In any case, over the last three months, Steve Novella and I published a solid commentary in Trends in Molecular Medicine decrying the testing in randomized clinical trials of, in essence, magic, while I managed to score a commentary in Nature Reviews Cancer criticizing “integrative oncology.” Pretty good, right? What do I see this month in the Journal of the National Cancer Institute (or JNCI, as we like to call it)? An entire monograph devoted to a the topic, “The Role of Integrative Oncology for Cancer Survivorship”, touting integrative oncology, of course. And where did I find out about this monograph? I found out about it from Josephine Briggs, the director of the National Center for Complementary and Alternative Medicine (NCCAM) herself, on the NCCAM blog in a post entitled “The Evidence Base for Integrative Approaches to Cancer Care“, in which she touts her perspective piece in the JNCI issue entitled “Building the Evidence Base for Integrative Approaches to Care of Cancer Survivors.” In an introductory article, Jun J. Mao and Lorenzo Cohen of the Department of Family Medicine and Community Health, Abramson Cancer Center, Perelman School of Medicine, University of Pennsylvania and the University of Texas M.D. Anderson Cancer Center, respectively, line up this monograph thusly:
Cancer survivors, millions in number, often struggle to manage the physical as well as emotional, social, and spiritual consequences of their cancer and its necessary conventional treatments (1). Many individuals, like Josh Mailman (2), choose to incorporate complementary and integrative medicine therapies such as meditation, acupuncture, yoga, and diet into their cancer treatment with the goal of gaining a sense of control and being more active participants in their care. By doing so, they seek to improve their outcomes, including reducing the side effects of conventional cancer treatments and improving their quality of life and survival. More than ever before, cancer survivors desire the evidence-based integration of complementary and integrative medicine into conventional cancer care not only to treat their cancer but also to help in the healing of mind, body, and spirit.
Yes, it’s true. Thanks to the efficacy of real medicine, real oncology, there are now millions of people alive today who have survived cancer. This is a wonderful thing, unprecedented in medicine. It is also true that there are survivorship issues, both physical and psychological, that need to be tended to. These include a myriad of issues, including lasting sequelae of cancer and the treatments that eradicated it that impact quality of life, as well as psychological issues.
As is usual in such propaganda, the argument is made that patients are crying out for the “integration” of CAM into conventional care. This is, as many of us have pointed out over the years on SBM, at best an exaggeration that results from the co-opting of conventional, science-based interventions, such as diet and lifestyle changes, exercise, and pharmacognosy, as being somehow “alternative,” “complementary,” or “holistic” when they are nothing of the sort. Whether most CAM advocates realize it or not (and I doubt the authors of the articles making up this monograph and most prominent quackademics realize it), this co-optation serves the purpose of providing a sheen of respectability to the—shall we say?—less reputable, more pseudoscientific modalities that are routinely lumped in with CAM, such as reiki and other forms of “energy healing,” acupuncture and other traditional Chinese medicine, and naturopathy—even homeopathy. In any case, if you look at how prevalent the use of CAM is the numbers for hard-core alternative medicine, such as homeopathy, acupuncture, reiki, and the like remain very low (single digit percentages); the illusion of popularity is produced by lumping in supplements (pharmacognosy), diet and lifestyle interventions, and a vague “spirituality” into the mix. CAM/”integrative medicine” is not a scientific or medical construct, it’s an ideological construct, a marketing tool.
It is a brand, not a specialty, and it’s a brand that, as Mao and Cohen put it, they want to see “incorporated within the standard of care worldwide.”
Promoting the brand
Thumbing through this issue of JNCI (metaphorically speaking, obviously; I read it online), I was struck at just how much the monograph within was constructed to promote the concept of “integrative oncology” rather than to critically examine the concepts at the heart of integrative oncology, all gussied up in descriptions of “building the evidence base” (as Dr. Briggs put it). I suppose this is not the least bit surprising, but it is disappointing that the JNCI would devote a whole monograph to such an endeavor. Even more disappointing (but, again, not surprising) is the revelation of just how much the National Cancer Institute (NCI) supports CAM studies, as described in an article by Jeffrey D. White, MD, Office of Cancer Complementary and Alternative Medicine, NCI, entitled “National Cancer Institute’s Support of Research to Further Integrative Oncology Practice“. (Note the acronym, OCCAM, which, as I like to point out, is perhaps the world’s most inappropriate acronym for a government agency.) The amount of research support for CAM in oncology (or “integrative oncology”) through the OCCAM is laid out:
Both the absolute and proportional sizes of the National Cancer Institute’s (NCI’s) CAM research portfolio grew substantially in the early 2000s reaching a peak in FY2004 ($128.7 million; 2.7% of NCI’s appropriations). Over the intervening decade, NCI has annually supported over 300 intramural and extramural projects with some component of CAM research, with research costs totaling 80–120 million dollars annually (1). The great majority of these projects explore aspects of basic science or clinical cancer research; however, NCI also supports research to improve communication about CAM issues (2). The NCI’s Physician’s Data Query program also provides summaries of the literature about several CAM interventions with separate formats developed for healthcare practitioners and for patients (3).
