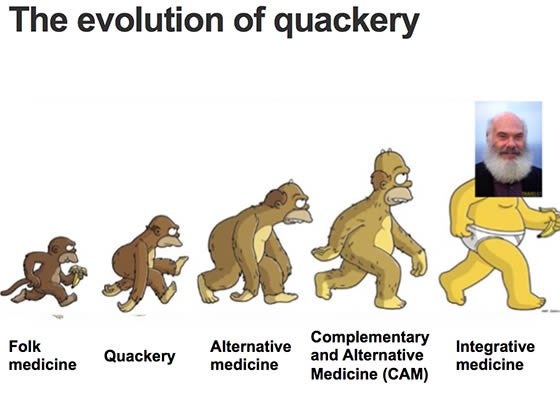
(Editor’s note: I was away at Skepticon over the weekend, where I gave a talk entitled “The Central Dogma of Alternative Medicine”. (When the talk’s up on YouTube, I’ll provide a link, of course.) Because of all the fun and travel delays I didn’t get a chance to turn my slides and notes into a blog post yet. Also, I’m on vacation this week. However, this gives me the opportunity to resurrect a blog post from 2007 on my not-so-super-secret other blog, because I think the concept is interesting. I even use it in a slide that shows up in many of my talks (above). I’ve updated dead links and added some text to include relevant links to posts written since. Enjoy, and I’ll definitely be back next week with original material, if not sooner, given that there are others here who might have the temerity to take part or all of this week off.)
I wish I had thought of this one, but I didn’t. However, I never let a little thing like not having thought of an idea first to stop me from discussing it (even if Steve Novella’s also discussed it), and this particular idea is definitely worth expanding upon because (1) it’s interesting and (2) it combines two of my interests, alternative medicine and evolution. I agree with parts of the idea, but it’s not without its shortcomings. Indeed, I’d very much welcome any of the evolutionary biologists who read this blog to chime in with their own ideas.
A colleague of mine, Martin Rundkvist over at Aardvarchaeology, has proposed a rather fascinating idea regarding the evolution of alternative medicine in which he argues that alternative medicine evolves according to certain selective pressures. As you may or may not know, evolution is not just for biology, but has been proposed as a mechanism in cultural memes, for example. Since alternative medicine is a cultural phenomenon, it is not unreasonable to look at such non-evidence-based medicine and hypothesize what might be the selective pressures that shape its popularity and evolution. After all, if we’re going to discourage the use of non-evidence-based medicine or even quackery, it’s helpful to understand it. We already know that alt-med terminology has evolved considerably into the current preferred term, “integrative medicine.” (See also the image above and my blog posts on this evolution here and here.)
Martin primarily considers what the selective pressures are on various alternative medicine modalities and comes to a startling conclusion: Namely, that the selective pressure on such modalities is primarily to select for ineffective treatments. He bases this on two primary forms of negative selection. First, he hypothesizes, there will be selective pressure against modalities that cause obvious harm. According to this concept, such modalities will tend to be eventually recognized as harmful and shied away from by alternative medical practitioners due to fear of lawsuits and government regulations. The second form of selective pressure will come from conventional medicine. In essence, alternative medical therapies that can be shown to have a reasonable degree of efficacy will risk being co-opted by us “conventional” practitioners of evidence-based medicine and thus taken out of the armamentarium of alternative practitioners, whose setting themselves apart from mainstream medicine is very important to their livelihood. This leads Martin to observe that homeopathy is the ultimate CAM therapy:
So, there is evolutionary pressure on alternative therapies to achieve near-zero effect. This is why homeopathy is still around: its main method being the administration to patients of small amounts of clean water, it’s uniquely suited to surviving indefinitely in the alternative-therapy biotope. Homeopathic remedies can neither harm nor benefit patients.
This is a fascinating and lucid insight. Clearly it has some merit. However, it is incomplete. The reason, I would argue, is that the negative selective pressures Martin identified are almost certainly not as potent as he thinks they are, as evidenced by how rare it is for an alternative medical therapy to actually go “extinct.” Indeed, I would argue that selection against harmful or potentially harmful remedies is actually fairly weak and perhaps even nonexistent. After all, black salve is still around after many decades, if not hundreds of years, and it can produce some truly horrifying complications (not for the squeamish). Even though the FDA banned importation of black salve products and they can be demonstrably harmful, they are still around and show no sign of disappearing. Another example is Laetrile. Multiple well-designed clinical trials demonstrated that Laetrile is ineffective against cancer, and it has the well-known potential complication of cyanide toxicity. It, too, shows no signs of disappearing. Of course, perhaps the most popular ineffective CAM therapy that has potentially deadly complications is chelation therapy, which remains widely used among CAM practitioners to treat cardiovascular disease and autism, despite of the extreme biological implausibility of the argument that it should work for either condition and despite there being no good evidence that it does. Indeed, back in 2006 there was even a well-publicized case of an autistic boy who died as a result of chelation-induced hypocalcemia causing a fatal cardiac arrhythmia.
