A lot of medical specialties have throwaway newspapers/magazines that are supported by advertising and somehow mysteriously managed to show up for free in the mailboxes of practitioners. In my case, I’ve found myself on the subscription list for such papers about oncology, but also general surgery (I’m Board-certified as a general surgeon). When I have to recertify in about three years, it will be as a general surgeon, which was really fun to try to do last time after having specialized as a breast cancer surgeon, and will likely be even more fun next time, when I will be 10 years further out from my general surgery and surgical oncology training. In any case, that must be why, no matter where I end up working, sooner or later I end up receiving General Surgery News (GSN).
As throwaway professional newspapers go, GSN is not bad. However, occasionally it publishes op-ed articles that make me scratch my head or even tick me off with their obtuseness. Lately, apparently, it’s started some blogs. The one in particular that is the center of attention for this post is by Victoria Stern, is called “The Scope” and is billed as “exploring the lesser known sides of surgery.” Of course, it’s a bit odd that some of the first posts on this blog are about work hour restrictions and whether they leave new surgeons unprepared to practice surgery, the debate over breast screening, and what it takes to train expert surgeons, none of which are exactly “lesser known sides of surgery.” Work hour restrictions, in particular, have been discussed in surgery journals, at conferences, and among surgeons ad nauseam, particularly whether we are training a generation of surgeons unable to deal with the rigors of practicing surgery in the real world.
What caught my attention, though was a post from yesterday entitled “The Myth of Alternative Care, Growth of Complex Care“. Reading the title gave me a sinking feeling because whenever anyone mentions “complex care” in the context of alternative medicine, “complementary and alternative medicine” (CAM), “integrative medicine,” or whatever you want to call it, I know that a heapin’ helping of tropes and positive spin on pseudoscience is likely to be on its way. The reason, of course, is that CAM advocates love to argue that patient care is so complex that conventional medicine can’t adequately address it and needs some “help” from CAM. The article doesn’t “disappoint.”
Basically, Stern frames the post thusly. Alternative medicine is “bad.” No argument there. However, CAM is a different beast altogether. She starts with the standard CAM talking point that increasingly “patients are looking for answers outside of conventional medicine.” (Where have I heard that one before? Oh, yes. In pretty much every article and post spouting CAM apologia that I’ve ever read.) She then cites a 2006 study that has been blogged about before by someone near and dear to many SBM readers about the use of alternative medicine to treat breast cancer that pointed out the less than optimal (to put it kindly!) outcomes that result from such practices. She then quotes my good buddy and SBM fearless founder and leader Steve Novella, such that it becomes rapidly obvious that the post is set up to contrast “integrative medicine” with that nasty cancer quackery such that CAM/IM is a good thing:
“Alternative medicine is harmful,” said Steven Novella, MD, a neurologist and assistant professor at Yale University School of Medicine who is executive editor of the blog Science-Based Medicine. “If such alternatives were evidence-based at all, they would be considered medicine, not alternative medicine, and would be adopted into mainstream care.”
Complementary therapies, however, are a different ballgame altogether. Unlike alternative therapies, complementary interventions are not touted as cancer treatments. As the name implies, complementary modalities, such as vitamins and herbal supplements, massage, acupuncture, are meant to accompany mainstream care. The idea is to treat the entire patient, not just the disease.
Now there’s a total waste of a perfectly good Steve Novella quote.
Yes, there’s the granddaddy of CAM/IM tropes right there, the claim, either direct or implied, that CAM/IM, contrary to “conventional” science- and evidence-based medicine treats the “whole patient” (in this case the “entire patient”) and “not just the disease. This argument is, as I like to say, a pile of fetid dingo’s kidneys, because the implication is that you can’t treat the “entire” patient without embracing quackery such as acupuncture. A good primary care doctor using science-based medicine is a wholistic doctor who treats the “entire patient.” The same is true of a good oncologist practicing science-based oncology or a good surgeon practicing science-based surgery. The false dichotomy is plain: Either embrace the quackery that is CAM, or you are not treating the “whole” patient. Yes, it irritates the crap out of me, because I see it so much, and so few physicians directly question the assumption at the heart of a passage like the one above.