I note that this is roughly the same size as NCCAM’s annual budget, with year-to-year fluctuations. Indeed, in 2004, OCCAM received more funding that NCCAM. Overall, if you add up all the CAM expenditures from all the institutes that make up the National Institutes of Health (NIH) in FY2013, you’ll find that it was nearly a half a billion dollars spent on the “integration” of pseudoscience with medicine by our federal government, half of that being administered by NCCAM and OCCAM. In any case, White’s article is, inadvertently no doubt, a perfect example of how a perfectly respectable specialty like natural products pharmacology (pharmacognosy) has been co-opted as somehow “alternative” or “complementary”:
NCI is the only institute at the National Institutes of Health with an office tasked with facilitating the growth of a CAM research portfolio and disseminating information on the topic. The Office of Cancer Complementary and Alternative Medicine (OCCAM), housed in the Division of Cancer Treatment and Diagnosis, works with various other components within NCI to accomplish these objectives. Among OCCAM’s activities is work done with laboratories in NCI’s Center for Cancer Research and the Natural Products Branch to establish collaborations with several international centers to screen novel natural products for anticancer activity and to train visiting postdoctoral fellows. This work is motivated by the recognition that traditional medical systems have been sources for identifying effective cancer therapeutics such as arsenic trioxide (5). OCCAM has also established unique opportunities for collaboration and dialog such as conferences about TCM and cancer and meetings to foster dialog and collaboration between CAM practitioners and cancer researchers.
Let’s just put it this way. Traditional Chinese medicine is a construct that was retconned by Mao’s regime to turn Chinese folk medicine that no educated Chinese wanted (because it was, by and large, quackery) into the “traditional Chinese medicine” to which academic medical centers such as M.D. Anderson and Memorial Sloan-Kettering Cancer Centers, not to mention the Cleveland Clinic, among others, devote considerable resources. It’s amazing how much things have changed in 30 years with respect to the government’s position on quackery.
Particularly troubling is how OCCAM is promoting “integrative oncology” beyond academic medical centers:
One major component of NCI’s clinical research activities is the work that takes place in the NCI Community Oncology Research Program (NCORP), formerly known as the Community Clinical Oncology Program. Approximately 30% of the clinical trials performed in this multicenter system for cancer prevention and symptom management studies are testing a CAM product (eg, ginger for chemotherapy induced nausea and vomiting) or other intervention (eg, acupuncture for cancer-associated fatigue) (4).
Let me repeat that: Nearly one-third of NCI-sponsored clinical trials through the NCORP are for “integrative oncology.” Comparing the evidence base for integrative oncology to conventional oncology, it boggles the mind that such a huge chunk of an important resource for testing is diverted in this way. Meanwhile, the NCI still administers its “best case” series, in which alternative medical practitioners present what they consider to be their most convincing single cases or case series to the NCI in order to try to entice the NCI into showing interest. It is this misguided program that led to the NCI working with Stanislaw Burzynski in the 1990s and Nicholas Gonzalez in the late 1990s and early 2000s, as well as to support high dose intravenous vitamin C treatment for cancer. OCCAM indeed.
