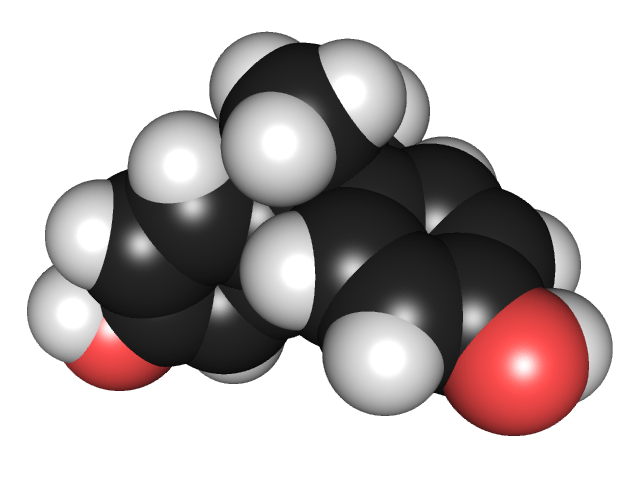
The molecular structure of Bisphenol A
Bisphenol A (BPA) is a chemical used in the manufacture of hard plastics which can be found in a wide range of products, including baby bottles, plastic utensiles, and plastic food containers. It has been the focus of some controversy over its safety, and the resulting debate reveals much about how the current system deals with such issues.
The concern is that BPA can leech from plastic containers into the food or liquid it contains, and when consumed can have negative health effects. The debate is over how to interpret existing evidence about BPA safety, which gives conflicting results. Essentially it is a debate about how to weight different kinds of evidence, and where safety thresholds should be.
The science of toxins
Toxicity is always a function of dose. Anything is toxic at high enough dose, and safe at a low enough dose. Regulatory agencies concerned with protecting the public health, therefore, typically use scientific evidence to establish doses that are likely to cause toxicity in humans and then set safe levels of exposure significantly below that level to create a buffer of safety. But what kind of evidence is used?
The only evidence that is considered direct evidence of cause and effect between a putative toxin and a specific toxic effect are randomized blinded controlled clinical trials. This is why these types of trials are considered the best type of evidence – variables are controlled for as much as possible, and they are done in a prospective manner.
Randomized controlled trials are the mainstay of evaluating the possible toxic effects of therapies, like pharmaceuticals. However, these types of trials ethically cannot be done on humans simply to assess the toxicity of a substance that has no potential therapeutic benefit. For example, you cannot perform a study that randomizes people to smoke to see if smoking causes cancer.
Therefore we must rely upon other types of evidence – all of which are imperfect. And this is what leads to debate over the question of toxicity.
One type of data is from animal studies – essentially doing randomized, blinded, controlled studies using animals instead of humans. The advantage of these types of studies is that they control for variables and can make specific conclusions about cause and effect. The weakness is that they are in animals and not humans. While some animals may be biochemically and physiologically similar to humans, there are always differences.
A second type of evidence is physiological/biochemical – searching for a potential mechanism by which a substance might cause toxicity. If such mechanisms match the actual toxicity seen in test animals, then a cause and effect conclusion is strengthened. Also, this type of evidence might be used to measure human exposure, absorption, how efficiently the toxin is cleared from the body, and its effects on cells in a dish or test tube. The strength of this type of evidence is that it is very reductionist – we learn what the chemical actually does. The weakness is that effects on cells in a dish does not always predict the effects of chemicals in a living system.
The third type is epidemiological evidence. The strength of this evidence is that it deals with humans and can assess toxicity that has actually happened in the real world with real people. The weakness is that it can be used to establish correlation only, not causation. This is because exposure is not randomized. For example, if you correlate a toxin with a disease, does the toxin cause the disease, does the disease increase the exposure to the toxin, or does some third factor increase both toxin exposure and risk of the disease?
Despite the fact that no one form of evidence is perfect, a consistent picture can emerge that points very strongly to a specific toxin causing a specific disease. We can say with a high degree of confidence that cigarette smoking causes certain types of lung cancer.
We can build to this confidence by showing mechanisms of toxicity that match what is seen in animal studies and epidemiological studies. Further, we can use triangulation to see if multiple correlations all line up and point toward one causal hypothesis. For example, if duration of smoking also correlates with cancer risk, and quitting correlates with a subsequent decreased risk, and smoking unfiltered has a stronger correlation than filtered, etc. then smoking probably causes cancer. If all the correlations predicted by the hypothesis that smoking causes cancer turn out to be true, then that interpretation is probably the correct one.
Controversies arise when all the evidence does not point in one direction. Then we can get into endless fights over which kind of evidence is more compelling, or which studies were better designed. This fighting, however, is often constructive, allowing the scientific, medical, and regulatory communities to sort out a large and complex body of evidence and try to make a reasonable judgment.
