What a wonderful world it would be if cancer patients could extend their survival time by mobilizing their immune systems by eating the right foods, practicing yoga, and venting their emotions in a support group. The idea that patients can enlist their immune systems to fight the progression of cancer is deeply entrenched in psychosomatic medicine and the imagination of the lay public, and evidence to the contrary has been sometimes bitterly resisted. Of course, cancer patients can use psychological techniques to relieve stress or find emotional relief in support groups and thereby improve the quality of their lives. But the prospect of being able to improve the quality of life pales in comparison to the promise of being able actually to extend life.
The hope that psychosocial intervention extends lives attracts philanthropic contributions to cancer centers and justifies research programs to determine just how psychological processes affect cancer. It is a lot easier to obtain funding if we promise to slow progression of cancer than if we merely claim to offer patients solace and support or to be study ways to reduce stress and improve emotional well-being.
No mechanism by which the mind can alter the course of cancer has been convincingly demonstrated. But the jury was still out until the late 2000s, when well-resourced, carefully designed trials — with survival as the primary endpoint — repeatedly failed to show that psychological interventions were effective. My colleagues and I asked at the 2006 European Health Psychology Conference whether we could “Bury the Idea…” that psychotherapy could extend lives of cancer patients, and this was followed by our systematic review of the available data, “The Conflict Between Hope and Evidence.” Investigators who had undertaken ambitious, well-designed trials to test the efficacy of psychosocial interventions echoed with “Letting Go of Hope” and “Time to Move on.” For some of us, to make claims in earshot of cancer patients that we could extend their lives with psychotherapy was perpetuating a cruel hoax.
Then in 2010, a study was published that claimed that a package of dietary advice and stress reduction techniques could hold off recurrence and extend the lives of women with early breast cancer. We published a detailed analysis showing the intervention was essentially inert and that the authors were “Finding What Was Not There.” However in 2012, that trial was counted as positive in a nonsystematic and highly selective review in Psycho Oncology, “Mind Matters In Cancer Survival,” which concluded:
The majority show a survival advantage for patients randomized to psychologically effective interventions for individuals with a variety of cancers, including breast, melanoma, gastrointestinal, lymphoma, and lung cancers. Importantly, for breast and other cancers, when aggressive anti-tumor treatments are less effective, supportive approaches appear to become more useful.
So,this article argued, psychological interventions are particularly indicated to extend the lives of patients with cancers that are less responsive to aggressive biomedical treatments. Yet, the review failed to cite any of the seeming unanimous contrary assessments now being reached by others, nor even some highly relevant randomized trials with null findings. The first question I had to ask was “How did this article get through peer review?” My suspicions that it had not were confirmed when I saw that the journal indicated that had been received on February 16, 2012 and accepted on February 24, 2012. I wrote to the editor:
I was quite surprised to see [the] article on psychosocial interventions and survival in Psycho Oncology with such selective and distorted attention to literature and lack of attention to criticisms of this work. To me it appears like a breakdown in peer review … Is there any explanation for it?
She replied
Professor David Spiegel submitted this paper as a non-peer reviewed editorial as the Recipient of the IPOS Sutherland Award.
This privilege is offered to all who receive the Sutherland Lifetime Achievement Award.
The process of deciding who receives the Sutherland Award goes through a committee and external peer review process.
Invited Editorials in this category are read by the 2 co-editors to ensure nothing that might infringe copyright or lead to legal proceedings is written.
While some may not agree with Professor Spiegel’s opinions this would not be a basis for dis-allowing an invited editorial. Editorials may be opinion-based.
Yet, a “peer review” of whether to invite someone to author an article is a far cry from peer review of the article itself. And nowhere did the article state that it was an invited editorial or that the normal peer review had not occurred. The was an example of the unacknowledged privileged opportunities to publish articles espousing particular positions about which I have been complaining for awhile.
I will bypass the strict deadlines and word limits set by Psycho Oncology for a Letter to the Editor and will instead provide a critique here, drawing heavily on peer-reviewed commentaries that my colleagues and I have published.
