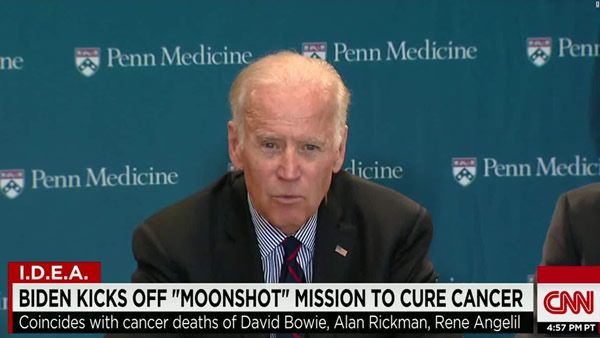
The Cancer Moonshot. It’s a topic that I’ve been meaning to address ever since President Barack Obama announced it in his State of the Union address this year and tasked Vice President Joe Biden to head up the initiative. Biden, you’ll recall, lost his son to a brain tumor. Yet here it is, nearly eight months later, and somehow I still haven’t gotten around to it. The goal of the initiative is to “eliminate cancer as we know it,” and to that end, with $195 million invested immediately in new cancer activities at the National Institutes of Health and $755 million proposed for FY 2017. My first thought at the time was that that wasn’t nearly enough money to achieve the ambitious goals set out by the President. That has now become particularly clear now that the National Cancer Institute has released the report from the initiative’s blue ribbon panel suggesting ten ways to speed up progress against cancer.
Initial thoughts on the Cancer Moonshot
When I first saw the President announce the Cancer Moonshot initiative several months ago, I couldn’t help but think that, although a very catchy title that would grab attention, calling the initiative the Cancer Moonshot was profoundly deceptive, probably unintentionally so but deceptive nonetheless. Why? The analogy between finding cures for cancer and going to the moon in the 1960s is profoundly flawed. The latter was primarily an engineering problem. The science, in particular the physics, necessary to achieve a moon landing was already adequately understood. What was needed was the technology to achieve the ambitious goal and the resources to develop that technology. In the Cold War era of the 1960s, in which the original moonshot was part of the geopolitical competition between the U.S. and the Soviet Union, it didn’t take much to direct resources to this end, resulting in a moon landing less than a decade after President John F. Kennedy, Jr. announced it.
The other reason that the analogy is deceptive is that the original moonshot was a much simpler problem to solve than cancer is. That’s not to say the original moonshot wasn’t a very difficult initiative, but cancer is orders of magnitude more difficult. As I’ve pointed out many times before, cancer is not just one disease. It’s hundreds. Even individual cancers are incredibly complex. Thanks to the power of evolution, tumors evolve into masses of heterogenous cells with different genetic makeups, such that tumor cells from a metastasis might well be resistant to treatments to which the primary tumor is sensitive. Breast cancers, for example, have been shown to harbor at least 1,700 different mutations, but only three of them showed up in at least 10% of patients, with the great majority of them being unique to each patient. Back in 2011, which was the 40th anniversary of President Nixon’s War on Cancer initiative, there was a spate of “Why haven’t we cured cancer yet” articles. I explained why. Cancer is not a single disease, and cancers are different. The mechanisms of carcinogenesis are not simple. Cancers evolve rapidly because of their genetic instability, leading to tumor heterogeneity. There are many more reasons, but those are the top three. Although, thanks to rapid advancements in gene sequencing and computer technology since the 1990s, the last two decades have produced massive quantities of data on the sequences of individual cancers, which genes are mutated and where, and how intracellular signaling pathways controlling proliferation, migration, and invasion are altered in cancer, at least thus far the effect on patient care has been far more modest.
None of this is to say that the Cancer Moonshot itself is a bad thing, only that, as has been the case for so many initiatives to “cure cancer” before, what it is likely to achieve is actually far more modest than what is being promised.