No, there are lots of potentially-harmful CAM modalities out there that show no signs of going away.
Let’s look at the flip side of the negative selection, co-optation of “effective” alternative therapies into mainstream medicine. Once again, this is probably a weaker negative selective force than it might seem. Herbal medicines, for example, are probably the most common of the CAM-type modalities to show some evidence of efficacy in randomized clinical trials. This is mainly because they are drugs. Impure and dirty drugs with widely-varying levels of active ingredient from lot to lot, but drugs nonetheless. The problem for the co-optation of these drugs by conventional medicine is that practitioners of scientific medicine do not like unpredictability in their drugs. They like drugs with a predictable effect; herbal medicines “in the raw,” so to speak, do not fit the bill, particularly when pure pharmaceutical alternatives that lack the contamination and unpredictability of herbs exist. Even if conventional medicine co-opts an herb, for example, it is usually in the form of the active ingredient purified from that herb. For example, if you have breast cancer, you could try to chew on the bark of the Pacific Yew tree for its anticancer properties, but you’d be a whole lot more likely to do better if you took pure Taxol derived from that bark – and took it intravenously. The example of Taxol also suggests that once conventional medicine co-opts an herbal or plant-based remedy, it usually does not supplant the original alternative therapy. After all, all of the “natural goodness” has been extracted from it during the purification of the active ingredient! CAM mavens would often rather take the raw herb or the herb chopped up and compressed into an herbal pill because it’s more “natural.”
As for other non-herbal CAM therapies, even when they’re co-opted by modern medicine (although it’s often arguable whether conventional medicine or CAM did the co-opting), often an “alternative” version remains. The scientific version will be stripped of all the woo, while the “alternative” version will retain it. Think massage therapy and perhaps even chiropractic, which, as I’ve said before, stripped of its woo is nothing more than physical therapy with delusions of grandeur in the form of claims of being able to cure all manner of illnesses that have nothing to do with the spine or the musculoskeletal system.
Finally, there is one last aspect of Martin’s concept that argues against it. Martin states:
Evidence-based medicine, alternative medicine and weaponry change through time because of selection pressure. This means that they evolve and produce a fossil record of discontinued methods and therapies.
Here’s the problem: There actually is no “fossil record” of discontinued CAM methods and therapies. The reason is simple: CAM does not abandon its methods, regardless of evidence and, to a large degree, regardless of harm. Yes, individual treatment modalities may wax and wane in popularity, but they never go away completely. They never go extinct. Think about it a bit. Can you think of a single “alternative medicine” treatment modality that’s ever been completely abandoned because it either doesn’t work, is too harmful, or has been co-opted by conventional medicine? I can’t. CAM is, in the words of James Randi, an “unsinkable rubber duck.” It just won’t disappear. Martin is quite correct that homeopathy, for example, has persisted for 200 years despite no evidence for its efficacy. Aryuvedic medicine has persisted at least a couple of millennia, despite a similar lack of evidence. Ditto most of traditional Chinese medicine, whose real history has been conveniently retconned over the last several decades, making it more popular even outside of China than it’s ever been. Never mind that these systems were developed in a time when very little was known about how the body actually works and are infused with spiritual and religious beliefs. They are still used by many millions, if not billions, of people worldwide. They have left no “fossils.” Of course, as in evolution in biology, this selection, applied over long periods of time, may ultimately eliminate such modalities, but if I were somehow able to call the Doctor to give me a ride in his TARDIS a couple of hundred years in the future, I bet that virtually all of these CAM modalities would still be in use. Part of the reason, I suspect, is that, as Martin pointed out, most CAM modalities do little; there is usually no CAM modality that can supplant existing modalities.