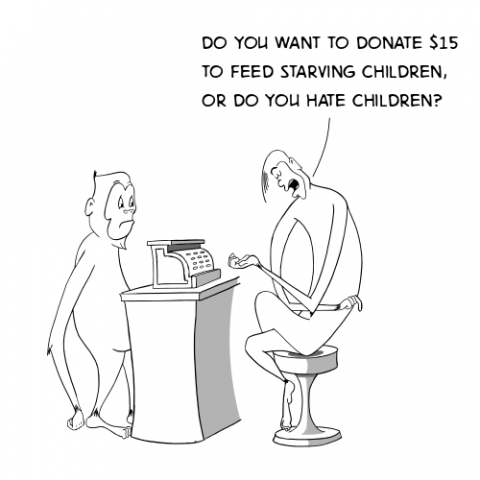
Let’s just put it this way. Whenever a CAM apologist says that she doesn’t practice that awful, nasty alternative medicine (which is quackery) and doesn’t recommend using it instead of conventional therapy, I respond, “That’s nice,” because that’s all it deserves. No one should be recommending foregoing effective science-based treatment in favor of magic and fairy dust. That is a bare minimum that we expect of physicians. However, when in the same paragraph (sometimes in the same sentence) I see advocates saying that it’s perfectly acceptable to add unproven therapies as an adjunct to conventional medicine (the “complementary” in CAM) or “integrating” them with science-based medicine, my teeth start to grind involuntarily. Bad reasoning has that effect on me. Think about it. A lot of the “respectable” CAM in integrative medicine derives from the very same pseudoscientific and prescientific ideas that are behind the quackery.
I like to use the idea of “energy healing” like reiki to illustrate the point. As I’ve written so many times before, reiki is finding its way more and more into academic medical centers as a “respectable” bit of integrative medicine. The key precept of reiki, as you will recall, is that reiki masters claim to be able to channel “healing energy” from what they call the “universal source.” Now, to drive the point home, let me suggest that you substitute the word “God” for “universal source.” See what I mean? Reiki is faith healing that substitutes Eastern mysticism for Christian beliefs. So, if faith healing is bad used alone, why is it suddenly “good” and “treating the whole patient” when used with standard treatment? The only reason I can think of is that at least the patient is getting standard treatment. That’s not enough. We shouldn’t be recommending the addition of ineffective treatments based on magical thinking to conventional treatment. Whether practitioners realize or admit it or not, acupuncture is based on similar prescientific ideas, given that qi (life energy) is supposed to be flowing through “meridians” (never mind that no anatomic structure has yet been discovered that corresponds to acupuncture meridians) and the needles are supposed to be “unblocking” or “redirecting” its flow for therapeutic effect. The same concept fits into chiropractic, as well, where removing subluxations is supposed to remove impediments to the action of “innate intelligence” healing the body. The list goes on and on and on of how vitalism is at the root of so many CAM treatments that are being “integrated” into medicine.
Unfortunately, Stern also incorporates another trope into her post:
In his surgical practice, Bruce Ramshaw, MD, FACS, chairman of the Halifax Health General Surgery Residency Program and co-director of the Advanced Hernia Solutions, Daytona Beach, Fla., takes a similar patient-centered approach to care. Dr. Ramshaw and his team, which includes a patient care manager, do not just treat hernias, they also try to understand their patients—what they really go through in their day-to-day lives as well as their fears and concerns about their health—offer potential solutions to diminish issues or anxieties, and involve family members in the process for added support.
In hernia repair and in medicine in general, there is no perfect way to treat each patient, said Dr. Ramshaw, but he hopes to come closer to an optimal treatment paradigm by applying this patient-focused approach to care. “Our goal is to form genuine relationships with patients,” Dr. Ramshaw said. (Read more about Dr. Ramshaw’s thoughts in his opinion piece, Love: Its Real Effect On Patient Care).
This kind of complex care that looks at the patient as a whole is becoming increasingly important not only for enhancing patients’ overall health, ensuring that they stay away from dangerous interventions and helping patients measure their expectations, but also as a way to create a true bond between physician and patient, an element of care that has been waning over the years. Although compassion and empathy won’t treat a person’s ailments, these traits can only help improve patient care and ultimately patient health.
Actually, there is little objectionable in Dr. Ramshaw’s article itself, other than its tendency towards a bit of “Patch Adams” sentimentality (although I note that he has written other things for GSN that I thought about blogging about before regarding “complexity theory” in medicine). So what is the problem? It’s not so much with Dr. Ramshaw as with what Stern does with his statements and articles. I think you can see it. Notice how CAM/IM is being conflated, without evidence, with measures that not only “treat the patient as a whole” but serve as a way to create a “true bond” between physician and patient. This is another massive false dichotomy. It is not necessary to embrace quackery to form a “true bond” between doctor and patient. Indeed, recommending treatments without good evidence behind them strikes me as potentially major impediment to forming such a “true bond,” at least if the patient ever finds out how thin the evidence base is for these treatments. In addition, what does it tell physicians practicing science-based medicine who can and do form “true bonds” with their patients without selling them fairy dust to tell them that such fairy dust is necessary to help them form such “bonds”?
Stern promises that her next blog will explore the “pros and cons of integrative medicine.” I can hardly wait.