Thanks to a hot tip from a follower on Twitter, I’ve once again found myself neck deep in chiropractic propaganda involving the care of a pediatric patient. The case as presented involves, among numerous specious assumptions, claims of successfully treating an infant’s paralyzed arm using chiropractic philosophy and spinal adjustment techniques. As I will explain in detail, this “miracle” is just another in a seemingly endless stream of emotional but worthless anecdotes being used for marketing purposes.
I’ll be discussing two videos, uploaded to YouTube by a father who wants to tell the world about the miracle of chiropractic. He uses that word a lot, in fact, assigning the label to no less than four outcomes and clearly setting the bar lower than my own personal threshold. The videos are a few years old, but have over 150,000 views and can still be found linked to on numerous websites and discussed in interviews. If you’re feeling generous, they serve as excellent examples of how the mind of the believer works when facing uncertainty regarding the health of a loved one.
I will provide a general synopsis of the events in question, but I do recommend watching the videos despite the fact that you will never get those 18 minutes back. They contain the details of the case and, particularly in the second video, some great examples of typical chiropractic tactics and buzzwords.
A Chiropractic Miracle, Part 1
A Chiropractic Miracle, Part 2
The case of the baby with the paralyzed arm
In the introduction to video #1, a common scenario that I see frequently as a newborn hospitalist is described. After a lengthy trial of labor, a pregnant woman is taken to the operating room for a C-section because fetal monitoring has revealed the possibility that the baby is in trouble. In addition to the baby’s unstable heart rate, the mother has developed a fever and is at high risk of infection herself, which might also adversely affect the child.
These situations can be difficult. Obstetricians often must recommend surgical intervention in scenarios such as this based on imperfect monitoring technology and without certainty of benefit. They don’t have a crystal ball that reveals whether or not a baby will suffer serious injury or die if an attempt to deliver vaginally is continued, and C-section delivery can increase the risk of a bad outcome for mother even while it reduces the risk for the child.
Mothers frequently have to make a very brave choice. C-sections are scary and they can significantly complicate the recovery process, lengthen the hospital stay by 2 or more days, interfere with successful breastfeeding, and in uncommon circumstances result in unexpected maternal injury and even death, although the likelihood of that is extremely low. Choosing to shoulder this greater burden of risk in order to protect their unborn child is, in my humble opinion, heroic. Unfortunately, the current push for so-called “natural” birth has made this decision even more challenging because of increasing societal pressure for mothers to deliver vaginally and preserve a desired experience. There are also articles like this, written by an acupuncturist and “ancestral health specialist”, that may seem reasonable to a lay audience but grossly exaggerate the risks.
In this particular case, the C-section was complicated by a difficult extraction when the baby was found to be impacted in the pelvis. This isn’t uncommon. Sometimes the incision must be made bigger, which is not called “a double c-section” by the way, and sometimes obstetricians must use a vacuum device in order to help pull the baby from the abdomen. I recently learned from Jen Gunter that nitrous oxide can also be administered to relax the muscles of the uterus. But never is a delivery table “inverted to use the forces of gravity.”
With such a difficult labor and delivery, I’m not at all surprised that the baby was a bit stunned and required some assistance with respiration initially. 10% of babies in general need intervention from trained (ideally) professionals to begin breathing and 1% need significant medical intervention to establish breathing and an adequate heart rate. The father states that it took two minutes and forty one seconds to resuscitate his baby, but no further detail is provided.
I doubt that the baby actually required more than standard resuscitation, at most a brief application of positive pressure ventilation with a bag and mask. He shows a picture of himself holding his swaddled newborn in the delivery room and I don’t see a breathing tube or any umbilical lines. What he refers to in the video as “the first of four miracles,” that his child began to breathe, I call human physiology and basic NRP training.
She does have a right hand peripheral IV, which also isn’t surprising considering she was observed in the NICU for a bit. Brief observation in the NICU is often done as a precaution after difficult deliveries, and PIVs are quickly removed once the baby feeds and demonstrates normal breathing patterns. I bet she was watched for a few hours and then deemed ready to go to the newborn nursery.
The father goes on to describe the birth injuries that resulted from the difficult extraction of his daughter. She had some bruising and evidence of injury to the right side of her neck, which would eventually be diagnosed as congenital muscular torticollis (“wry neck”), and what appears to be a very mild left positional foot deformity. She also demonstrated a lack of movement of her right arm, likely caused by forceful stretching of her neck during delivery, but I doubt that the father was told that his baby’s right arm was “completely paralyzed” with the implication that it was permanent.
In the second video, which was published a year and a half after the first, additional details are given that involve him being told by hospital doctors that she would likely need surgical correction of her torticollis. I find this odd considering that most patients recover with gentle stretching, physical therapy is highly successful in more significant cases, and surgery is required in less than 5% of patients, generally for the most severe presentations or when the condition is diagnosed after a year of age.