The content of “Mind Matters in Cancer Survival” in Psycho Oncology overlaps considerably with an identically entitled commentary in JAMA by the same author, and the longer Psycho Oncology article shares nine of the 10 citations of the JAMA article. I do not know whether the JAMA article was thoroughly peer reviewed, but I can attest that a number of authors who actually conducted clinical trials with survival as the outcome wrote critical responses to JAMA that were summarily rejected without comment. So much for post-publication peer review, but freedom from criticism is one benefit of privileged access publication. Articles showing up in the literature without acknowledgment that they have evaded peer review, either prepublication or post, is confusing and slows the progress of science. An article protected from criticism escapes the kinds of influences that serve to move scientific discussion forward. Science should be about reconciling ideas with embarrassing data.
The shorter JAMA article framed the issue of how mind matters in cancer survival much the same as the Psycho Oncology article, but did so in a more dramatic and disconfirmable fashion. For instance, the JAMA article more boldly cites as evidence of psychological control over disease progression that
Individuals tend to die after rather than before their birthdays and major holidays, suggesting some ability to postpone death for a short period to reach a meaningful goal.
This idea was the basis of the movie Black Swan but has been thoroughly debunked. A systematic review concluded
Research over the past three decades has failed to provide convincing evidence that psychological phenomenon such as ‘giving up’ or ‘holding on’ can influence the timing of death.
Keeping this myth alive, of dying persons controlling the time of their death, burdens cancer patients and their caregivers with unrealistic hopes that patients can, if they try hard enough, keep themselves alive for important family events. Conversely, if patients are nonetheless dying at times that are inopportune for family members, they can be accused of not trying hard enough or simply not being made of the right stuff. Even worse, the myth encourages family members to exhort dying patients to hang in there and endure excruciating pain to be alive for family events, rather than graciously accepting the end or whatever fits their personal preferences.
The JAMA “Mind Matters in Cancer Survival” also interprets in more decisive terms a recent palliative care trialwith non-small cell lung cancer patient . The trial had found that patients who given four opportunities to discuss resuscitation preferences, pain control, and the aggressiveness of treatment received less aggressive treatment, were less depressed, had higher quality of life, and lived longer with a median survival advantage of 2.25 months.
The JAMA article imposed this interpretation
This apparently counterintuitive finding suggested emotional support is not only psychologically beneficial but also medically efficacious. Moreover, the palliative care intervention also improves the quality of life by reducing depression.
Perhaps, but maybe more aggressive treatment at the end of life might not only decreases quality of life but actually shorten life. There is no indication in the original article that the investigators’ primary motive was to extend life, certainly not at the cost of other considerations. And with the intervention group receiving less aggressive treatment, the most parsimonious explanation of results is that life was shortened in the control group because of more aggressive treatment. We don’t know if the treatment received in the control group was less medically appropriate, but we certainly don’t have a basis to jumping to the conclusion that provision of emotional support to the intervention group was the key mechanism for the longer survival of the intervention group.
The Psycho Oncology article counts this trial as the eighth of a series of trials providing positive evidence for the efficacy of psychotherapy in promoting survival of cancer patients. (Whoops! When did this become a trial of psychotherapy?)
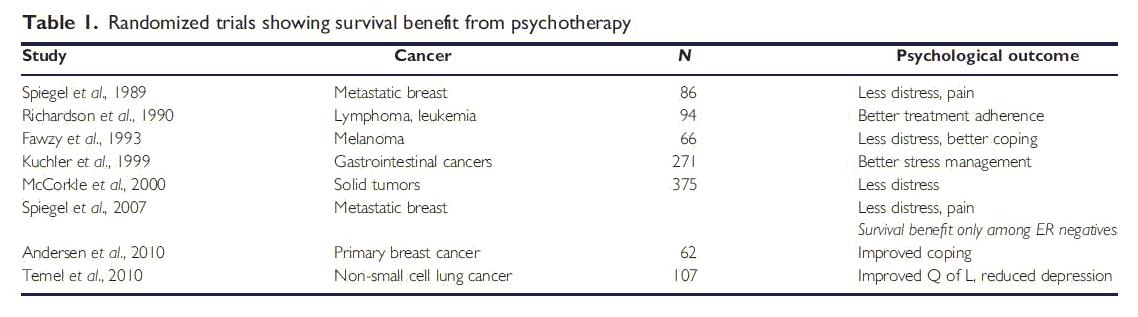
enlargeFew of the other “positive trials” listed in Table 1had survival as their primary endpoint. Most were not shown to improve survival in appropriate analyses. Among those that came even close, none were construed by their investigators as testing psychotherapy. I will review the widely misunderstood 1989 Spiegel Lancet study in a future blog post, but here I will concentrate on why the other trials the Psycho Oncology article claims to have shown “survival benefits from psychotherapy” did not do so. I will also call attention to some relevant trials that the article missed altogether, and then point to some strengths of the trials conceded in the article to be negative.