In any discussion of the evolution of CAM, I would be remiss not to look at its primary competition for resources (i.e., patients) in the ecosystem of medicine, namely scientific, evidence-based medicine. EBM has been hugely successful in many areas. Indeed, it can be said to have driven back CAM to a much smaller “ecological” niche than it once occupied. These days, relatively few people rely on CAM modalities when faced with a truly life-threatening illness, such as cancer. The Katie Werneckes, Abraham Cherrixes, and the Chad Jessops of the world (if the latter even had cancer), who treat life threatening cancers with high dose vitamin C, the Hoxsey concoction, or nasty, burning goo like the infamous “black salve,” respectively, are pretty uncommon. The main ecological niches for CAM these days have contracted to two areas. First are “diseases of living.” In other words, CAM has been for the most part relegated to the treatment of what are generally vague complaints that are not exactly diseases or to self-limited conditions. Indeed, one could argue that the strongest positive selective pressure for CAM modalities is how well each one gives the appearance of doing something therapeutic for such conditions, whether it actually does anything or not. In other words, how good of a placebo is it? Or is its timing or method of administration optimally adapted to correlate with the patient’s improvement anyway, allowing the confusion of correlation with causation? The better the adaptation, the more likely a CAM modality will thrive and expand.
The other remaining ecological niche for CAM, I would argue, is in serious diseases for which conventional medicine does not have much to offer. These conditions include diseases such as terminal cancers that have passed beyond our ability to treat them, as well as any manner of chronic diseases for which conventional medicine does not have a cure, such as Parkinson’s disease, chronic pain syndromes, multiple sclerosis, etc. Conventional medicine can treat and often palliate such conditions, but it cannot cure them. In this latter niche, I would argue that the primary positive selective pressure would be how well the CAM modality can inspire belief in its practitioners and hope in its users. The two are related, of course; the more the practitioner believes in the modality the more he or she can sell the patient on it.
Of course, applying evolutionary principles to CAM only goes so far. It’s a highly complex situation, and there are a number of positive and negative selection pressures that one could postulate. Certainly, the marketplace and how much of a feel-good aspect there is to CAM therapies are important. Finally, no doubt, like evolution, there are aspects to CAM proliferation that do not depend upon selection, a CAM equivalent of genetic drift, for example. Indeed, there was a fascinating paper five years ago about why quackery persists which argues for a similar hypothesis of selection for more ineffective therapies but also added a twist: That even in self-medicating or use of alternative medicine effective remedies can be lost due to stochasticity, in other words, due to random chance. Indeed, the authors point out that most highly efficacious innovations would be predicted to be lost due to stochasticity. Indeed, my reading of this study would suggest that one reason why highly effective treatments actually do persist in our society is because scientists, physicians, and science-based medicine validate what treatments are efficacious, retaining the treatments that are and trying (but not always succeeding) to discard the ones that aren’t. For people self-medicating, such a mechanism is not operative.
Since were using evolutionary principles now, one might also look at CAM this way with respect to its “competitors.” Perhaps CAM is adopting an evolutionary strategy not unlike that of dogs or cats. In other words, it was subsuming itself to its more successful competitor, conventional medicine, in much the same way that ancient wolves were domesticated by humans and ultimately started to speciate into dogs. The problem with that analogy, of course, is that both human and dog gain benefits from their relationship. Humans gain companionship and work from dogs; dogs gain protection and a reliable source of food and shelter. It could be argued which species gains more, human or dog (probably humans early on and dogs now), but there is little doubt that both species benefit. So, in the relationship between CAM and conventional, who benefits?
The answer is obvious: CAM. Scientific medicine does not need CAM, but these days CAM appears to need scientific medicine. Indeed, the very name CAM was adopted to allow alternative medicine to seem more palatable to practitioners of conventional medicine and ease its ability to insinuate itself into academic medicine, which, as I’ve documented extensively, it is having increasing success in doing so, even to the point of finding its way into the curriculum of various medical schools.
