The scientifically-accepted mechanism by which multiple sclerosis causes symptoms
Multiple sclerosis (MS) is fascinating illness that can range from mild annoyance to debilitating nightmare. The frightening nature and unclear cause of the disease makes it a magnet for questionable medical therapies (i.e. quackery). A piece published last week in (surprise!) The Huffington Post helps fuel the fires of suspicion and paranoia while failing to shed any light on the future of MS research.
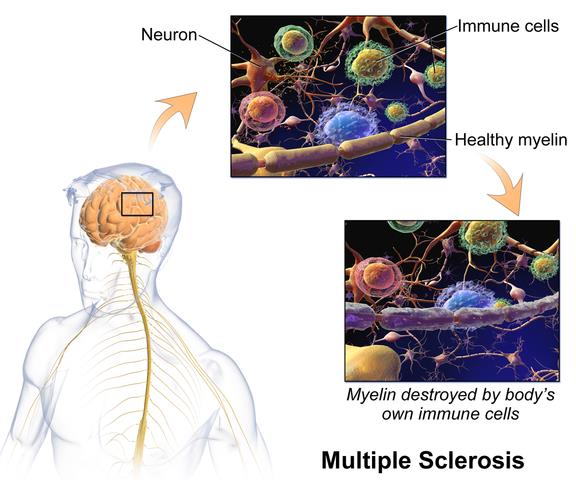
Multiple sclerosis is a disease of the nervous system. Its victims develop symptoms based on what part of the nervous system is affected. For example, if MS attacks the optic nerve, a patient may experience blurry vision or blindness. If it affects the motor areas of the brain that controls the left leg, the patient will develop weakness in the left leg. Typically, the symptoms will last a certain period of time and then improve, but often not completely back to normal.
Unknown causes, varying effects, and imperfect treatments
The exact initial cause of the disease isn’t known, but we do have a good understanding of how the disease works. In MS, the immune system attacks the sheath surrounding certain types of nerve cells. This leads to “plaques” in nervous tissue such as the brain, and these plaques correspond to the symptoms of MS. The disease appears to result from a combination of a genetic predisposition and some sort of environmental insult, such as a viral infection. Many people have T-cells in their immune system that recognize myelin, the substance attacked in MS, but in MS these T-cells are more capable of attacking myelin. In order to do this effectively they must breach the “blood-brain barrier”, a system that keeps the circulation in the brain protected from toxins, infections, and the immune system. In MS, this barrier is breached, perhaps by infection, allowing T-cells into the brain to coordinate an attack on the nerve cells. Based on our still-incomplete knowledge of the disease, we have developed some pretty effective treatments over the last decade or so. These treatments are based on drugs that affect the immune system. All of these drugs have significant side effects and none are completely effective. There are probably many different “kinds” of MS based on different genetics and different environmental triggers, so we have a long way to go in understanding the disease and developing treatments. Given the fear and debility associated with the disease, and our still-incomplete knowledge, it’s natural for people to look for (and see) patterns where none exist. Diseases like MS attract quackery (such as bee-sting therapy) and conspiracy theories, such as the one in The Huffington Post.
It started with an article in The Globe and Mail, Canada’s national newspaper. This article detailed some new MS researcher by an Italian doctor named Paolo (I kid you not) Zamboni. Dr. Zamboni hypothesized that MS may be at least partly due to a problem with venous blood flow in the brain, and that a surgical procedure can correct this blood flow and improve MS symptoms. He has done some small studies to evaluate these claims. These studies have not yet been replicated by other researchers, and it isn’t clear (at least to me) how plausible his hypothesis is. Still, it is interesting, and the Globe and Mail article was fairly well-written, providing a counter-balance to Zamboni’s exuberance:
“I am confident that this could be a revolution for the research and diagnosis of multiple sclerosis,” Dr. Zamboni said in an interview…Not everyone is so bullish: Skeptics warn the evidence is too scant and speculative to start rewriting medical textbooks. Even those intrigued by the theory caution that MS sufferers should not rush off to get the surgery – nicknamed the “liberation procedure” – until more research is done.
The National MS Society (US) is also taking a cautious approach and is facilitating further research into this new theory.
Throwing caution to the windbags
“Cautious” is not a word that ever applies to medical reporting in The Huffington Post. Erika Milva vilifies the American press and the MS society, blaming entrenched interests for failing to jump on Zamboni’s ideas.
Of the MS society’s statement, Dr. Lorne Brandes, an oncologist who blogs for CTV News’ Health Blog, wrote, “If their official response to Dr. Zamboni’s research was any cooler, icicles would form on their spokespersons’ lips. Why am I not surprised? These organizations are big money operations, run by risk-adverse professionals and fundraisers who are absolutely petrified of making a mistake and prematurely backing a losing horse. Their interests are also heavily intertwined with those of Big Pharma.”
This is absurd. Advocate groups such as the NMMS are often supported by patients and their families and others who are strongly motivated to get results. The MS society is actively seeking researchers to help investigate these new findings but is cautioning patients not to jump to quickly after unproven therapies.
It is important for researchers to think outside the box and we believe Dr. Zamboni has done this. His hypothesis is a path that must be more fully explored and Dr. Zamboni himself has stated that additional research is essential to evaluate it…The National MS Society is pursuing follow-up research in how CCSVI might be involved in the MS process and we have invited investigators from around the world whose research is relevant to MS to submit proposals to apply for grants that would explore this lead. These applications will undergo an accelerated review process.
Where is the tepid, icicle-laden response?
Diseases that inspire fear, as MS legitimately does, attract a great deal of emotional attention. This type of attention, when applied to real research, can drive progress in science. When this enthusiasm is decoupled from science, the door for quackery is open, and anyone can and will walk in.
Further reading
- Frohman EM, Racke MK, & Raine CS (2006). Multiple sclerosis–the plaque and its pathogenesis. The New England journal of medicine, 354 (9), 942-55 PMID: 16510748
- Zamboni, P., Galeotti, R., Menegatti, E., Malagoni, A., Tacconi, G., Dall’Ara, S., Bartolomei, I., & Salvi, F. (2008). Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis Journal of Neurology, Neurosurgery & Psychiatry, 80 (4), 392-399 DOI: 10.1136/jnnp.2008.157164
- Zamboni, P., Galeotti, R., Menegatti, E., Malagoni, A., Gianesini, S., Bartolomei, I., Mascoli, F., & Salvi, F. (2009). A prospective open-label study of endovascular treatment of chronic cerebrospinal venous insufficiency Journal of Vascular Surgery, 50 (6), 1348-1358000 DOI: 10.1016/j.jvs.2009.07.096
