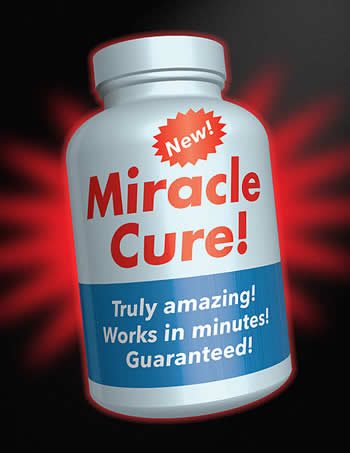
From the US Food and Drug Association article “6 Tip-offs to Rip-offs: Don’t Fall for Health Fraud Scams
“What’s the harm?” is an insidious idea when used as a justification for unscientific medical treatments. The argument is typically put forward with the assumption that direct physical harm is the only type of harm that can result from such treatments, so as long as they aren’t toxic there is no downside to trying them. Harm comes in many forms, however: delayed effective treatment, wasted time and energy, financial harm, the psychological harm of false hope, and the downstream effects of instilling unscientific beliefs regarding health care.
One other form of harm is physical but is not due to direct physical damage or toxicity. Rather, it is caused by CAM treatments interacting with proven therapies. A recent survey, presented at the Clinical Oncology Society of Australia annual scientific meeting, explored the potential for such interactions among oncology patients. Lead researcher Sally Brooks found that, in addition to vitamins and minerals, cancer patients were most interested in fish oil, turmeric, coenzyme Q10, milk thistle, green tea, ginger, lactobacillus, licorice, Astragalus and reishi mushrooms.
As I have written many times before, herbs are drugs, but many patients do not treat them as such because they are regulated and marketed as “supplements,” more like food than drugs. There are concerns that many vitamin and herbal products may interact with chemotherapy or radiation therapy in order to reduce effectiveness or even increase side effects.
The research on antioxidant supplementation, for example, raises some concerns, but is equivocal. Part of the effectiveness of chemotherapy comes from increasing reactive oxygen species (ROS) which cause damage to cells. ROS damage both cancerous and healthy cells, and so are part of the desired effects from chemotherapy, but also the side effects. It is therefore possible that antioxidants may decrease the side effects of chemotherapy, but also decrease the effects. The balance between efficacy and side effects is carefully managed in chemotherapy, and if patients are taking antioxidants (especially without telling their oncologist), this can affect that careful balance.
Systematic reviews to date have concluded that the evidence for the net effect of antioxidants in chemotherapy is mixed and of insufficient quality to come to any solid recommendations.
Other effects are also of concern. Turmeric, for example, may decrease the effectiveness of chemotherapy by interfering with the mechanisms by which chemotherapy induces cell-death in cancer cells. Turmeric also interferes with the cytochrome P450 system which is important for the metabolism of many drugs, including some chemotherapy agents, and therefore may increase side effects and toxicity.
Astragalus has effects on the immune system. While preliminary evidence suggests this may be helpful in cancer treatment, it may worsen auto-immune diseases and interact with immunosuppresive drugs.
Overall the evidence for any benefit from the commonly-taken herbal supplements as adjunctive care for any particular cancer is mixed and preliminary. At the same time these agents are drugs that can cause side effects and interact with chemotherapeutic agents, causing photosensitivity, interacting with metabolism and clearance, and perhaps reducing effectiveness. Some may actually prove useful as well, but the complexity of their effects requires careful study, which is often lacking.
Patients often do not disclose supplement use to their physicians, and therefore may not have an opportunity to receive specific advice on such use.
It is also important to recognize that studies involving carefully-standardized supplements are difficult to apply to the real world because the supplement industry is so poorly regulated. Many recent studies have found that supplements are often contaminated, have variable doses, and even contain product substitutions. It is very difficult, therefore, for patients to even know what they are getting.
While further research for each individual herbal product in specific doses for specific cancers and in combination with specific cancer treatments is required before we can make definitive statements about their safety and efficacy, there is also research into the net outcomes of those taking so-called CAM along with their cancer treatments.
What evidence we have is also preliminary, but not favorable. Some studies, for example, show that patients using CAM along with standard cancer treatments have a decreased survival. There are not randomized, and so conclusions regarding cause and effect are difficult, but such evidence does suggest caution.
Other studies find that quality of life, often touted as the main benefit for CAM, is also decreased in cancer patients using CAM.
Conclusion
Overall the evidence for the effectiveness, side effects, drug interactions, and net effects on survival and quality of life with herbs and other unconventional treatments for cancer is of poor quality, showing mixed and complex results. With herbs, since they often have active pharmacological effects, there is the potential for benefit, but also the potential for harm (as with any drug).
The claims made for such treatments often greatly exceed the evidence. Patients, therefore, are generally met with misleading information, suggesting efficacy where the evidence is thin, and downplaying the potential for harm and negative interactions. Because such treatments are promoted as “alternative” patients also are often reluctant to discuss such issues with their physicians, who may be in the best position to advise them on the potential risks and benefits.
As Brooks (the author of the recent survey) and others also point out, unconventional treatments may also present a financial burden at a time when patients are already under financial stress from their illness and perhaps reduced ability to work. They may also experience psychological stress from being pressured by well-meaning but misguided friends and family members pushing them to try unconventional treatments, at a time when they are vulnerable due to their illness.
The underlying source of all this unnecessary risk and stress for cancer and other patients is the basic notion of “complementary” or “alternative” medicine. The marketing of a subset of treatments as CAM creates an artificial double standard, one in which the rules of evidence are altered, informed consent is compromised by misinformation, product standards are lowered, and patients often do not feel comfortable discussing such treatments with their physicians.
Eliminating this double standard could be an effective first step in correcting such problems.