BPA
What does the evidence for BPA show? The FDA (whose job it is to review such questions) recently made public their assessment of all the scientific evidence for the toxicity of BPA. Here is an excerpt from the executive summary from their draft report:
FDA estimates that BPA exposure from use in food contact materials in infants and adults is 2.42 µg/kg bw/day and 0.185 µg/kg bw/day, respectively. FDA has determined the appropriate no observed adverse effect level (NOAEL) for its assessment of BPA to be the NOAEL for systemic toxicity of 5 mg/kg bw/day (5000 µg/kg bw/day) derived from two multigenerational rodent studies. This NOAEL results in adequate margins of safety of approximately 2,000 and 27,000 for infants and adults, respectively. The data reviewed on highlighted endpoints, such as the prostate gland and developmental neural and behavioral toxicity, were insufficient to provide a basis to alter the NOAEL used to calculate the margins of safety. FDA has concluded that an adequate margin of safety exists for BPA at current levels of exposure from food contact uses.
The FDA primarily relied upon animal data for its conclusion, specifically deciding that this type of evidence is the most useful for the question of BPA.
The National Toxicology Program (NTP) disagreed with the FDA. They believe that scientific studies showing that BPA can have hormone-like effects in the human body (specifically mimicking the action of estrogen) should be given more weight. Reviewing the same data they came to a slightly different conclusion. NTP Associate Director John Bucher, Ph.D. summarized their findings in an NIH press release:
“There remains considerable uncertainty whether the changes seen in the animal studies are directly applicable to humans, and whether they would result in clear adverse health effects. But we have concluded that the possibility that BPA may affect human development cannot be dismissed.”
The regulatory agencies of other countries also differ on their assessments of the safety of BPA. Canada has decided to take steps to limit human exposure to BPA, starting with a ban on baby bottles with BPA. The purpose of the ban is to err on the side of safety.
Meanwhile, the European Union is at the other end of the spectrum, going as far as saying that the US (referring to the NTP report) and Canada are using bad science to create unwarranted fears about BPA. In a recent update to their policy on BPA they write:
The conclusions of the Panel are that after exposure to BPA the human body rapidly metabolises and eliminates the substance. This represents an important metabolic difference compared with rats. EFSA will continue to monitor closely scientific findings regarding BPA and any related health effects.
They are pointing out one of the weaknesses of rat studies – differences in metabolism – and arguing that rat studies showing there is a risk are therefore flawed, and we should be reassured by the fact that humans rapidly metabolize and eliminate BPA from the body.
New JAMA article
One of the interesting aspects of such controversies is that the science is a moving target. This week an epidemiological study was published in JAMA looking at the levels of BPA in the urine of adults and comparing that to the incidence of several common diseases. Remember, this is correlation only and cannot, by itself, establish causation. What they found was:
Higher urinary BPA concentrations were associated with cardiovascular diagnoses in age-, sex-, and fully adjusted models (OR per 1-SD increase in BPA concentration, 1.39; 95% confidence interval [CI], 1.18-1.63; P = .001 with full adjustment). Higher BPA concentrations were also associated with diabetes (OR per 1-SD increase in BPA concentration, 1.39; 95% confidence interval [CI], 1.21-1.60; P < .001) but not with other studied common diseases.
This suggests that BPA exposure is associated with a higher risk of heart disease and diabetes. This is supported by mouse evidence suggesting that BPA can block the effects of a hormone that prevents obesity and diabetes.
Conclusion: Science will tell us if BPA is a health hazard
What we have is a vigorous debate among various scientific agencies about the relative merits of animal, toxicological, and epidemiological evidence for the risks of human exposure to BPA. I find this all a healthy part of transparent science. Slowly, debating the evidence and performing further studies will get us closer to the truth with greater confidence.
Given the existing evidence I suspect that there are real but small effects from BPA at current human exposure. These effects may be too small to worry about, but (and here is where most agree) more research is necessary.
The question that cannot be answered just with scientific evidence is where we should draw the line in terms of guaranteeing safety. There is no such thing as absolute safety or zero risk. Everything entails some risk. Everything we eat, drink, wear, drive, touch, and use comes with some finite risk. Most reasonable people would agree that we should avoid excessive risks and not worry about trivial risks – but much of the world entails the gray zone in between these extremes.
Also – eliminating something like BPA is not without risk either. What will take its place, and is that safe? BPA is used because it is cost effective and there are advantages to the durable plastic that is used in many products. What will we lose if we give up this technology?
Canada may decide to err on the side of caution, while the EU is happy that the current margin of safety is adequate. These are judgment calls not entirely answered by scientific evidence alone.
But good science and transparent debate will inform these judgments. And they will be endless.

