirmed 826 cases, 100 hospitalizations, and 3 deaths for a case rate of 1.6%. In Mexico, with a population of over 100 million (nearly 2,000 times the population of the Marshal Islands), the immunization rate exceeded 95%. Because of this high coverage rate, there were only 41 documented cases for a case rate of 0.00004%. In both outbreaks, most cases were in infants too young to be vaccinated or older children who had not been vaccinated.
2003 Marshall Islands
- Population 53,000
- Immunization rate below 75%
- 826 cases, 100 hospitalized
- Case rate = 1.6%
- 3 deaths
- Most cases in infants too young for vaccine, and older unvaccinated
2003 Mexico
- Population 100 million
- Immunization rate above 95%
- 41 cases
- Case rate = 0.00004%
- No deaths
- Most cases in infants too young for vaccine
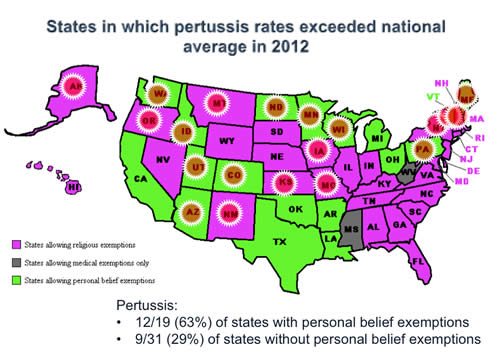
With the exceptions of Mississippi and West Virginia, every state allows a parent to claim a non-medical vaccine exemption for their child. Since valid medical contraindications to vaccination are rare, the rate of medical exemptions is low and has remained stable over time at around 0.5%. However, religious exemptions are allowed in 48 states and 18 states allow so-called personal belief exemptions (PBE). Of course, a religious exemption is a personal belief exemption, and the fact that there exists this distinction is ludicrous and likely unconstitutional as well, since it discriminates against atheists (hence the PBE in some states). On the other hand, there really is no large “main stream” religion that has an official anti-vaccine stance, except perhaps for Christian Science (there is no official anti-vaccine statement, though they traditionally prefer prayer over many medical interventions) and maybe the Dutch Reformed Church (it isn’t really clear). And then there are many small Christian sects that have shunned vaccination, sometimes with grave consequences. But this is really beside the point: it is absurd to allow religious doctrine rather than science to dictate public health policy. Unfortunately, it is shamefully easy for a parent to vaccine-exempt their child. Some states, like Michigan and California, have made it slightly more difficult for parents to take the steps necessary for claiming an exemption, resulting in a drop in exemption requests in some cases. But loopholes in these laws still make it quite easy for parents to avoid vaccinating their children. Unfortunately, we have ample evidence that with increasing vaccine exemptions rates comes increasing rates of disease. And while allowing religious exemptions is bad enough, and are clearly most often used by people without any religious beliefs concerning vaccinations, allowing PBEs makes matters worse. In 2012, pertussis rates exceeded the national average in 63% of states allowing PBEs, but in only 29% of states without PBEs.
Arkansas, like the rest of the country, has seen an increase in vaccine exemption rates over time. However, when that state began allowing PBEs (they call them philosophical exemptions), the rate increased sharply. What was interesting, though not surprising, is that as the overall exemption rate rose dramatically, the rate of religious exemptions declined. People could now exempt their children “honestly”, without claiming a religious reason, and this seems to have brought others out of the woodwork who might not have requested a religious exemption.
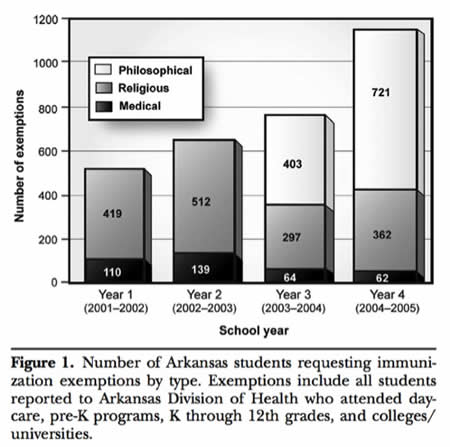
Thompson et al. 2007. “Impact of Addition of Philosophical Exemptions on Childhood Immunization Rates“. American Journal of Preventive Medicine, Volume 32, Number 3
While the exemption rate for the U.S. as a whole has remained relatively stable at 1.5 percent, there are danger zones of vaccine refusal where rates are much higher. In my state of Massachusetts, high-exemption-rate counties include Berkshire (3.2%), Hampshire (4.2%), Cape Cod (4.5%), and Franklin (6%). But this data is just too granular to see the even more dangerous hot-zones of under-vaccination. To get a better, finer picture of where disease outbreaks are most likely to occur, we need school-level data. We need to see the schools harboring the largest percentage of under-vaccinated children.
After working with officials at the Massachusetts Department of Health, Massachusetts has finally agreed to join California and several other states by making these data available to the public on its website.
For the reasons discussed above, the public availability of this information is crucial to our efforts to push back against the dangers of vaccine refusal. Unfortunately, the Massachusetts data is missing key elements critical to this effort. While I applaud the Massachusetts Department of Public Health (MDPH) for its work on this important project, they have been constrained by their own internal data release standards prohibiting the release of data for schools with fewer than 30 reported kindergarten students. (see the MDPH Confidentiality Procedures, Procedure 7). This includes the smaller, private schools that are so often the choice of the more affluent, educated, and “well-informed” parents most likely to hold anti-science, anti-vaccine beliefs, and to request vaccine exemptions for their children. The rationale for this policy is related to the fact that, with schools of this size, it becomes more difficult to protect the identities of children who may be vaccine-exempt. In other words, in a class of 20 children it is easier to guess which children may be claiming exemptions. I find this silly, and beside the point. Individual children would not be identified. What this policy does do is deprive parents of important information about the safety of their child’s environment. Honest, fair transparency would allow discussions to take place based on real-life, school-specific risk, and pressure could be placed on those parents who think they can hide in the herd. If every small, private school in my region can be declared “nut-free”, despite little evidence that this drastic policy is necessary to protect nut-allergic children, then surely at least revealing vaccination rates should be acceptable. But, of course, that is not sufficient. What we need is a complete reassessment of our priorities. It is time to eliminate all non-medical vaccine exemptions. It is time we stop pretending that the dangerous practice of not immunizing ones child is a choice worthy of respect and protection. In the meantime, some states are at least making it a bit more difficult for parents to exempt their children. In California, where the exemption rate has doubled since 2007, parents must meet with a provider to discuss the risks of their decision, and provide proof of that encounter as well as a written statement from them. In Michigan, exempting parents must meet with a local health worker to hear about the risks of underimmunization and sign a state form taking responsibility for these risks. A similar law has recently been enacted in Oregon.
As the data now stand, most Massachusetts parents have the information they need to determine if their child’s school is more or less likely to be the epicenter of a vaccine-preventable disease outbreak. But parents who send their children to the smaller private schools most likely to harbor unvaccinated children, are still in the dark.
The Massachusetts DPH has assured me that they will be taking a hard look at their data release policies, with the hope that they can be revised to allow inclusion of smaller schools, such as in California where data is released for schools with kindergartens larger than 10 students in size. In that case, we may soon have a true map of my state’s potential hot-zones for vaccine-preventable disease outbreaks. And parents can begin to have the conversations, and arguments, that need to be had.