
When I was pregnant, I obediently took the iron pills and prenatal vitamins prescribed by my obstetrician. And I prescribed them for every pregnant patient I took care of as a family physician. I never questioned the practice. It seemed intuitively obvious that it was a good thing; we know pregnancy makes extra nutritional demands and depletes iron stores. It never occurred to me to question what I had been taught, because it seemed perfectly logical. I did question other things I was taught that didn’t seem so logical. In my internship, we were ordered to do episiotomies on every patient (the rationale was that it made birth less traumatic for the baby and prevented uncontrolled perineal tearing in the mother). I was severely chastised for omitting an episiotomy on a patient who begged me not to do one. She had had several babies and was stretchy enough to deliver easily without an episiotomy. In this case, my common-sense clinical judgment was vindicated by further research in the years after my internship; new evidence showed that routine episiotomies were of no benefit, practice changed in response to the new evidence, and episiotomies are no longer done routinely.
That was a long time ago. I have long since learned that even the most reasonable assumptions can be wrong. I happened to be right about episiotomies, but I might just as well have been wrong; and the only way to know whether a belief is true is to test it in controlled scientific trials. As Will Rogers said, “It isn’t what we don’t know that gives us trouble, it’s what we know that ain’t so.” It turns out that routine multivitamin and iron supplementation is not supported by any convincing evidence from scientific studies. And practice is changing. Recently, when one woman asked her OB what she should do about prenatal vitamins he pulled his wastebasket out from under his desk and said “put them there.”
The evidence for folic acid
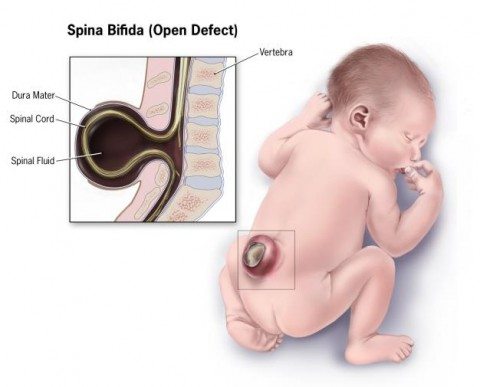
Spina bifida, one of the consequences of insufficient folic acid.
Folic acid prevents serious congenital abnormalities, neural tube defects like spina bifida and anencephaly. It is recommended for any woman who might become pregnant, because the damage occurs early, sometimes before she knows she is pregnant. The United States Preventive Services Task Force (USPSTF) found high quality (Grade A) evidence to support their recommendation that “All women planning or capable of pregnancy take a daily supplement containing 0.4 to 0.8 mg of folic acid.”
The American Academy of Family Physicians seconds that recommendation and recommends folic acid supplementation be continued for the first 6-12 weeks of pregnancy. But it points out that many other elements of routine prenatal care are based on tradition and lack a firm evidence base. It makes recommendations about healthy diet, but it doesn’t make specific recommendations about prenatal multivitamins. It doesn’t recommend iron supplements for all pregnant women, only for those with iron deficiency anemia.
The evidence for iron
The USPSTF found insufficient evidence to recommend for or against routine iron supplementation in pregnancy. In summary, it said:
routine iron supplementation during pregnancy may improve maternal hematologic indices and reduce the incidence of iron deficiency and iron deficiency anemia (IDA) in the short term. However, there is no clear or consistent evidence that prenatal iron supplementation has a beneficial clinical impact on maternal or infant health. In addition, no trials are available on the effect of prenatal screening for IDA on clinical outcomes despite routine screening practices in many high-income countries. Rigorous studies are needed to fully understand the short- and long-term effect of routine iron supplementation and screening during pregnancy on women and infants, including the effects on rates of cesarean delivery, small size for gestational age, and low birthweight. Until then, the evidence on routine iron supplementation and screening in prenatal care will remain unclear at best.
The evidence for multivitamins
The American Congress of Obstetricians and Gynecologists (ACOG) recommends a multivitamin with folic acid.
