What do Tylenol, Excedrin Extra Strength, Nyquil Cold & Flu, Vicodin, and Anacin Aspirin Free have in common? They all contain the drug acetaminophen. Taking multiple acetaminophen-containing drugs can be risky: while acetaminophen is safe when used at appropriate doses, at excessive doses, it is highly toxic to the liver. Take enough, and you’ll almost certainly end up hospitalized with liver failure. Acetaminophen poisonings, whether intentional or not, are a considerable public health issue. In the USA, poisonings from this drug alone result in 56,000 emergency room visits, 26,000 hospitalizations, and 458 deaths per year. [PDF] This makes acetaminophen responsible for more overdoses, and overdose deaths [PDF], than any other pharmaceutical product.
Last week, Johnson & Johnson announced that it’s lowering the maximum recommended daily dose for its flagship analgesic, Extra Strength Tylenol, from 8 tablets per day (4000mg) to 6 tablets per day (3000mg). Why? According to the manufacturer,
The change is designed to help encourage appropriate acetaminophen use and reduce the risk of accidental overdose.
What’s an appropriate acetaminophen dose?
The dosage of any drug is based in part on its therapeutic window — the difference between the dose needed to cause a beneficial effect, and that which causes unwanted effects. In the case of acetaminophen, the limitation is how acetaminophen is eliminated from the body. Once ingested, acetaminophen is quickly absorbed from the gastrointestinal tract into the bloodstream. About 25% of the drug is immediately metabolized by the liver because of the first-pass effect. And the liver acts on the rest as it circulates through the body. Liver metabolism involves converting acetaminophen into substances (metabolites) that are easier to eliminate by the kidneys — and that’s where the risk of toxicity comes from.
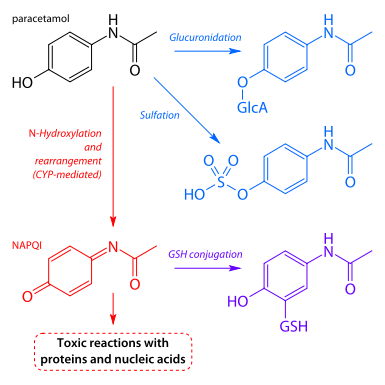
Multiple liver enzymes can act on acetaminophen. The main metabolic pathways, sulfation and glucuronidatation, transform acetaminophen into harmless products that can then be excreted in the urine. In overdosage situations, however, these pathways become saturated, and eventually exhausted — so other metabolic pathways kick in. Unfortunately, these other pathways create toxic versions of acetaminophen that attach to, and destroy, liver cells. So at normal doses, acetaminophen causes no toxicity. At high doses, liver injury is almost a certainty. This chart illustrates the science of metabolism and toxicity: blue is good, and red is bad.
(Paracetamol is another name for acetaminophen.)
What leads to poisonings?
While many acetaminophen overdoses are intentional poisonings, a substantial number of cases are unintentional. In adults, the maximum recommended daily dose has traditionally been 4000mg. That’s eight extra-strength (500 mg) Tylenol tablets, or twelve regular-strength (325 mg) tablets. A single dose of 7,500mg can cause liver injury, and consumption of 10,000 to 15,000 mg can be fatal. It’s important to note that 4000mg is the maximum daily dose from all sources — and that’s where many accidental poisonings come from. Combining cough and cold products, or taking too many painkillers, and bumping your total daily dose slightly over 4000mg in a single 24 hour period is unlikely to cause any harm. But take enough at once, or take regular moderately excessive amounts (say in the case of someone abusing Vicodin, Percocet, or even cough syrup), and unplanned overdoses can result. Chronic consumption of acetaminophen is is not uncommon: I’ve seen patients taking well over a dozen Percocet per day, for weeks or months — pushing acetaminophen consumption into the toxic range. They are surprised when I tell them my primary concern isn’t the narcotic consumption, but rather the huge amount of acetaminophen they’re consuming daily, which is almost certainly damaging their liver.
In 2009, the FDA held a series of hearings to address this issue of acetaminophen toxicity. (Harriet Hall covered it then.) It’s not a problem unique to J&J’s Tylenol. Acetaminophen is in hundreds of prescription and non-prescription products, and is used at all stages in life, starting in infancy: 28 billion doses of acetaminophen were consumed by Americans in 2005. Besides fever, headaches, and other everyday aches and pains, acetaminophen is the usual first drug of choice for treating chronic conditions like osteoarthritis. And hydrocodone-acetaminophen combination drugs (e.g., Vicodin) are among the most frequently prescribed drugs.
The FDA’s hearings resulted in an expert panel making several recommendations, including advice that the maximum recommended daily dose of acetaminophen should be reduced, to lower the likelihood that patients will exceed a safe daily dose. This recommendation was made despite some advice (PDF) to the contrary. So while there remains some debate about the toxic dose, it was felt this measure would reduce the incidence of poisoning.
Unexpected consequences?
From a public health perspective, we should try to reduce the risk of acetaminophen poisoning. Cutting the maximum daily dose of Tylenol Extra Strength should reduce the risk of poisoning in the event it’s combined with other acetaminophen-containing drugs. There’s even some evidence that suggests that 4000mg per day for prolonged periods may cause elevations in liver enzymes — data which led to the American Liver Foundation recommending (PDF) the maximum chronic dose should be 3000mg per day. So there may be a clinical rationale, too. But changing the maximum dose won’t mean much to consumers that don’t read the label. And from the individual patient perspective, forcing a hard maximum of 3000mg per day for all patients may have unwanted consequences, too. To start, you may need to take 650-1000mg of acetaminophen at a time to achieve analgesic effects beyond placebo. So achieving prolonged pain control, while also not exceeding 3000mg per day, may be difficult. Yet higher doses could be preferable to alternatives, such as anti-inflammatory drugs, or narcotics, especially when used regularly, for chronic conditions. So will the dose change have any measurable effect? Here’s your control group: The maximum dose isn’t changing in Canada.
Conclusion
Acetaminophen is a remarkably safe and effective drug when taken at appropriate doses, yet it is also the cause of hundreds of deaths per year. Manufacturers are now acting, based on the FDA’s advice, with the intent of reducing the chance of accidental poisoning. The pragmatic approach? Read labels and be cautious when combining different over-the-counter drugs. For most adults, keeping daily consumption below 4000mg is the safest approach to minimizing risk. And in some cases, a maximum of 3000mg may be more appropriate. But these are general approaches, that may not appropriate for everyone. A maximum dose of 3000mg make make sense at the population level, but may be problematic in terms of individual pain control. Regardless of the dose, if you regularly take high doses of acetaminophen, either alone or as a combination of products, a discussion with a health professional to discuss the risks and benefits may be warranted.