Richardson JL, Shelton DR, Krailo M, et al: The effect of compliance with treatment on survival among patients with hematologic malignancies. Journal of Clinical Oncology 8:356-364, 1990
This trial evaluated 3 different interventions training low income patients with hematologic malignancies and their caregivers in the monitoring of side effects and complications, how they could communicate better with medical personnel, and the need for them to recognize and get prompt attention for fever, bleeding, and other medical problems. One of the three interventions involved home visits and leaving poster reminders of what needed to be done. The investigators’ description of their interventions does not sound like psychotherapy. To remove any doubt, I wrote to the first author and I published her reply:
“I would agree that our study was not psychotherapy. Our study was very behavioral in concept and delivery – teaching people how to manage the disease, the treatment and the health care system. I think you can go a long way with basic patient education, family education, and health care system manipulation strategies.”
An earlier report of this trial does designate survival as a primary endpoint. With no more than 25 patients assigned to the control group or any of the three interventions, the trial would have been grossly underpowered to test effects on survival of any one of the different interventions. Post hoc survival analyses combined the three different intervention groups into one. Simple univariate analyses revealed a survival benefit for patients getting one of the interventions.
The authors state
It is also possible that the programs, by training the patients to be responsible for their own care, allowed them a sense of greater control and resulted in less fear and anxiety (p. 363).
This quotation has been cited elsewhere as the basis for counting this study as evidence that psychotherapy improves survival. Yet, the intervention did not focus on reducing fear and anxiety, and a related paper from the project reports no changes in depression across the intervention period.
The most parsimonious explanation of this trial is that after discharge from the hospital, low income and nonEnglish-speaking cancer patients benefit from education and home visits for them and their families, but it seems quite a stretch to invoke some unmeasured psychological processes as the mechanism.
Fawzy FI, Fawzy NW, Hyun CS, et al: Malignant-melanoma – effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Archives of General Psychiatry 50:681-689, 1993
This small study of stress management and health education for postsurgical malignant melanoma patients did not have survival as a primary endpoint and did not have even a provision for long term follow-up. Nonetheless, inspired by the Spiegel 1989 Lancet study, the authors undertook a post hoc examination of survival at 5-6 and 10 years post treatment and declared
When controlling for other risk factors, at 5- to 6-year follow-up, participation in the intervention lowered the risk of recurrence by more than 2 1/2 fold (RR = 2.66), and decreased the risk of death approximately 7-fold (RR = 6.89). At the 10-year follow-up, a decrease in risk of recurrence was no longer significant, and the risk of death was 3-fold lower (RR = 2.87) for those who participated in the intervention.
Largely as a result of this claim, the study received widespread attention and for a long time, little critical scrutiny. Yet, when it was entered as evidence in the Great Debate (Resolved: Psychosocial Interventions Can Improve Clinical Outcomes in Organic Disease) held at the American Psychosomatic Society in 2001, it was savaged by Arnold Relman, former editor of the New England Journal of Medicine as being
…fatally flawed because the analysis is not by the intent-to-treat method, which should be standard epidemiologic practice. The authors did not report the results on all their randomized subjects, which would have been the proper, “intent-to-treat” procedure. The number of exclusions and losses to follow-up after randomization could easily have affected the outcome critically since their groups were relatively small and they report a relatively small number of deaths or recurrences. So, I believe that any critical and experienced epidemiologist would consider that study invalid. You have to analyze by intent to treat, and there were enough cases lost to have totally changed the results and the conclusions, depending on their outcome. You simply cannot find out what happened to a lot of missing patients in this study, so you cannot have much confidence in the conclusions.
Wally Sampson, editor emeritus of science-based medicine caught some strangeness in the control group of this study. The 5-year survival of Stage I melanoma in the time after the trial was approximately 92%, yet the 5-year follow up survival for patients from the control group retained for analysis was only about 72%. Sampson calculated that the probability of a representative sample of 34 persons with Stage I melanoma having a 5-year survival rate this low is about 0.001.
Our detailed review of both the 5-6 and 10 year follow-up articles confirmed:
- Main analyses were biased by selectively excluding patients after randomization. Of the 40 patients assigned to the intervention group, one patient was excluded due to death, one due to incomplete baseline data, and a third due to the presence of Major Depressive Disorder.