It’s not just the government, of course. After all, the Society for Integrative Oncology is very much into promoting integrative oncology as well, as befits its name, as described in an article in the monograph by Susan Bauer-Wu, Suzanna Zick, Richard T. Lee, Lynda G. Balneaves and Heather Greenlee entitled “Advancing the Evidence Base and Transforming Cancer Care Through Interprofessional Collegiality: The Society for Integrative Oncology“:
As an interdisciplinary and interprofessional society, SIO is uniquely poised to lead the “bench to bedside” efforts in integrative cancer care. SIO members are comprised of a variety of professionals including, but not limited to, conventional cancer clinicians (ie, medical oncologists, radiation oncologists, and oncology nurses), family medicine providers, naturopathic doctors, traditional Chinese medicine practitioners, mind–body therapists, nutritionists, patient advocates, and basic scientists. This diverse membership facilitates true clinical integration of complementary modalities because such change requires breadth of expertise and different perspectives, to listen and learn from one another while challenging each other’s assumptions and existing paradigms.
OK, hold it right there. Any medical society that allows naturopaths to be members and touts “integrating” their “expertise” into medicine has automatically lost any claim to scientific legitimacy, given that naturopathy consists of a veritable cornucopia of pretty much every quackery known to humankind, including homeopathy (which is required study for naturopathy students and the knowledge of which is tested in the NPLEX, the naturopathic certification examination). Just peruse Scott Gavura’s Naturopathy vs. Science series, or any of a number of posts by myself or other SBM bloggers if you think I exaggerate. In particular, pay attention to what naturopaths say when they think no one’s listening. Ditto traditional Chinese medicine practitioners, as has been explained many times here before. This is the essence of quackademic medicine, elevating practitioners of pseudoscientific medicine, medicine based on prescientific concepts of how the body works and diseases develop, and outright quackery to be equals with practitioners of science-based medicine.
But it’s not just the SIO, unfortunately. In a commentary by Kevin D. Stein, Ted Gansler, Colleen Doyle, Rebecca Cowens-Alvarado, Virginia Krawiec, Carter Steger and Elvan C. Daniels entitled “Integrative Oncology and Wellness Considerations in Cancer Survivorship” the American Cancer Society has also weighed in. Yes, this is the same American Cancer Society that used to maintain a series on unproven methods in cancer treatment dedicated to examining cancer quackery—sadly abandoned over 20 years ago with the rise of CAM—but is now weighing in on “integrative oncology” and touting its research there. What the ACS writes is another perfect example of how “integrative oncology” has co-opted what should be science-based treatments, such as treatments involving exercise, nutrition, and life style modification:
The Society’s Nutrition and Physical Activity Guidelines for Cancer Survivors (2) are the foundation of communication, programmatic, and advocacy efforts designed to support survivors in their ability to make healthy lifestyle choices. Resources such as the What to Eat During Cancer Treatment cookbook, The Complete Guide to Nutrition For Cancer Survivors, and the online I Can Cope—Nutrition During Treatment help survivors manage nutrition-related side effects of treatment and maintain good nutritional status. The Society’s collaboration with the American College of Sports Medicine to create the Cancer Exercise Trainer certification helps survivors identify qualified exercise professionals to assist with setting and achieving physical activity goals, and our collaboration with the LiveSTRONG at the Y program provides local expertize to support survivors in being physically active.
No one would argue with these goals. There is nothing “alternative” or “integrative” about them. Now comes the quackery:
The ACS Extramural Grants department funds innovative research to advance the field of palliative care and symptom management, including integrative oncology. In addition to investigator-initiated mechanisms, the Society is also developing Requests For Applications to address how nutrition and physical activity influence survivors’ treatment, symptoms, weight, and QOL. Through Health Professional Training Grants, the Society funds clinicians and clinician-researchers working in the area of integrative oncology and has funded health professionals studying Reiki, mindfulness, acupuncture to treat hot flashes, and other integrative methods.
Reiki is, as I’ve discussed more times than I can remember, faith healing that substitutes Eastern mysticism for Christianity as its core belief system, and acupuncture is nothing more than a theatrical placebo, as has been discussed on this blog more times than I care to catalogue. Yet reiki, which does not belong in a medical center, except perhaps if one allows reiki masters into hospitals in the same way priests and ministers are allowed into hospitals (i.e., as chaplains there to comfort patients, with no claim of being able to treat anything), is now found in academic medical centers, such as the Cleveland Clinic, the University of Arizona, and many other academic medical centers, and the ACS is funding studies of it.