Parkland Memorial hospital in Dallas delivers more babies than anywhere else in the United States, something like 35-40 babies every day. They have seen everything a thousand times. I do not think that anyone there would outright state or even imply something as inaccurate and anxiety provoking as “torticollis surgery would result in a straight neck but the inability to turn her head to the right for the rest of her life.” Human memory is such that I take recollections of stressful events that took place three years (2nd video) or even twenty months (1st video) ago with a huge grain of salt.
What is a newborn brachial plexus injury?
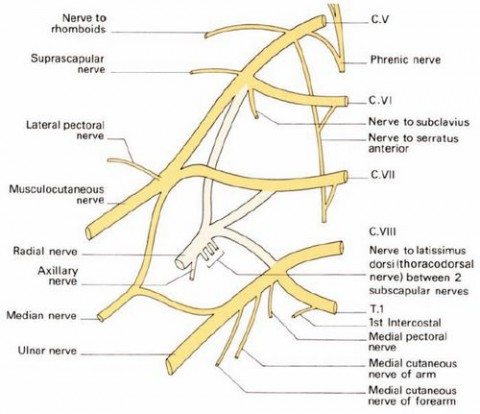
The brachial plexus is a collection of spinal nerve roots, and the complicated collection of peripheral nerves they feed into, originating from each side of the cervical and upper thoracic spine. Memorizing the names, locations, and muscular innervation from the brachial plexus also serves as a medical school rite of passage during first year anatomy. The brachial plexus ultimately innervates the muscles and skin of the shoulder and arm, and injury to some or all of the involved nerves results in classic patterns of weakness, paralysis, and sensory loss, such as Erb’s palsy. And although injury to the brachial plexus can occur during a routine delivery from forces related to uterine contractions and maternal pushing, the biggest risk factor is generally accepted to be forceful lateral traction on the neck during difficult deliveries such as described above or when a vaginally delivered baby becomes stuck at the shoulders.
Brachial plexus palsy is primarily a clinical diagnosis. Even MRI is unreliable in differentiating the type and severity of injury in newborns, so giving parents a specific prognosis can be challenging. In general, decreased or absent movement is the result of stretching of the nerves and subsequent diminution or failure of conduction. This can occur with transient loss of the fatty insulation around otherwise intact axons or, in the most severe cases, when entire nerves are ripped out of the spinal cord.
Newborn brachial plexus injury isn’t common, occurring in only 0.15% of deliveries overall but in up to 17% of vaginal deliveries where the baby is stuck at the shoulders. I’ve seen a handful of cases over the past 13 years, with most being on the milder end of the spectrum. I’ve never personally discharged a newborn home with a completely paralyzed extremity.
Roughly half of presentations of newborn brachial plexus injury involve a characteristic pattern known as Erb’s palsy. In these cases, the baby’s arm is internally rotated, straightened out, and held against the body because of weakness in the shoulder and upper arm. In another 35% of cases, the Erb’s palsy is accompanied by additional injury that affects the wrist and hand, which is known as “waiter’s tip” positioning.
Involvement down to the fingers is uncommon but it does happen. Not surprisingly, fractures of the clavicle and humerus are occasionally associated with brachial plexus injuries, as are injuries to the shoulder and cervical spine, even true (non-chiropractic) subluxations. These injuries can mimic or exacerbate brachial plexus injury.
Spontaneous and complete resolution of newborn brachial plexus injury is the rule rather than the exception. Even when babies initially have little to no movement of the involved arm, the prognosis is good. Although imperfect, the general consensus is that any improvement seen in the first few post-natal weeks, even just wiggling the fingers, is seen as a predictor of eventual recovery.
Some children, even when early improvement is documented, do go on to have permanent deficits however. Treatment in more severe or persistent cases typically involves physical therapy to prevent muscle tightening, and to maximize strength and function, and sometimes surgery to reconnect nerves. Surgery can help but often does not result in the recovery of full function.
What is congenital muscular torticollis?

A right sided congenital torticollis
Torticollis or “wry neck” occurs when a patient has difficulty maintaining the head and neck in a neutral position, which results in a typical appearance of having the head persistently turned to one side. There are a number of potential causes at varying ages, but the most common is direct injury to the sternocleidomastoid muscle that occurs prenatally or during a traumatic delivery. The injured muscle tissue is replaced with scar tissue that makes it shorter and tighter, and may result in a palpable lump.
If the right muscle is injured, for example, the head is usually bent towards the affected side but turned to the opposite. Conservative treatment is almost always effective, resulting in complete recovery of neck movement, especially if started within the first several weeks of life. Stretching exercises can be done at home by caregivers and techniques can be implemented to encourage infants to move their head to the both sides on their own. Sometimes more intensive physical therapy is required and very rarely surgery, which treats rather than results in the inability to turn the head. Prognosis is excellent even in the most severe cases, and full recovery usually occurs within 6 to 12 months.
Now back to our case.