- In contrast, of the 40 patients assigned to the control condition, only 28 completed baseline and 6-month assessments, but survival data were included for those in the control condition regardless of the completeness of their data.
- Fewer patients randomized to intervention and retained for analysis had died at 5-6 year follow-up than control patients (p = .03), but this difference would become non-significant with the reclassification of one patient or reversal of any of the many post hoc decisions about selectively including or excluding patients.
- The impressive claims about a sevenfold difference in survival at 5-6 years and threefold at 10 years represent an abuse of statistics. First, a simple log-rank test was not significant for differences in the distributions of survival for the two groups. Second, the authors apparently confused odds ratios with relative risks. Odds ratios are useful in observational studies, but they are likely to overestimate the benefits of offering an intervention in clinical practice when applied to results of randomized trials. Third, these odds ratios arise only in inappropriate multivariate analyses. The authors selected possible covariates from preliminary analyses that allowed inspection of almost as many covariates as the number of deaths to be explained (20) at the 5 to 6 year follow-up. Even the small pool of covariates retained for subsequent analyses violated the usual rule of having at least 10 to 15 events (in this case deaths) to be explained per covariate.
The Psycho Oncology article does not mention that in 2007 a Danish group reported results of a large, well designed controlled trial attempted to replicate the Fawzy study. Fawzy’s co-author/wife served as a consultant. No effect for survival or time to recurrence was found.
Kuchler, T., B. Bestmann, et al. (2007). “Impact of psychotherapeutic support for patients with gastrointestinal cancer undergoing surgery: 10-year survival results of a randomized trial. JCO,25(19): 2702-8.
This study was covered in my inaugural blog post and claimed that 222 minutes of psychotherapy produced a 10-year survival benefit among a mixed group of patients with gastrointestinal cancer. The Psycho Oncology article interprets this as another demonstration of the power of mind in cancer survival, but a simpler explanation is more reasonable. Namely, therapist took an active role in medical care and spent about as much time interacting with the rest of the medical team as with the patients. Compared to the control group, the intervention group received a lot more postoperative chemotherapy, radiotherapy, and time in intensive care. This difference in medical care cannot readily be dismissed.
McCorkle R, Strumpf NE, Nuamah IF, et al: A specialized home care intervention improves survival among older post-surgical cancer patients. Journal of the American Geriatrics Society 48:1707-1713, 2000
This nursing intervention for postsurgical cancer patients emphasized both physical and psychosocial support and the monitoring of physical status and an offsetting of potentially lethal complications of surgery. The article identified as the intervention’s key focus the monitoring of physical status and heading off potentially complications of surgery. A later meta analysis evaluating whether psychological interventions increased survival excluded the trial because
The result may… reflect an effect of combined optimized medical treatment and psychosocial intervention
The authors seemed intent on distinguishing their trial from a psychosocial intervention, stating
…this is the first [trial] to examine the impact of…nursing interventions on survival in cancer patients. Other studies have focused on patient’s psychosocial status, including depressive symptoms, function, and the effects of support groups.
To settle any doubt about the authors’ aims, I asked the first author directly and published her reply
We did what we did really because of the physical care. The deaths were related to major complications, sepsis, pulmonary embolus, etc. The nurses picked these things up and prevented the crisis” (R. McCorkle, personal communication, August 3, 2004).
Spiegel D, Butler LD, Giese-Davis J, et al: Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer – A randomized prospective trial. Cancer 110:1130-1138, 2007
This study attempted replication of the original Spiegel 1989 Lancet study with a somewhat larger sample of 67 women with confirm metastatic or locally recurrent breast cancer and a control group[ in which 61 women received only educational materials. The text of the Psycho Oncology article notes that the trial had no overall effect on survival, but counted it in the table as a positive finding based on post hoc subgroup analyses in which women with negative estrogen receptor status (n = 25) in the intervention group live longer when exposed to the intervention. This would not have been hypothesized. If anything, given psychoneuroimmunological speculations about psychological factors in breast cancer, an effect of psychological intervention restricted to positive estrogen receptor status women would have been predicted.
Regardless, an argument is being made on the basis of post hoc subgroup analyses involving only 25 patients. The Psycho Oncology article also fails to note that another study of supportive expressive therapy failed to replicate this finding in similar post hoc analyses.
