In a recent post I shared a bit of my personal, near-death experience with measles during the US epidemic of 1989-1991. As I describe in that post, I contracted a very serious measles infection at the end of medical school, and was highly infectious when I interviewed for a residency position at Seattle Children’s Hospital. Like others my age who received an ineffective, killed measles vaccine between 1963 and 1967, I had not been adequately protected. The MMR vaccine was not yet available, and no boosters were recommended at the time. Unfortunately, though my measles titers (a test of immunity to measles) were checked when I entered medical school, the school’s student health department failed to notice or respond to the results – I was not immune and did not receive a booster dose at that time, as I should have. That mistake was huge, and could have cost me my life. It also caused me to potentially sicken many vulnerable children during my tour of the hospital, as well as others I may have inadvertently exposed during the window of communicability as I walked the streets of Seattle. The Department of Health had to be called to trace all of my steps and attempt to track down and protect any potential contacts.
Measles (or rubeolla) is a serious infectious disease caused by an RNA-containing paramyxovirus. The virus is primarily spread by respiratory droplet from a cough. Within two days of replicating in the nose and throat, it disseminates rapidly throughout the body. The incubation period is 10-12 days, after which the clinical manifestations of the disease begin. These early signs typically include escalating fevers, runny nose, cough, and watery, red eyes. Within a few days, the typical pink, blotchy measles rash begins at the hairline and spreads down the body, usually lasting for 5-6 days. While the initial signs of measles (the prodrome) resemble a bad cold, the illness quickly becomes much more severe. As a resident, we were taught that there is no such thing as a mild case of measles. Victims invariably look and feel horribly ill. Additionally, 30% of cases are associated with complications such as diarrhea, ear infections, pneumonia (5%), encephalitis (0.1%), seizures, permanent neurological impairment, and death (0.2%). The highest morbidity and mortality is seen in children under 5 and adults over 20 years of age. The mortality rate is approximately 0.2%, with death usually a result of pneumonia or encephalitis. Subacute sclerosing panencephalitis (SSPE) is a rare, degenerative brain disease that occurs several years following an episode of measles in approximately 5-10 cases per million reported cases.
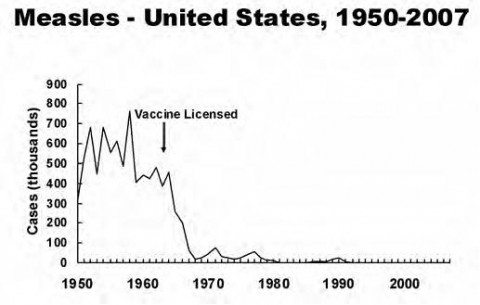
Prior to introduction of the measles vaccine in 1963, there were approximately 500,000 cases of measles reported annually in the United States, though it is estimated that the true annual incidence was more like 3-4 million. The disease reared its head in 2-3 year cycles, infecting nearly everyone at some point during childhood. Shortly after the vaccine was introduced, the incidence of measles plummeted by more than 98%, and the epidemic cycles ceased.
The combined MMR vaccine, covering measles, mumps, and rubella, was introduced in 1971, though still as a single dose. A booster dose at 4-6 years of age was recommended in 1989 when it was determined that over half of all school-aged cases of measles occurred in children who had already been vaccinated. The addition of this second dose for school-aged children raised the vaccine efficacy rate from 90-95% to 99.7%, and in 1983 there were fewer than 1,500 reported cases of measles in the United States. The epidemic that occurred in this country between 1989 and 1991 (my own illness included) resulted in over 55,000 cases and 123 deaths, and was largely a result of poor vaccination rates among black and Hispanic preschool-aged children living in high-poverty, urban areas. Ninety percent of deaths during that epidemic occurred in people who were entirely unvaccinated. A major campaign to vaccinate all preschool-aged children brought this crisis under control, and disease rates have declined since then. In 2000 measles was officially eradicated as an endemic disease in the United States. In 2004, a record low 37 cases of measles were reported, presumably all a result of importation from endemic countries.