The Blue Ribbon panel’s report
When the news stories started coming out last week about the Cancer Moonshot, I naturally gravitated over to the National Cancer Institute website to get the details. The first thing I did was to look at who was on the blue ribbon panel. There’s no doubt that there are heavy hitters on the panel, whose names I immediately recognized, but there are also a fair number whom I had never heard of before. Be that as it may, the process is described thusly:
The BRP members were announced on April 4, 2016, and the first (virtual) meeting took place on April 11. At this meeting the members agreed to establish seven working groups to focus on major topic areas. The working group members were announced on May 2, and the groups met frequently until mid-July. In addition, the BRP met several more times—in person on April 18 and July 20, and virtually on July 13.
The working groups began with broad discussions of the state of the field for their respective topics and considered ideas from the members and the community at large. The panel considered more than 1,600 ideas submitted by the broader cancer community through a dedicated website, email, and other routes. Some working groups created subgroups with focused expertise in particular areas to carefully craft their recommendations. As the working groups narrowed in on their specific recommendations, the chairs of multiple groups also met to discuss cross-cutting themes and to merge similar topics into joint recommendations.
The BRP reviewed the working groups’ draft recommendations at its June 13 meeting and reviewed their final recommendations at its July 20 (in-person) meeting.
In other words, it sounds like a typical process for producing a white paper or set of evidence-based recommendations. The result was a 100+ page report, Research Opportunities for the Vice President’s Cancer “Moonshot“. I didn’t read the entire thing, given how long it was, but did hit some of the highlights, such as the Tumor Evolution and Progression Working Group Report. Each working group report is divided into nice bite-sized sections, including
- What is the recommendation?
- Where are we now?
- Where do we need to be (in 1-5 years)? (with priorities listed)
- Strategy: What will it take to get there?
- What does success look like?
The panel’s recommendations are also summarized in a short version and long version of the report, as well as in a video:
The recommendations include:
- Establish a network for direct patient involvement
- Create a clinical trials network devoted exclusively to immunotherapy
- Develop ways to overcome resistance to therapy
- Build a national cancer data ecosystem
- Intensify research on the major drivers of childhood cancers
- Minimize cancer treatment’s debilitating side effects
- Expand use of proven prevention and early detection strategies
- Mine past patient data to predict future patient outcomes
- Develop a 3D cancer atlas
- Develop new cancer technologies
Some of these recommendations are pretty uncontroversial. For instance, although more detail is given, who on earth would be against developing new cancer technologies? The rub, of course, is which new cancer technologies. Similarly, who would be against minimizing the debilitating effects of chemotherapy and other treatments? Or expanding the use of proven prevention techniques? For instance, tobacco use is the single largest cause of preventable deaths, and those deaths aren’t just due to tobacco-associated cancers like lung cancer. If smoking could be eliminated, as I’ve pointed out before, deaths from cancer would plummet because by far the most common cause of preventable cancer is tobacco, causing an estimated 86% of cases of lung cancer, 65% of cases of esophageal cancer and cancers of the oropharynx and head and neck, 37% of cases of bladder cancer, and 29% of cases of pancreatic cancer.
Uncontroversial recommendations aside, most of the recommendations are pretty measured and well thought out, although at least one appears to be a result of a current scientific bandwagon effect. Let’s take a look.
Selected Cancer Moonshot recommendations: Immunotherapy
The first thing I noticed when I read the Cancer Moonshot Blue Ribbon Panel report, is that there wasn’t anything particularly bold about it, the effusive praise heaped on it by the American Society of Clinical Oncology (ASCO) notwithstanding. Personally, if this weren’t called the Cancer Moonshot, I wouldn’t think that was a bad thing, but rather a good thing. In actuality, the report is a synthesis of where cancer research is right now and where it is going rather than any sort of bold vision of where it should go. Again, that’s not a bad thing. Martial rhetoric, exaggerated promises, and analogies to massive scientific efforts of the past have always been at odds with the evolutionary and incremental nature of cancer research; so a report that proposes, in essence, to take the technology and science we have today and to build on it is the best that is likely to be expected, even if it’s a bit boring. In retrospect, I wish I hadn’t skipped this year’s ASCO meeting because I could have seen Vice President Biden give his pitch for the initiative.