Andersen BL, Yang HC, Farrar WB, et al: Psychologic Intervention Improves Survival for Breast Cancer Patients A Randomized Clinical Trial. Cancer 113:3450-3458, 2008
The study has been interpreted as a challenge to the conclusions of my colleagues and me that no trial psychosocial intervention has ever achieved a positive effect with survival designated as a primary outcome and in which there was no medical co-intervention confound. The intervention involved providing women with strategies to reduce stress and improve mood and diet in ways believed to influence the likelihood of recurrence. The study has been widely hyped and now NCI is even offering free training and delivering this intervention, an issue I will address in a future blog. My colleagues and I examined this trial carefully and concluded in a published critique that survival was not in a primary outcome and there was a lack of evidence that an effect on survival had been achieved.
We noted that the article reporting survival inexplicably did not provide the usual unadjusted outcomes for survival, such as a Kaplan-Meier estimate, which would allow independent evaluation of claims of an effect on survival. Also, the number of women experiencing a cancer recurrence did not differ significantly between the intervention (25.4%) and control conditions (29.2%). Odds Ratio = 0.83, CI = 0.46 – 1.48, P = .525. The difference in median time to recurrence was small –six months– with the range of time to event approximately 11.8 years in the control group and 10.9 years in the intervention group. There was no difference in the proportion of women who died in the intervention group (21.1%) versus the control condition (26.5%), Odds Ratio = 0.74, CI = 0.40 – 1.36, P = .332, with a similar lack of results when we examined only those deaths due to breast cancer. Finally, the differences in recurrence (n=4) and survival (n=6) between the 2 groups was less than impressive.
This was about as far as we could go in re-analyzing the data available in their article. When we submitted our critical commentary to Cancer, Professor Anderson attempted to have it suppressed and when she did not succeed, she refused to offer a reply. She has since also refused to answer journalists’ questions concerning our commentary.
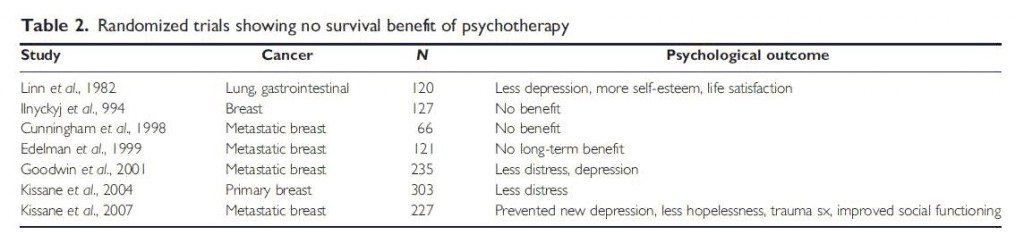
The Trials Considered Negative in the Psycho Oncology Article
My colleagues and I reviewed the trials considered negative in the Psycho Oncology article. Of the seven trials counted as negative, three (1, 2, 3) were large, well conducted and transparently reported trials with survival as an a priori outcome. A fourth smaller trial also had survival as an a priori primary outcome and included more patients who were actually exposed to the intervention than the original Spiegel Lancet study.
A fifth study achieved modest, but unsustained improvement on mood measures and no effects on survival, but there is no evidence that survival was an a priori primary outcome.
A sixth study explicitly rejected survival as an outcome for a sample of patients with stage IV cancer included on the basis of clinician judgment that they had less than 12 but more than three months to live. These patients were chosen on the assumption that being so close to death, “advanced intervention [of any kind] has relatively little impact on survival” and so psychotherapy focused on improving “the quality but not the length of survival”.
A final study by Ilnyckyj and colleagues excluded patients who were judged to need psychotherapy, but nonetheless provided psychotherapy in groups led by professionals who “were not instructed any specific techniques” and who lacked the guidance of any treatment manual. There was a breakdown randomization of the study, and no differences were found for psychological outcomes. The trial remained unpublished until a medical fellow who was not involved in the original study was inspired by publication of Spiegel’s Lancet article to undertake a 11 year follow-up. The study would have remained in obscurity because it in was published in a soon defunct journal (Annals of the Royal College of Physicians and Surgeons of Canada) and was not referenced in either PubMed nor ISI Web of Science, but it was included in a review by David Spiegel.
enlargeRelevant Trials Unmentioned in the Psycho Oncology Article
As I have noted, the Psycho Oncology article failed to note either a well-designed intervention study that failed to replicate Fawzy’s results or another study that failed to replicate subgroup analyses for Spiegel’s 2007 findings of differences associated with estrogen receptor status. Another study that was ignored was a large, well designed and well controlled study of a home intervention providing support and information to cancer patients and had null findings. Finally, a study of cognitive behavioral symptom management intervention for patients with solid tumors appeared too late to be included in the Psycho Oncology article, but meets the criteria by which other trials were included. Post hoc analyses revealed no effect on survival.
