The carotid artery in the neck is a common site of atherosclerosis. As plaque builds up, it leaves less room for blood flow and can cause strokes through clotting or embolization. Carotid stenosis is defined as a greater than 70% narrowing of the lumen (the space through which the blood flows in an artery). It can cause symptoms, including transient ischemic attacks (TIAs) and minor strokes; but it is frequently asymptomatic. It can be treated with carotid endarterectomy (CEA) or carotid angioplasty and stenting (CAAS). There has been much discussion about which procedure is better and when it is better not to do either.
What are the risks?
Symptomatic carotid artery stenosis (with TIAs or minor strokes) requires prompt evaluation and triage. After a TIA, the risk of stroke is increased. There is a scoring system using age, blood pressure, clinical features, duration of symptoms, and diabetes. Patients with the lowest score have a 1.2% risk of stroke within 7 days, and those with the highest score have a risk of 11.7%. There is compelling evidence that endarterectomy benefits symptomatic patients. It reduces the risk of a major stroke in the next two years by 80%. Overall, the number needed to treat (NNT) is eight operations to prevent one stroke.
Asymptomatic carotid artery stenosis of 75% or less carries a stroke risk of 1.3% annually. When stenosis is more than 75%, the combined rate for TIA and stroke is 10.5% per year, but some of those strokes are cerebral hemorrhages or lacunar infarcts that would not be expected to benefit from endarterectomy. Early studies found that surgery significantly lowered the risk of stroke, but better subsequent studies found little or no benefit. By one estimate, the number needed to treat to prevent one stroke over 5 years is around 40. Because of the relatively low risk of surgery-preventable strokes, experts have generally called for surgery to be restricted to cases where the peri-operative risk is less than 3%, where the stenosis is greater than 80%, and where the surgeon is experienced.
Surgical risks cover a wide risk of complications ranging from infection to death. Risks are greater in symptomatic patients and in facilities where fewer procedures are done.
Acceptable guidelines for operative risks have been developed: risk of stroke or death of 3% for asymptomatic patients, 5% for patients with TIA, 7% for patients with stroke, and 10% for patients with recurrent stenosis. But these guidelines are being questioned. They were based on studies with selected patients and experienced surgeons, and medical treatment has improved since those studies were done. The annual rate of stroke in asymptomatic carotid stenosis may now be less than 1% with medical treatment. In the real-world setting today, the relative benefit of surgical vs. medical treatment is smaller than the studies indicated, and the risks of surgery seem less reasonable.
What are the treatment options?
There are basically three options: lifestyle modification, medications, and procedures.
Lifestyle modification includes anything that will reduce the risk of a stroke and reduce the progression of arteriosclerosis, including smoking cessation, exercise, and diet. Of course, these preventive measures are advisable for everyone, not just for patients with carotid stenosis.
Medications include antiplatelet medications like aspirin and clopidogrel (Plavix), drugs to reduce blood pressure, and statins, which not only reduce cholesterol levels but also reduce inflammation, reduce the formation of clots, and help stabilize plaques.
Procedures include invasive open surgery and less invasive stent placement.
In carotid endarterectomy (CEA) an incision is made in the neck; the artery is exposed, opened, and plaque is removed.
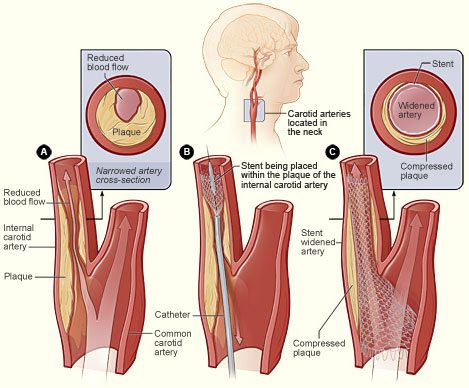
In carotid angioplasty and stenting (CAAS) an incision is made in the groin. A catheter is threaded into the femoral artery and guided up through the aorta and into the carotid artery, where a balloon is inflated to break up plaque and a wire-mesh stent is left in place to maintain the enlarged space for blood flow.
CEA equivalent to CAAS
Two studies reported in the March 17, 2016 issue of The New England Journal of Medicine by Rosenfield et al. and Brott et al. compared stents to endarterectomy and found no significant differences in long-term outcomes.
Beyond deciding the merits of surgery vs. stenting, the bigger question is whether asymptomatic patients will benefit from either procedure. The accompanying editorial points out that “More than 90% of carotid-artery interventions are performed in asymptomatic patients, even though evidence suggests that up to 90% of them will undergo an ultimately unnecessary and potentially harmful procedure.” In the US, 90%; in Germany and Italy, 60% of surgeries are done on asymptomatic patients; in Canada and Australia, 15%; and in Denmark, 0%. Why such a discrepancy? Doctors in all those countries have access to the same evidence from scientific studies, but apparently they have different opinions about the levels of risk and benefit that justify performing invasive procedures. I can only speculate about other possible reasons such as financial considerations.
What about screening?
The US Preventive Services Task Force (USPSTF) recommends against screening asymptomatic people in the general population for carotid stenosis because screening is likely to do more harm than good. A detailed explanation of their reasoning and the evidence they relied on can be found here.
They point out that “no externally validated risk stratification tools can reliably distinguish between persons who have clinically important carotid artery stenosis and those who do not or those who will experience harm after treatment with CEA or CAAS.” They conclude:
The USPSTF found no evidence that screening for carotid artery stenosis leads to additional treatment and benefit beyond standard preventive treatments based on traditional cardiovascular risk factors. In patients and surgeons similar to those in the RCTs, treatment with CEA for asymptomatic carotid artery stenosis can result in a net absolute reduction in stroke rates, but this benefit has only been shown in selected patients with selected surgeons and must be weighed against a small increase in nonfatal myocardial infarctions. The net benefit of CEA largely depends on patients surviving the perioperative period without complications and living for at least 5 years. The magnitude of these benefits would be smaller in asymptomatic persons in the general population than among patients in RCTs.
For the general primary care population, the magnitude of benefit is small to none. Adequate evidence indicates that both the testing strategy for carotid artery stenosis and treatment with CEA or CAAS can cause serious harms. In selected centers similar to those in the trials, CEA is associated with a 30-day stroke or mortality rate of approximately 2.4%; reported rates are as high as approximately 5% in low-volume centers and 6% in certain states. Myocardial infarctions are reported in 0.8% to 2.2% of patients after CEA. The 30-day stroke or mortality rate after CAAS is approximately 3.1% to 3.8%. The overall magnitude of harms is small to moderate depending on patient population, surgeon, center volume, and geographic location.
Conclusion: Current practice for carotid artery stenosis – more harm than good
Scientific studies have provided us with considerable evidence about carotid artery screening and treatment; but for whatever reason, the evidence has often been disregarded. Carotid endarterectomy and angioplasty/stenting are being done on too many asymptomatic patients in the US. And asymptomatic people in the general population are getting carotid ultrasound screening (often from direct-to-consumer businesses like Lifeline) despite the evidence that it does more harm than good.
I agree with the authors of the NEJM editorial:
Outside clinical trials, endarterectomy and stenting should be reserved for patients with symptomatic severe stenosis or for asymptomatic patients who are shown to be at higher risk for stroke with medical therapy than with intervention. Such patients (approximately 10 to 15% of patients with asymptomatic stenosis of 70 to 99%) may be identified by an algorithm that incorporates information about microemboli detected by means of transcranial Doppler, and in the future by imaging strategies that identify the vulnerable plaque.