The first recommendation that leapt out at me was definitely the recommendation for a clinical trials network devoted exclusively to immunotherapy. Yes, that’s the one that’s clearly based on a current scientific fad. My guess is that, if the Cancer Moonshot Blue Ribbon Panel had been convened in the 1990s it would have included an initiative to investigate antiangiogenic therapy (therapy that targets blood vessel development). Is immunotherapy a big enough deal to rate one of the ten major recommendations of the panel and a recommendation for a national clinical trials network devoted solely to immunotherapy? Maybe, but over the years I’ve become a lot more skeptical, remembering all the hype and promise of antiangiogenic treatments in the 1990s and the previous wave of immunotherapy hype in the 1980s. (That’s what happens when you get to be a bit of an old fart.) Those memories temper my enthusiasm.
On the other hand, there’s no doubt that a new class of drugs, immune checkpoint inhibitors, is a big deal. There are lots of other forms of immunotherapy that have been developed. For example, there are humanized monoclonal antibodies against specific cancer targets (like Herceptin). There are cell-based therapies, some of which I saw when I was a resident in the late 1980s and early 1990s. There are dendritic cell therapies. There are also cancer vaccines, which have had pretty mixed results and are mostly still experimental. There are vaccines to prevent cancer, the most successful of which is, obviously, HPV vaccines such as Gardasil and Cervarix, which prevent cervical cancer by preventing infection by the most common HPV types. To be honest, though, my assessment of these other forms of immunotherapy is that they’ve had fairly limited success over the last 30 years, other than Gardasil and Herceptin, and I consider Herceptin to be targeted therapy more than immunotherapy. Immune checkpoint inhibitors are different, though. These days, when a cancer researcher (and, truth be told, the Cancer Moonshot Blue Ribbon Panel) say “immunotherapy”, what they really mean are mainly immune checkpoint inhibitors.
One of the most critical components of the immune system is the ability to distinguish between what is “foreign” and “self.” The main job of the immune system is to leave self alone and to attack foreign invaders, such as bacteria. Obviously it’s a lot more complicated than that, because we have trillions of bacteria that live on our bodies in relative harmony with us, but for purposes of this discussion it’s not necessary to go into that more deeply. The problem with cancer, of course, has always been that cancer at least starts out as “self.” It is our own cells. When they become cancerous, some tumor cells are indeed recognized as no longer being self, but some cancers are very good at evading the immune system, often by tricking these immune checkpoints. Immune checkpoint inhibitors target proteins controlling these checkpoints, such as PD-1, which normally acts as a type of “off switch” that helps keep the T cells from attacking other cells in the body. Immune checkpoint inhibitors are one of the most promising classes of new drugs in the pipeline.
The report states:
The success rates of first-generation cancer immunotherapies, such as checkpoint inhibitors, genetically engineered T cells, and new immune activators have improved remarkably over the last 10 years, resulting in durable, long-term survival—and, in some cases cures—for a subset of patients with advanced cancers such as melanoma, blood, and lung cancers. However, only 10-20% of patients with these cancers have long-term responses to current immunotherapies. We must learn why some patients who have melanoma (such as President Carter) or lung cancer respond to checkpoint blockade immunotherapy, whereas patients with many other types of adult cancers, including ovarian, breast, pancreatic, brain, and prostate cancer—as well as most pediatric cancers—have brief responses or do not respond at all.
Same as it ever was. One could say the same thing about many targeted therapies. I’m not sure I would have devoted a whole national clinical trials network to just immunotherapy. I would have thought bigger and included all targeted therapies, as I tend to agree with cancer researcher Vinay Prasad:
Immunotherapy refers to promising new drugs that harness the body’s immune system to fight cancer, and indeed these have generated impressive outcomes for some patients. But with dozens of immunotherapy studies underway, that rocket has already lifted off, and it’s unclear what Biden’s moonshot can add. And, unfortunately, the bitter reality is that despite immunotherapy’s promise, its benefits will probably remain confined to a minority of patients with certain types of cancer. Immunotherapy is unlikely to be a panacea.