A chiropractic miracle story or a tall tale?
The father describes calling a chiropractor friend and business partner, who came to the hospital to treat his daughter that day. Within only three hours of an Activator adjustment, they saw the first movements of the right arm, and there was “complete resolution” on day 2 after additional adjustment. He relates how the hospital staff was in disbelief, and once again I doubt that his daughter’s doctors would really say the words that are being put into their mouths. This “second of four miracles” is more reasonably explained by the natural course of this kind of injury and some exaggeration of the severity by dad.
The “third of four miracles” was the treatment and resolution of his daughter’s torticollis within a year of birth. He naturally gives credit to a “highly recommended area chiropractor,” likely because of her DICCP certification and the four entire days she spent learning birth and post-partum pediatrics, who adjusted his daughter weekly for a full year for $5,000. They saw improvement by 8 months and resolution by the end of her first of year of life, which is the expected course for most cases when treated with gentle stretching regimens.
Finally, his “last of four miracles” is the resolution of his daughter’s mild positional foot deformity, which appears to be a calcaneovalgus foot. I’ve seen hundreds of these and they almost always resolve within a month or two without any intervention. He doesn’t outright claim that chiropractic played any role in the improved positioning of the left foot, but I think it’s implied. See what you think. There are plenty of chiropractors that will adjust subluxated feet, however.
What really happened?
Many babies with brachial plexus injuries, and I suspect that the child in this case is one of them, show signs of significant improvement in the first few days of life. That is the natural course of milder injury as nerve swelling and slowed conduction begins to improve. The time to full recovery is variable, but I have seen babies have significant improvement and apparent return to full movement of the arm prior to discharge.
I don’t doubt that most of the facts given in the two videos are accurate. An emergency section was called for which was traumatic and resulted in some injury to the baby. She likely had a mild brachial plexus injury that resolved on its own. She was eventually diagnosed with congenital muscular torticollis, which also resolved on its own or with simple stretching that was recommended by the chiropractor or the child’s medical doctor. Nothing specific to chiropractic played a role in the child’s recovery.
Of course we don’t have access to medical records, so we are relying on the potentially biased recollections of the father that may have become warped or exaggerated over time. It is entirely possible that the child never really had a complete absence of movement in the right arm. One clue that this may have not been as severe as dad is recalling is that peripheral IV. It’s in the baby’s right hand. Generally we don’t do any manipulation of the extremity when severe brachial plexus injury is suspected.
Even assuming that dad’s memory is accurate, the pathophysiology of brachial plexus injury is fairly well worked out in newborns. Stretching is by far the most likely etiology, not the dislocation of multiple cervical and thoracic vertebrae pinching the spinal nerves as they exit their respective spinal canals. That would be an extremely rare and severe injury, clearly evident on plain x-ray, which would not resolve in a couple of days by lightly thumping on the side of the neck. It has near-homeopathy level plausibility.
We also know the pathophysiology of congenital muscular torticollis. It is caused by injury to a specific muscle in the neck and subsequent fibrosis. It is not related to the position of the spine and, again, light thumping on the neck with an Activator could not possibly play a role in its resolution.
Finally, and I thought long and hard about whether or not to include this, the father in these videos is Chris Burfield who, is not a chiropractor but is a chiropractic strategic marketer who builds self-described “Propaganda Marketing Machines.” Here he is discussing how to case medical doctors’ offices for clues about their personalities and other “sneaky ninja” tactics to trick them into setting up appointments to discuss patient referrals. Here is one of Burfield’s websites where he discusses making and selling viral videos to spread the word about chiropractic. In this 2015 podcast interview, he discusses his daughter’s case and then how to use YouTube videos as marketing.
His career, and even examples of him discussing the use of YouTube viral videos to promote chiropractic, do not mean that he is intentionally misleading the public. It does seems shady, but I mention this more as an example of how one’s personal biases can mold our interpretation of events and even our memories over time. I found Burfield in a discussion on a Facebook marketing page stating that chiropractic brought his daughter’s paralyzed arm “back to life.”
Conclusion: The propaganda machine keeps on spinning
We will never know exactly how Burfield’s daughter presented after her traumatic delivery. Without access to the medical record, we will never know exactly how her condition was discussed by the treating physicians. Ultimately, as a pediatrician, a father, and a human being, I’m very happy that she recovered seemingly without incident.
Not every patient is so lucky. Putting faith in pseudoscience such as chiropractic philosophy can be dangerous. Depending on the technique used, a brachial plexus injury could be worsened and even made permanent if the nerves are further stretched. And injury to the neck, although uncommon, has been documented when chiropractors attempt to treat torticollis.
Finally, and I realize I’m adjusting a dead horse here, chiropractic marketing tactics are manipulative and shameless. I honestly don’t understand how they look patients in the face when using their memorized scripts or sleep at night after a day of pestering medical doctors in their offices or people at health fairs or shopping malls. Don’t fall for the hype.