Though this is a tremendous accomplishment, the successes achieved throughout the rest of the world are equally if not more encouraging. Within two years of successfully eliminating the transmission of measles in the United States, a relentless vaccination program conducted by the Pan-American Health Organization (PAHO) is close to achieving similar success throughout Latin America and the Caribbean. In 2011, the PAHO asked each member country to submit a progress report to verify the eradication of measles, rubella, and congenital rubella syndrome from the Americas. The CDC has just published this report for the United States, and has confirmed the sustained elimination of these entities. Once the other reports are in, the Western hemisphere will have verified an amazing, widespread public health accomplishment.
Similar successes are being demonstrated around the world. Globally, the coverage rate for the first dose of a measles-containing vaccine increased from 72% to 84% between 2000 and 2011. The number of countries providing a routine second dose increased from 97 (50%) in 2000 to 141 (73%) in 2011. During this period of time, the annual reported measles incidence decreased 65%, from 146 to 52 cases per million population, and the estimated number of measles deaths decreased 71%, from 548,000 to 158,000. All World Health Organization (WHO) regions of the world reported substantial reductions in mortality, ranging from 36% (India) to 90% (Western Pacific). Between 2000 and 2012, an estimated 13.8 million people worldwide were spared a measles-related death due to the Measles and Rubella Initiative, a global collaboration between the WHO and national infectious disease and control agencies. Still, hot regions of low vaccination coverage continue to challenge these efforts. According to the CDC’s report on the Global Control and Regional Elimination of Measles, 2000–2011:
Field investigations of recent measles outbreaks found most cases were among unvaccinated persons, suggesting the main underlying cause was persistent gaps in immunization coverage, despite overall increased measles vaccine coverage…All five countries with the largest number of infants who did not receive MCV1 [a single dose of measles-containing vaccine] through routine immunization services in 2011 had large outbreaks of measles during 2011, highlighting the importance of a strong immunization system.
Here’s where our success story takes a sick and ironic turn. Despite our triumph over these seemingly monumental challenges – dramatic drops in morbidity and mortality in the far corners of India and Africa, and the near heroic success of eliminating measles from places like Mexico City’s Neza-Chalco-Itza, considered the world’s largest slum – our hope of truly eradicating measles from the planet faces an additional but much more banal obstacle: educated, privileged, Google-empowered parents who fall for the pseudoscientific mythology of vaccine risk. Enlarging pockets of underimmunization due to vaccine hesitancy are threatening to derail our massive, worldwide efforts at controlling this and other horrendous diseases.
Vaccine hesitancy and refusal was largely responsible for the 189 confirmed cases of measles that occurred in the United States in 2013, the highest measles rate in 17 years. According to the CDC, most cases were in persons who were unvaccinated.
The trend shows no sign of breaking. Some of the more recent cases and outbreaks in the US highlight this problem:
- March 13, 2013: Brooklyn, NY – an intentionally unvaccinated 17 year old who became infected with measles while on a trip to London, initiated the largest outbreak of measles in the United States since 1996. A total of 58 cases were identified, all in an orthodox Jewish community of Brooklyn, NY. All cases occurred in intentionally unvaccinated individuals or in infants too young to be vaccinated.
- April-May, 2013, North Carolina – An unvaccinated traveler to India sparked an outbreak of 23 cases of measles. Most cases were among residents of a largely unvaccinated religious community in rural North Carolina. Most were unvaccinated.
- August, 2013: 20 cases spread through a Texas Mega-church, the leader of which preached about the dangers of vaccines. All cases occurred in families that chose not to vaccinate, and all of the infected children to had been home schooled.
- Feb 4, 2014: Measles confirmed in a graduate student at MIT who acquired the disease on a trip to South America.
- Feb, 2014: Five Counties in New York each reported one confirmed case of measles. Four of the five cases were unvaccinated:
- Feb 1, 2014: Rennselaer County, NY – A case of measles confirmed in a student at Rensselaer Polytechnic Institute (RPI). Multiple exposures may have occurred in a number of different settings beyond the college campus due to the student’s recent cross-country travel.
- February 4, 2014, Albany County, NY – An unvaccinated one-year-old child contracted measles on a trip to the Philippines. He was treated and potentially exposed people at a private medical practice and at the Albany Medical Center.