Boxscores are for Baseball, not the Evaluation of Clinical Trials
We can beconfident that the boxscores newspapers reported for the major leagues include the valid scores of all the relevant games with no games included that should not have been. For a variety of reasons, these conditions do not hold for boxscores of clinical trials, and most authorities reject and even ridicule reliance on boxscores for the evaluation of interventions has evidence-based.
The Psycho Oncology article gives an 8-7 boxscore for positive versus negative trials evaluating psychosocial interventions promoting survival of cancer patients. But the flaws in how this score was calculated highlight why most authorities negatively view boxscores. The trials counted as positive include three for which authors of the original study denied were tests of psychotherapy and another in which the group assigned to psychotherapy also received considerably more medical intervention. A fifth study had not even declared survival as a primary outcome, and classification of it as positive depends on secondary subgroup analyses. A sixth study also did not have survival as a primary outcome, used different rules for retaining intervention versus control patients, and relied on voodoo statistics to support claims of an effect on survival. A seventh study claimed to have obtained an extension of life for early breast cancer patients, but this claim depends on voodoo statistics, and the author has refused to respond to published criticisms.
The final trial classified as positive, Spiegel’s original Lancet study, will be discussed in detail in my next post, but it suffices to say here that it too was not designed with survival as the primary outcome.
Boxscore evaluations of clinical trials disregard the quality and even the aims of studies. None of the studies classified as positive had both survival a primary outcome a priori and had equivalent medical treatment delivered to intervention and control groups. In contrast, a number of negative studies designated had survival has an a priori outcome and some negative trials were simply not included in the Psycho Oncology evaluation.
We cannot quantify publication bias in the literature concerning whether psychosocial interventions affect survival, but we can establish that there it’s substantial. First, published trials that are accepted as relevant are a small subset of the many trials conducted to evaluate effects of interventions on psychological outcomes without survival as a primary outcome. There has been little interest in going to each of these studies to conduct post hoc follow-up survival analyses, particularly when the mechanism by which psychological intervention could influence survival is so undocumented. If someone were to attempt such a follow-up analysis and obtained negative findings, a report would probably not be published. The rationale for rejection was that the trial was not intended to test an effect on survival. On the other hand, finding an effect on survival in post hoc analyses would be a “man bites dog story” considered worthy of publication.
There is evidence of publication bias even for well-designed studies that designated survival as a primary outcome. Journal of Clinical Oncology published an extremely flawed study claiming positive results. Yet, when I contacted authors of well-designed studies with null findings, they reported that their manuscripts were rejected at Journal of Clinical Oncology. Confirmation bias is high, especially for the publication of studies with attention-getting hypotheses, even if they are implausible.
The hypothesis that psychotherapy can improve survival concerns a basic biomedical outcome, and yet evaluations of it have not adhered to the basic rules by which biomedical interventions are evaluated. I doubt whether the hypothesis would have kept in circulation if was evaluated by those rules. “Evidence” is summarily rejected in the biomedical literature when it has small samples with post hoc re-designations of primary outcomes, reliance on subgroup analyses and analyses that are not intent to treat, and ignoring of powerful confounds. Why should it be any different for psychosocial interventions that allegedly affected the same important biomedical outcome, death?
Claims that psychotherapy promotes survival of cancer patients represent the same woo science that is used for other complementary and alternative interventions. These false claims can confuse patients making difficult choices about accepting disfiguring and painful medical procedures with established efficacy. Moreover, particularly at the end of life, the false hope of psychotherapeutic intervention extending patients lives can distract them from putting their lives in order and planning for a good death, unburdened by anyone’s expectation that they need to fight on.
I renew my offer to publicly debate the hypothesis that psychotherapy promotes survival. I’m sure we could sell a lot of tickets and I would donate my proceeds to a charitable cause offering psychosocial interventions to improve the quality of life of under-served cancer patients and their caregivers.

