Whether you call them hot flashes or “power surges,” the symptoms of menopause can be very distressing. They were routinely treated with hormone replacement therapy (HRT) until the Women’s Health Initiative study in 2002 persuaded many patients and doctors to abandon that treatment. The results of that study were misunderstood by some and questioned by others, and there continues to be confusion about what the evidence shows and how menopausal symptoms should be treated. We have learned much more about this subject since 2002. HRT is still the most effective treatment and can be used safely under the new treatment guidelines.
The history of hormone replacement therapy
In the second half of the 20th century, there was much enthusiasm about estrogen. Mimicking the estrogen levels of a young woman was seen as a way to remain young and healthy. Doctors recognized that there were risks, but they seemed minor. There were studies showing that HRT protected women from the increased risk of heart disease after menopause. Few if any doctors prescribed it solely to prevent heart disease, but cardiovascular protection and osteoporosis prevention were seen as added benefits that served to tip the balance towards a decision to prescribe it for menopausal symptoms.
Then the Women’s Health Initiative study (WHI) dropped a bomb. It found that HRT didn’t protect women from cardiovascular disease after all. It showed that HRT did more harm than good. The number of prescriptions dropped by as much as 80%. Many women turned to alternative treatments that had not been studied anywhere near as extensively as HRT.
The Women’s Health Initiative study
The WHI found that women who took HRT were more likely to develop coronary heart disease, stroke, deep-vein thrombosis (blood clots), and breast cancer. That was the message that came out in the media, quickly followed by accusations that doctors had been killing women by prescribing HRT. That was flat wrong: there was no difference in all-cause mortality between women who took HRT and women who didn’t. And they found benefits: there was a significant reduction in the risk of colorectal cancer and osteoporotic bone fractures.
The study’s findings were far more nuanced than the media reported. The WHI study was really two separate studies, of estrogen and of combined estrogen/progesterone. Women with an intact uterus shouldn’t take estrogen alone because unopposed estrogen stimulation can cause endometrial cancer. But by age 60, one-third of women have had a hysterectomy, and they can be treated with estrogen alone. The greatest risks were found in women who took combination estrogen/progesterone. When estrogen was used alone, the risks were considerably less.
As the data were analyzed and reanalyzed, it became clear that the patient’s age makes a difference. Taking estrogen close to the time of menopause caused little harm and provided a number of benefits. This graph is from a 2016 Perspective article in The New England Journal of Medicine.
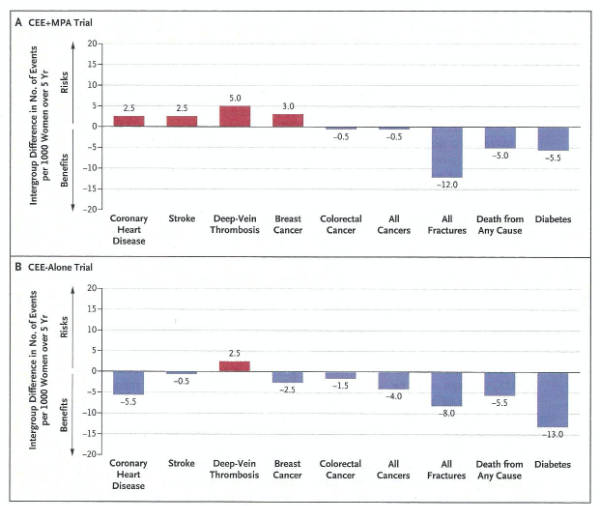
“Results are shown for the two formulations, conjugated equine estrogens (CEE) alone or in combination with medroxyprogesterone acetate (MPA), for women 50 to 59 years of age. Risks and benefits are expressed as the difference in number of events (number in the hormone-therapy group minus the number in the placebo group) per 1000 women over 5 years. Data are from Manson et al.5” (click to embiggen)
It shows the data for women 50-59 who took combination HRT (panel A) or who took estrogen alone (panel B). Red is bad, blue is good. You will probably be surprised at the amount of blue. For estrogen alone, HRT only increased the risk of deep vein thrombosis while it decreased the risks of coronary heart disease, stroke, breast cancer, colorectal cancer, all cancers, all fractures, death from any cause, and diabetes. For combined therapy there were four areas of increased risk, but treatment decreased the risk of colorectal cancer, all cancers, all fractures, death from any cause, and diabetes.
HRT recommendations
Numerous professional organizations have examined the evidence and come up with new treatment guidelines. The “2012 Hormone Therapy Position Statement of the North American Menopause Society” provides a good overview of the evidence and concludes:
Recent data support the initiation of HT around the time of menopause to treat menopause-related symptoms and to prevent osteoporosis in women at high risk of fracture. The more favorable benefit-risk ratio for ET allows more flexibility in extending the duration of use compared with EPT, where the earlier appearance of increased breast cancer risk precludes a recommendation for use beyond 3 to 5 years. [ET = estrogen therapy, EPT = estrogen/progesterone therapy.]
It stresses individualization of treatment and consideration of personal risk factors.
Bioidentical hormones
Today, 35% of current hormone users are taking bioidentical hormones from unregulated compounding pharmacies, despite concerns about contamination and dose consistency, and despite the lack of evidence for their safety and effectiveness. “Bioidentical” is something of a misnomer: they are “identical” only to one or two of the long list of sex hormones in a woman’s body, and there’s no way they could mimic the complex dance of all those hormones as their levels fluctuate naturally over hours and days.
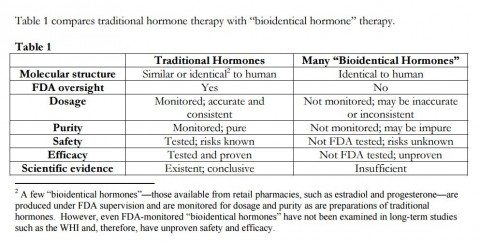
For a good overview of bioidentical hormones, see the position statement of The Endocrine Society. Their findings are summarized in this table (click to embiggen):
Non-hormonal treatments for menopause
The North American Menopause Society has a position paper on non-hormonal management for women who are unable or unwilling to take hormones:
- Recommend: cognitive behavioral therapy, hypnosis, paroxetine, and possibly a few other prescription drugs
- Recommend with caution: weight loss, mindfulness-based stress reduction, soy isoflavones, and stellate ganglion block
- Do not recommend: cooling techniques, avoidance of triggers, exercise, yoga, paced respiration, relaxation, over-the-counter supplements and herbal therapies, acupuncture, calibration of neural oscillations, and chiropractic interventions.
Conclusion: Once again, the media got it wrong
Hormone replacement therapy fell into disfavor following the Women’s Health Initiative study, in part because the results were poorly reported by the media and were widely misunderstood. HRT remains the most effective and best-studied treatment for hot flashes, and the benefits outweigh the risks if treatment is individualized, if it is started close to the time of menopause, and if it is used for a limited period. It has significant benefits for a number of other health conditions like osteoporosis, and in the 50-59 year age group it appears to reduce all-cause mortality.