How far the ACS has fallen, allowing its admirable initiatives in promoting better care of cancer survivors to be co-opted by quackery. Unfortunately, it is a conscious strategy on the part of integrative oncology advocates to promote the use of CAM to treat cancer survivors, as described in an article by Julia H. Rowland and Ann O’Mara entitled “Survivorship Care Planning: Unique Opportunity to Champion Integrative Oncology?” What choice do CAM advocates have, given that CAM has not been shown to increase survival, but to shoehorn it into oncology as “integrative oncology” by emphasizing using placebo medicine to ease symptoms in survivors. None of this stops Rowland and O’Mara from trying to imply that CAM can increase survival in cancer patients:
Within the spectrum of treating the lingering and late effects of cancer, some promising interventions are emerging. For example, ginseng and yoga have shown promise in symptom management trials of fatigue and sleep disturbances respectively, both chronic problems reported frequently by cancer survivors (5,6). Given the documented positive association between quality of life and survival, there is arguably an important role for CAM use in recovery and life after cancer.
After co-opting pharmacognosy and exercise as somehow “alternative,” the next frontier for “integrative oncology” is to imply that it can somehow improve survival.
Bringing it all together
There were too many articles to cover them all in this post. In particular, there were a couple of clinical trials that demonstrate quite aptly the problems with integrative oncology as a concept. Perhaps, if nothing else grabs my attention before then, I will take a look at them next week, or perhaps I will discuss them on my not-so-super-secret other blog. What I wanted to finish with is what was clearly intended as the centerpiece of this monograph, a set of clinical guidelines by Heather Greenlee, Lynda G. Balneaves, Linda E. Carlson, Misha Cohen, Gary Deng, Dawn Hershman, Matthew Mumber, Jane Perlmutter, Dugald Seely, Ananda Sen, Suzanna M. Zick, Debu Tripathy, for the Society for Integrative Oncology Guidelines Working Group entitled “ Clinical Practice Guidelines on the Use of Integrative Therapies as Supportive Care in Patients Treated for Breast Cancer“. This is, after all, where the “rubber hits the road,” so to speak, in which the SIO ranks integrative oncology interventions based on what its guidelines working group considers to be the best existing evidence. The results, it turns out, are not surprising to someone rooted in science-based medicine. I’ll show you what I mean.
First of all, let’s look at how the guidelines were developed. First, SIO started with a working group, an expert panel, if you will, made up of members possessing expertise in medical oncology, radiation oncology, nursing, psychology, naturopathic medicine, traditional Chinese medicine, acupuncture, epidemiology, biostatistics, and patient advocacy. One wonders where the homeopaths and reiki masters were, although certainly naturopathy encompasses at least homeopathy, given how integral homeopathy is to naturopathy. In particular, one wonders why there doesn’t appear to be a chiropractor on the panel, given the popularity of chiropractic, which is at least as “respectable” as naturopathy or traditional Chinese medicine and has the added advantage that some musculoskeletal manipulation might actually provide some relief for low back pain. (Read Sam Homola’s excellent posts to learn what chiropractic, stripped of its vitalism, might be able to accomplish when strictly limited to musculoskeletal pain such as low back pain.) As I like to say, chiropractors are undertrained physical therapists with delusions of grandeur, but they are popular, and there’s no reason I can see for the SIO to leave them off the panel, at least not compared with TCM practitioners and naturopaths, as they did actually do a search for chiropractic, as shown in the supplemental data. (Spoiler alert: None of the chiropractic modalities were found to have sufficient evidence to make a recommendation.)
It is, however, telling to look at the list of excluded modalities:
Several interventions were excluded for the following reasons. Some have already been well summarized by other groups [eg, diet (22,23), physical activity (22–24)], while others already have a large evidence-base and are often no longer included in the definition of integrative or complementary interventions as they have become mainstream [eg, cognitive-behavioral therapy (25), psychoeducation (26), counseling (27), and support groups (26)]. Others were in early or pilot stages of research (eg, attention restoration therapy) or were not considered integrative interventions for the purposes of these guidelines (eg, prayer, spirituality).