- February 7, 2014, Rockland County, NY – Another one-year-old unvaccinated child developed measles while visiting the Philippines and potentially exposed patients at a local medical office and a large shopping mall.
- February 7, 2014, Monroe County, NY – A University of Rochester student who contracted measles during a trip to the Republic of Georgia was treated at Strong Memorial Hospital.
- Feb 24, 2014: Orange County, NY – DOH issues Health advisory concerning a confirmed case of measles in Goshen, NY.
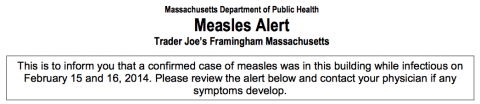
- Feb 24, 2014, Framingham, MA: two confirmed cases of measles potentially exposing many people at a Trader Joe’s, a local restaurant, a Bose Corporation office building, and a Harvard Vanguard medical clinic.
- Jan-Feb, 2014: California – 15 cases of measles have already been documented in California this year, mostly associated with travel to the Philippines and India. Most of the cases occurred in intentionally unvaccinated individuals or in infants too young to be vaccinated. Four of the 15 cases occurred in the Bay Area. This includes an unvaccinated man with measles who rode the San Francisco BART train between Feb. 4 and 7, potentially infecting many people in a particularly underimmunized region.
The human tragedy aside, outbreaks like these require extensive resources from state and local public health agencies, including thousands of hours of investigative labor.
As bad as it is in the United States, the creeping menace of vaccine denialism has taken root even more destructively in the United Kingdom. The UK reported 2,000 cases of measles in 2013, the highest level in 19 years. In the Swansea region of Wales alone, over 1,200 cases of measles were reported between November, 2012 and July 2013, and the numbers continue to rise.
It is clear that, while we have succeeded in eliminating endemic measles in the US, imported cases from other countries are creating outbreaks in areas where parents are altering vaccine schedules and outright refusing to vaccinate in increasing numbers. As discussed previously, the school vaccine exemption rate demonstrates wide geographic variability, from 0.1% in Mississippi to 6.2% in Washington State. But even this hides more extreme regional differences. There are some schools and school districts with much higher exemption rates and dismally poor vaccine coverage. Washington State publishes its school vaccination and vaccine exemption rates. A quick search of their DOH website reveals countywide exemption rates as high as 19%. California also publishes vaccination and personal belief exemption rates on its DPH website. Perusing this data is truly eye-opening and frightening. In Marin County, 7.8% of kindergarten students have been registered as vaccine-exempt by their parents. Some schools in the state have staggeringly high vaccine exemption rates. There is one in which the entire student body is vaccine-exempt. While vaccine exemption rates can tell us much about the trends in parental vaccine hesitancy, it underrepresents the problem. For example, it tells us little if anything about parents who alter the schedule without claiming a formal exemption. An altered schedule may technically meet school vaccine requirements, while still damaging herd immunity and increasing the population risk of disease.
Although the problem of parental vaccine hesitancy in the United States is of critical public health importance, it’s an issue that has been largely ignored. Parents who are concerned may be hesitant to bring it up, as it tends to polarize individuals within communities. While much emphasis is placed on the safety of our children’s environment, from the air they breathe and the water they drink, to the types of foods they eat and the way their fruits and vegetables are grown, few parents give any thought to whether their children are surrounded by the protective shield of community immunization. While this information should be an important consideration when deciding where to send one’s child to school, it isn’t on the minds of most parents, nor is this information typically made available. My state of Massachusetts does not currently publish this data. None of the parents I know have ever thought about the degree to which their children are protected by herd immunity in their school or community. If that data were made available, and the importance of community immunity discussed and pushed more aggressively by providers, public officials, and society in general, perhaps the dangerous trend of vaccine hesitancy would begin to shift. It would be a tragic shame if all of our efforts and dramatic successes were thwarted by the backward antiscience of parental vaccine denialism.
We have also arranged things so that almost no one understands science and technology. This is a prescription for disaster. We might get away with it for a while, but sooner or later this combustible mixture of ignorance and power is going to blow up in our faces.
– Carl Sagan (from The Demon Haunted World)