In other words, there is nothing about immunotherapy that is likely to be the “magic bullet” that some portray it as.
Selected Cancer Moonshot recommendations: Clinical trials
I was heartened to see in the panel’s recommendations establishing a network for direct patient involvement, building a national cancer data ecosystem, and mining past data to learn to predict patient outcomes. One of the most pressing problems confronting cancer research is recruiting patients to clinical trials to test new therapies. Thus, I like hearing things like:
This recommendation calls for cancer patients to join a new national network that, with appropriate privacy safeguards, will provide them with a genetic profile of their own cancer and let them “pre-register” for clinical trials, so they can be contacted when a trial for which they may be eligible opens. Researchers will be able to access patient outcomes reported in the network database to conduct studies on what treatments work, in whom, and in which types of cancer.
And creating an ecosystem to facilitate cancer research:
Technology has enabled the collection of a massive amount of patient data. But these data are often stored in proprietary databases or accessible only to a select group of people, limiting their usefulness as a research resource. A national ecosystem that links many of the nation’s largest data repositories would enable one-stop, free access for researchers, doctors, and patients to share data on cancer and fuel faster progress.
Smaller countries, with national health care systems, already have such outcomes data that researchers can mine. The fragmentation of the US health system and a lack of will to make such a database a priority have long been an issue. Also, such a database and encouragement to patients to empower them to be more involved in their own care by having access to their genetic profile could increase patient enthusiasm for research.
Similarly, what about mining past data for the purpose of hypothesis-generation?
Understanding why some patients with the same type and stage of cancer, and same treatment may end up with different outcomes continues to be a research challenge. Analysis of existing tumor tissue from patients who received standard-of-care treatment, stored at biobanks around the country, may enable discovery of genetic and other factors that distinguish which individuals would bene t from standard care versus experimental treatment in a clinical trial.
We have an enormous resource in the form of existing patient samples. It just hasn’t been adequately mined. However, I can’t help but echo cancer researcher Vinay Prasad’s skepticism when the Cancer Moonshot initiative was first announced:
Another oft-mentioned proposal is harnessing the power of big data. One such idea is to closely examine what therapies have worked for individuals and which unique genetic traits allowed those therapies to work, and then extend these findings to other patients. Unfortunately, such an approach is fraught with limits. My colleague Andrae Vandross and I recently reviewed the published reports of patients who have had an exceptional response to a cancer drug. In many instances, we found that these patients responded unusually well not only to the studied drug but also to older ones. In several cases, these people had already survived far longer than the typical patient by the time they received the lauded medication. It is hard, then, to conclude which patients have great outcomes because of a drug and which simply have slow-growing cancers — a phenomenon doctors have recognized for years. But this distinction is the very crux of the big-data approach. Observational data — no matter how “big” — will have difficulty overcoming this challenge.
The other trouble with big data is that if we agree that the outcomes we have now are mediocre (and I think we can agree on that), studying these outcomes in greater detail is unlikely to result in truly transformative approaches. It would be like NASA scientists studying old nautical voyages to figure out how to reach the moon.
I’m not as pessimistic about big data approaches a Prasad is, but I do share some of his skepticism. We’ve been trying big data approaches using genomic data for over 15 years now, and thus far we haven’t found anything truly transformational. Again, to me that’s not a criticism of using big data approaches. Such computational approaches are and will be very useful in cancer research. It’s just that they are and will be very useful in an incremental fashion, and they are prone to pitfalls that have plagued cancer research since cancer research began. In cancer, we frequently point out that biology is king. If you’re lucky enough to get a “good” cancer, chances are that you will tend to do well no matter what treatment is used. (Most alternative cancer cure testimonials consist of patients with “good” cancers.) If you’re unlucky enough to get a nasty cancer, chances are that you will do poorly regardless of treatment. I don’t see anything in the “big data” proposals that will overcome that. However, I also don’t think that better tools for hypothesis generation and to improve patient participation are a bad thing. They’re just not transformational.