Of course, once again I must emphasize that diet and physical activity were never “alternative” or “integrative,” nor was cognitive-behavioral therapy, counseling, or support groups, although all of these were oversold as improving cancer survival, as our occasional guest blogger James Coyne has described. As for the rest, prayer and spirituality are religion, not science. Overall, this list of excluded therapies is perfect as an illustration of the arbitrariness and falseness and of the very concept of “integrative medicine,” as is the manner in which the SIO defined these therapies itself:
Complementary and alternative therapies are generally defined as any medical system, practice, or product that is not part of conventional medical care (13,14). Examples include natural products (ie, vitamins, minerals, botanicals, and fish oil) and mind–body practices (ie, yoga, meditation, acupuncture, and massage). Complementary medicine is the use of a therapy in conjunction with conventional medicine (14). Alternative medicine is the use of a therapy in place of conventional medicine. Integrative medicine is the use of evidence-based complementary practices in coordination with evidence-based conventional care. Integrative oncology refers to the use of complementary and integrative therapies in collaboration with conventional oncology care.
Again, natural products are part of conventional medical care. For instance, digoxin is derived from the foxglove plant, although, as I like to say, there is a reason we don’t recommend that patients with heart failure or arrhythmias chew foxglove leaves to treat their heart condition. In terms of oncology, Taxol is derived from a substance in the bark of the Pacific Yew, and many chemotherapy agents were derived from natural products or the modification of natural products. The difference between using the “integrative oncology” version of natural products and the SBM version of natural products is that the “integrative” versions are crude, impure, and vary in activity from lot to lot.
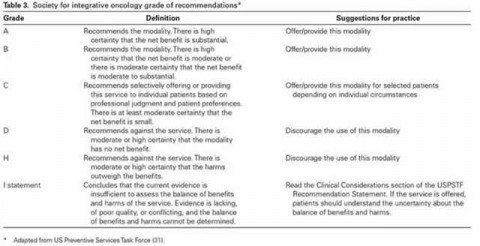
Arbitrary and artificial definitions aside, the panel did an extensive literature search of nine databases (EMBASE, MEDLINE, PubMed, CINAHL, PsychINFO, Web of Science, SCOPUS, AMED, and Acutrial) from January 1, 1990 to December 31, 2013 and identified 4,900 articles, of which 203 were eligible for analysis because they were randomized controlled clinical trials of CAM interventions in breast cancer that met the inclusion criteria. It then ranked the interventions using the Jadad scoring scale and a modified scale adapted from the Delphi scoring scale to result in a score from A to I defined as follows (click to embiggen):
So what did the SIO find? Let’s put it this way. The results were most definitely…underwhelming. For example, the only grade A recommendations were for meditation, yoga, and relaxation with imagery for routine use for common conditions, including anxiety and mood disorders (Grade A). Notice that there are no grade A recommendations for anything having to do with pain, but only for symptoms with an even heavier subjective component, namely anxiety and mood. Of course, yoga is a form of exercise and therefore nothing out of the realm of conventional medicine, given the number of studies that have shown the benefits of exercise in cancer patients. Similarly, the only grade B recommendations included stress management, yoga, massage, music therapy, energy conservation, and meditation for stress reduction, anxiety, depression, fatigue, and quality of life. Interestingly, again, none of these, with the possible exception of meditation, can be considered in any way “alternative,” thus once again demonstrating how integrative oncology specifically and integrative medicine in general have co-opted treatments that should be considered conventional as somehow “alternative”. As for music therapy, massage, and the like, these represent modalities that I like to point to as examples of what we used to call supportive care that have been “medicalized” by CAM and turned into therapies when in reality they’re just activities and modalities that help patients feel a bit better or help pass the time, no specific effects intended. As for massage, it is rather disappointing that SIO lumped it together with “healing touch,” given that healing touch is a form of energy healing very much like reiki and thus total quackery, whereas massage at least has the benefit of feeling good to most patients.
As for the rest, surprisingly (given that this is an SIO document) but not surprisingly to anyone rooted in SBM, acupuncture does not appear as a modality in grade A or B, meaning that, at best, the SIO considers acupuncture for anything to be only worth recommending “selectively offering or providing this service to individual patients based on professional judgment and patient preferences” and deems that there “is at least moderate certainty that the net benefit is small.” Electroacupuncture (which is in reality TENS rebranded as acupuncture) and acupressure are given a grade B recommendation for nausea and vomiting, but that’s about the best, and as I’ve discussed before that evidence is a bit shaky.