What this tells me is that we’re looking at a “speciation” event in alternative medicine. There is a strain of alternative medicine that fits in with the whole movement towards CAM in medical schools, and there is a strain of alternative medicine that does not. Now here’s where Martin’s idea of selective pressures favoring placebos in alternative medicine comes in. The strain of alternative medicine that either excessively credulous or cynical academicians embrace falls under exactly the sort of selection pressure that Martin discussed that favors minimal effects. The reason is simple. The two most common justifications used for including CAM in academic medical centers are (1) the patients want it and (2) the perception among academic physicians that it won’t do any harm anyway and seems to make patients feel better. Consequently, the most common varieties of CAM in such settings are massage therapy, meditation, acupuncture, yoga, and nutrition-based therapies. Oddly enough, arguing against Martin’s idea is that seldom will you see homeopathy in academic medical centers, at least in the U.S. I speculate that that is because in such settings, there is also a negative selective pressure against extreme scientific implausibility – at least upon the initial incursion. On the other hand, perhaps it’s just an odd quirk of history, culture, or whatever that makes use of homeopathy less common in the US. After all, reiki is just as ridiculous as homeopathy, if not more so (my talk this weekend prominently featured reiki, for instance), but it’s everywhere these days in academic and community medical centers.
So what term best describes the relationship between CAM and academic medicine? Certainly CAM advocates would argue that it’s a symbiotic relationship. I would counter that it’s a parasitic relationship, and here’s why. Parasitism is defined as a relationship where one organism benefits and the other is harmed. CAM is indeed parasitic. It benefits from its association with academic scientific medicine by obtaining a level of plausibility and respectability that it could never obtain on its own, while it arguably harms academic medicine in the process. True evidence-based medicine is what academic medical centers are ostensibly built to promote, applying the scientific method to medical therapies in order to find more effective treatments. What academic medical centers should be doing is to educate the new generation of physicians in the scientific method, to better prepare them to be able to evaluate claims for treatment, whether they come from conventional medicine or elsewhere. This is how medicine has advanced so rapidly over the last 60 years. Blurring the line between science and non-science, evidence-based medicine and woo, through the enthusiastic promotion of CAM in medical school curricula, harms that endeavor, both by degrading the ability of physicians to think critically (thus preparing them to accept even more implausible treatments) and by wasting money and resources that could be better used to study more promising science-based modalities to study obviously highly-implausible gobbledygook before there’s any good evidence that it does anything at all beyond the placebo effect. It would be one thing if CAM were being studied from a truly scientific perspective. I don’t object to that; indeed, I encourage it. A true scientific examination of the vast majority of CAM will likely find it useless, while a few gems might be pulled out of the dirt. Unfortunately, though, as I’ve mentioned before, that’s not what usually happens. What almost invariably happens is that CAM is used as a marketing tool.
Although I often disagreed with him (mainly about politics) Panda Bear, MD (whose blog seems to have been hacked and has become a spam site) gets it right in describing this parasitic relationship:
Suppose I were to actually build a house. Along with a foundation it would require framing of the walls and floors, siding, wiring, glazing, plumbing and a dozen other skilled trades coordinating their efforts. The practioners of Complementary and Alternative Medicine would be like your Aunt Mildred telling you how to hang the toilet paper in the finished bathrooms and then trying to claim credit as an essential part in the construction. Complementary and alternative medicine only exists because real medicine does all of the heavy lifting leaving a risk-free enviroment [sic] in which it may ply its patent remedies. At best it’s an afterthought, something that legitimate hospitals add to their services to attract the kook money. At worst it’s a cynical ploy to fleece a little extra from the desperate, many of whom are dying and will gladly pay for another straw to grasp. In no way is it an essential part of medical therapy except that it provides entertainment to the patients and their families while medicine and nature run their courses.
He’s not quite right, at least now. These days, CAM is like Aunt Mildred claiming that the house was built by magic.
Conventional medicine fights the real battles and faces the real danger of failure, while increasingly CAM attaches itself to conventional medicine, much as the parasitic roundworm Ascaris lumbricoide finds its way into the small intestine of its host. CAM benefits from its association, but its host, conventional medicine, most definitely does not. At best it is not harmed; at worst, grave harm to scientific medicine becomes possible.
All this speculation leads me to believe that the form of CAM that increasingly thrives in academic medical centers is indeed developing into a new “species” of woo, so to speak. It’s wraps itself in scientific-sounding terminology and, for the most part, discards the more outrageously silly religious and supernatural elements that it can, all in order to become seemingly inoffensive enough that academic physicians, although they may not approve of it, remain insufficiently sufficiently alarmed by it to rise up and purge the system of this parasite. Meanwhile, the parasite grows in number and strength, continually weakening the body of academic medicine the longer it stays. Eventually, like the roundworm, it spreads its eggs where more and more academic medical centers can pick them up until the species is so entrenched and self-perpetuating that it can’t be dislodged without resulting in severe injury or death to the host.