The overall problem
I don’t see much reason to go into a lot of detail about the other recommendations. As I said before, most are not particularly controversial. Certainly none of them are transformational, including developing strategies to overcome resistance to anticancer therapies (a research priority that’s been a priority ever since anticancer therapies entered the field), minimizing side effects (a long-neglected priority that has come to the fore already in the last five or ten years, no “moonshot” required), expanding the use of prevention and early screening (the latter, of course, is not without risks, such as overdiagnosis and overtreatment), intensifying research into the drivers of childhood cancers (which basically says right there that it’s just ramping up what we’re already doing), or developing new technologies to fight cancer (which is something cancer researchers have been doing since time immemorial).
I will admit that I found the proposal to develop a 3D and 4D cancer atlas to be kind of cool:
Oncologists today rely on past experience, consultation with multidisciplinary teams, published studies, and other sources to make diagnosis and treatment decisions. Providing a web-based catalog of the genetic lesions and cellular interactions in tumor, immune, and other cells in the tumor microenvironment that maps the evolution of tumors—from development to metastasis—will enable researchers to develop predictive models of tumor progression and response to treatment that will ultimately help oncologists make informed treatment decisions for each patient.
The “4D” aspect, discussed in the more detailed report, involves rerecording the same data over time for individual patients. The problem with such an atlas, however, is the same problem with all of “precision medicine,” namely that we don’t yet know what to do with all the mountains of information gathered for them when it comes to applying all that data to individual patients. That leads me to wonder if the effort and expense necessary to build such a tool will pay off.
I realize that to persuade politicians to fund an effort it’s often necessary to sex it up and make it appealing. I also know that slow and steady incremental advancement is far less sexy than a “moonshot”-style effort, as in a massive surge of resources and effort directed at a single focused goal. Unfortunately, the whole concept of a “moonshot,” while well-suited for focused engineering problems such as landing a human being on the Moon, is poorly suited to a problem like “eliminating cancer as we know it,” which, by the way, is a poorly defined goal. You might remember the then-director of the NCI, Andrew Von Eschenbach, making the goal of the NCI to “eliminate suffering and death” from cancer by 2015. Well, it’s now 2016, and there’s still plenty of suffering and death from cancer in the US. Indeed, I remember attending a meeting of the American Association for Cancer Research in 2003 or 2004, where I attended a talk by Von Eschenbach and thought, “What is this guy smoking?” That was pretty much the reaction of every researcher with whom I spoke about his talk. The point is that making promises like that, framing cancer research as a “war” (which implies someday winning), or selling the idea that a concentrated “moonshot”-style effort can eliminate cancer is the wrong message.
Cancer is not a focused problem. It’s many hundreds, if not thousands, of problems, many interrelated, some not, that require many different solutions. Progress in cancer research, like science, will always be incremental, resistant to surrendering to victorious scientists and physicians the way Germany and Japan surrendered to the Allies in 1945, resistant to promises to eliminate it in 12 years, and certainly resistant to focused “moonshot” efforts to solve it. That doesn’t mean that there aren’t some good ideas worth implementing in the Cancer Moonshot, nor does it mean that it wouldn’t be worth increasing cancer research funding significantly, given the decrease in real purchasing power of the NIH and NCI budgets since 2004. Invested wisely, such funding could certainly contribute to real advances. The problem is, as with all science, it’s very difficult to predict where, when, or how such advances will manifest themselves or even what they’ll be. All we do know is that they’ll come about through incremental progress based on prior research. Unfortunately, that message is not one that’s as appealing as that of the Cancer Moonshot.