The key observation was that the “majority of intervention/modality combinations (n = 138) did not have sufficient evidence to form specific recommendations (Grade I).” (Grade I means insufficient evidence.) I note that the supplemental document shows that homeopathy is one of those modalities, even though there is more than enough evidence on basic science considerations alone coupled with clinical trials that show no benefit above placebo to state that it is ineffective for basically everything. Ditto reflexology, which gets a grade I recommendation for most things, but a grade C recommendation for “improving quality of life among BC [breast cancer] patients.” Meanwhile healing touch is given a grade C recommendation for “improving mood in BC patients undergoing chemotherapy.” Once again, healing touch is energy medicine quackery, much like reiki. In other words, little, if anything, in these clinical guidelines gives support for real “alternative” treatments, although they do give mild support for a few potentially science-based modalities rebranded as CAM/”integrative oncology.”
Amusingly, however, these new guidelines are much weaker in their recommendations than a previous set of SIO guidelines discussed by Kimball Atwood six years ago. Particularly notable is how far down the ladder of recommendation strength acupuncture has fallen since then, and the SIO, at least for breast cancer survivors, no longer recommends considering consulting a “qualified expert in CAM modality, such as an Doctor of Naturopathy (ND) who is board certified in naturopathic oncology ” when conventional therapies fail, but I’m actually not sure the SIO did this, because these guidelines are for cancer survivors. Either way, it would seem as though the more studies are examined and performed, the weaker SIO’s recommendations become, which is not surprising given that most “integrative” oncology modalities are placebo.
Of course, the real reason for this monograph is not so much a critical analysis of integrative oncology, although some of the authors do appear to try to do this. The real purpose is to use an ostensibly critical analysis buying into the false dichotomy of “integrative oncology” in order to rebrand potentially science-based modalities as “alternative” or “integrative” and to provide ammunition for advocates of “integrative oncology” to start “integrating” quackery with science-based medicine. As Benjamin Kligler and Margaret Chesney state in their article in the monograph entitled “Academic Health Centers and the Growth of Integrative Medicine“, referring to the Consortium of Academic Health Centers for Integrative Medicine (which we’ve discussed before many times, for example, here and here):
Many barriers—including reimbursement challenges—still exist in the effort to make integrative approaches available as part of routine care. With the publication of this monograph though, we take an important step in removing one of the barriers to integration: the availability of high-quality research evidence on the appropriate role of integrative medicine in cancer care. We are proud to be part of this effort and look forward to the many ways in which the Consortium can provide support and momentum for researchers and clinicians in oncology as we move forward.
Except that this monograph doesn’t really do anything of the sort. If anything, it confuses matters. Unfortunately, integrative oncologists have been far too successful in promoting this false dichotomy listed in the same article unironically:
The Consortium of Academic Health Centers for Integrative Medicine—an organization comprised of 57 academic health centers and health systems in North America—defines integrative medicine as follows:
Integrative Medicine is the practice of medicine that reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic approaches, healthcare professionals and disciplines to achieve optimal health and healing.
As this definition implies, although an openness to using therapies such as acupuncture or massage is a component of the integrative approach, integrative medicine goes far beyond simply combining the therapies previously described as “complementary/alternative medicine” with conventional care. It describes a change in philosophy, which expands our role beyond that of treating disease to reaffirm the commitment to treating the whole person. Almost more than anywhere else in medicine, the practice of oncology and the work of caring for a patient with cancer and their family clearly call for this approach and for a commitment to whole-person care. Lifestyle counseling, behavioral medicine interventions, and spiritual support all play critical roles in this integrative approach, alongside the use of other therapeutic strategies rooted in a rigorous evidence-based approach to the best conventional care. This is integrative medicine for cancer.
No, it is a false dichotomy. It is not necessary to “integrate” quackery like healing touch, naturopathy, or acupuncture with science-based conventional medicine in order to “reaffirm the commitment to treating the whole person” or expand a practitioner’s role “beyond that of treating disease.” A favorite saying of mine might be a bit of a cliché, but that’s OK. It’s a cliché that’s true. There is no such thing as “alternative,” “complementary,” or “integrative” medicine, nor should there be. Such medicine that is shown to be safe and effective scientifically ceases to be “alternative,” “complementary,” or “integrative” and becomes just medicine, and that is how it should be. Treatments that are truly effective and safe do not need the training wheels of a title like “alternative,” “complementary,” or “integrative.” They will stand on their own to scientific testing, no special protection required, and they shouldn’t be used until they have. Remember, as well meaning and sincere as its practitioners and champions are, “integrative oncology” is a Trojan horse that is depositing quackery right into the heart of academic medicine.