A review of the literature found evidence to support routine folic acid supplementation but not supplementation of omega-3 fatty acids, vitamin D, or iron. It found evidence of harm from supplementation with large doses of vitamins A, C, and E. As for multivitamins, it concluded:
Vitamin and mineral supplements cannot replace a healthy diet, and there are not enough high-quality data to recommend multivitamin supplements for all American women.
The Skeptical OB, Amy Tuteur, says:
Folic acid does prevent neural tube defects like spina bifida. The rest of the vitamins in prenatal vitamin preparations probably don’t provide any benefit for women who are well nourished.
Evidence of harm?
There is little evidence of harm from routine supplementation with multivitamins and iron. Some women have trouble swallowing pills, especially when they suffer from morning sickness. Allergic reactions to components in the pill can occur, but they are rare. Some patients report constipation, diarrhea, and nausea, which can often be relieved by switching to a different formulation.
Diet instead of pills?
There’s no reason to think that the nutritional needs of pregnancy can’t be adequately met through diet alone. There are published dietary guidelines for pregnant women. In addition to the general nutritional advice that is applicable to everyone, specific advice for pregnant women includes:
- Minimize intake of food and drinks containing saccharin (other artificial sweeteners are probably OK).
- Limit consumption of caffeine (possible association of high caffeine intake with spontaneous abortion and low birth weight; moderate amounts are probably safe).
- Most pregnant women require an additional 300-400 calories a day beyond what would normally be required to maintain their weight when not pregnant.
- Avoid unpasteurized dairy products, delicatessen foods, pâtés, and meat spreads (risk of Toxoplasma and Listeria contamination, based on case reports).
- Avoid raw eggs (risk of Salmonella contamination, based on case reports).
- Fruits and vegetables: wash before eating.
- Avoid certain herbal teas that have been associated with adverse outcomes, like chamomile, licorice, peppermint, or raspberry leaf; teas containing ginger, citrus peel, lemon balm, and rose hips are probably safe in moderation.
- Reheat leftover foods thoroughly before eating.
- Avoid undercooked meat; cutting boards, utensils, and hands should be washed with hot, soapy water after contact with uncooked meat.
- Liver and liver products should be eaten in moderation (risk of vitamin A toxicity).
- Avoid shark, swordfish, mackerel, tilefish, and tuna steaks and limit intake of other fish (to minimize mercury intake).
- Avoid refrigerated smoked seafood, raw fish, and shellfish; eat farmed salmon in moderation.
Dietary sources of iron include fruits, vegetables, meat, and poultry. The non-heme iron in vegetarian diets is not as well absorbed as the heme iron from meat, so vegetarians have almost double the requirement for iron compared to women who eat meat.
“It seemed like a good idea at the time”
One of my husband’s friends was shocked to hear that he had finally married at age 41; everyone thought of him as a confirmed bachelor. My husband explained, “Yes, I got married. It seemed like a good idea at the time.” Thirty-four years later, after raising two daughters, he still thinks it was a good idea. Routine prescription of prenatal vitamins and iron seemed like a good idea at the time, and it might still be a good idea, at least for women who are at risk of anemia or inadequate diet. The lack of evidence of benefit doesn’t necessarily mean the practice should be abandoned. The chance of harm is minimal.
Conclusion: There are no absolutes regarding prenatal vitamins
There is compelling evidence to support the use of folic acid supplements before pregnancy and during the first trimester. There is no good evidence to support the routine use of multivitamins or iron, but there is no good reason not to use them. If doctors recommend them, they should be honest about the uncertainty of the evidence and let their patients participate in the decision. Our own Scott Gavura has provided some guidance on selecting a prenatal multivitamin. Whether or not patients choose to take multivitamins and iron, they should be given guidance about a healthy diet that meets the nutritional needs of mother and child.
Incidentally, this is a good example of how mainstream medicine is willing to re-examine its own practices and change course. Something alternative medicine never seems to do.
