A recent article by David Zweig titled New Research Suggests Number of Kids Hospitalized for COVID Is Overcounted claimed:
The reported number of COVID-19 hospitalizations, one of the primary metrics for tracking the severity of the coronavirus pandemic, was grossly inflated for children in California hospitals, two research papers published Wednesday concluded.
The two papers were accompanied by a commentary by Drs. Amy Beck and Monica Gandhi titled Adjudicating Reasons for Hospitalization Shows That Severe Illness From COVID-19 in Children Is Rare. The commentary claimed that “Both demonstrate that reported hospitalization rates greatly overestimate the true burden of COVID-19 disease in children.” I believe there are several limitations to these studies that make it difficult to reach the conclusion that harms to children from COVID-19 have been greatly exaggerated.
Let’s examine these studies further. As screening for SARS-CoV-2 is now standard of care at most hospitals, both studies examined all admitted children who tested positive for SARS-CoV-2. They retrospectively reviewed their charts to best determine which percentage of COVID-19 cases were found incidentally. An example of incidental infection would be a child who suffered a fracture and tested positive for SARS-CoV-2 upon admission screening.
The first paper: Webb & Osburn
The first paper is titled Characteristics of Hospitalized Children Positive for SARS-CoV-2: Experience of a Large Center by Drs. Nicole Webb and T. Shea Osburn. The study was conducted at the second-largest children’s hospital in California and included patients 22 years or younger. It spanned 5/1/2020 to 9/30/20, several months before California’s big COVID-19 surge. It found 163 patients screened positive for SARS-CoV-2 on admission. 17 patients were diagnosed with multisystem inflammatory syndrome (MIS-C), a potentially severe complication of COVID-19 in children. These 17 patients were excluded from the analysis as the “focus was acute SARS-CoV-2 positivity”, leaving 146 patients for their analysis. The authors reviewed these charts to determine if the COVID-19 diagnosis was incidental, potentially symptomatic, or significantly symptomatic
Of these 146 patients, 58 (39.7%) were classified as having incidental infection. Of the children with symptomatic COVID-19, some were very sick. Twenty children (14%) were “significantly symptomatic” defined as “patients with respiratory or cardiac symptoms consistent with COVID-19 requiring respiratory support or ICU-level care”. These children were hospitalized for an average of 12.6 days. Several patients required “substantial respiratory support”. One 16-year-old “medically complex” child died of COVID-19. Children with common conditions, namely obesity and asthma, which are present in at least 20% of American children, were at higher risk for severe disease.
The second paper: Kushner et al.
The second paper by Kushner et al. is titled For COVID” or “With COVID”: Classification of SARS-CoV-2 Hospitalizations in Children. It examined children 18-years or younger from 5/10/20 to 2/10/21. It started the day universal screening of all admissions began at this hospital. 117 children were identified. Of these, 39.3% were asymptomatic and 45% of admissions were categorized as unlikely to be caused by SARS-CoV-2. Again, some of the children with symptomatic COVID-19 were very sick. 7.7% had severe illness, and 12.8% had critical illness. 26.5% required ICU admission due to COVID-19 or MIS-C. One immunocompromised child died.
So are the numbers inflated?
On Twitter, science writer David Zwieg stated that “Pediatric COVID hospitalization numbers are inflated by *at least* 40%, per two peer reviewed studies”:
Pediatric COVID hospitalization numbers are inflated by *at least* 40%, per two peer reviewed studies
It's hard to overstate the significance of this
My 🔥SCOOP🔥 for @NYMag, with official commentary from @MonicaGandhi9 and context from @sdbaral
— David Zweig (@davidzweig) May 19, 2021
Mr. Zwieg wrote in an article for New York Magazine that “the official tallies were found to be so far off.” Which “official tallies” are these? Beyond the two specific California hospitals where the studies occurred, he does not say. Drs. Beck and Gandhi also claim that the studies “demonstrate that reported hospitalization rates greatly overestimate the true burden of COVID-19 disease in children?” Which specific source for “reported hospitalization rates” do Drs. Beck and Gandhi think is flawed? They do not say, and no reference is given for their claim.
But are they right? Are incidental SARS-CoV-2 infections frequently included in the hospitalization tallies? The best answer I can give is: Likely yes, but it depends on the tally, undercounting may be a bigger problem, and even using the lowest estimate, the number of hospitalized children is not trivial.
How many children have been hospitalized due to COVID-19?
Getting accurate information on exactly how COVID-19 has affected children is difficult. There are several “reported hospitalization rates”, and several tallies of hospitalized children. Additionally, recognizing that undercounting is a significant problem, the CDC has tried to estimate the actual number of hospitalized children. Organizations openly acknowledge the significant challenges they face in trying to accurately determine the number of children hospitalized with COVID-19. For example, the American Academy of Pediatrics (AAP) notes that the “format, content, and metrics of reported COVID-19 data differed substantially by state”. Different states even have different definitions of at what age someone is considered a child.
Given the difficulty in collecting accurate information, the range of pediatric hospitalization rates is wide. According to the AAP, “Children were 1.3%-3.1% of total reported hospitalizations, and between 0.1%-1.9% of all child COVID-19 cases resulted in hospitalization”. Overall, the AAP calculates that 0.8% of children with COVID-19 are hospitalized. A CDC report found that among 69,700 laboratory-confirmed cases of COVID-19 in children younger than 20 years, 2,082 were hospitalized (3%). This study relied “on information systems developed at the local, state, and federal level over decades for communicable disease surveillance that were rapidly adapted to meet an enormous, new public health threat”. Another study by Preston et al. of 869 medical facilities and 20,714 children with COVID-19 found that 2,430 (11.7%) were hospitalized. It included children “who had an inpatient or emergency department encounter with a primary or secondary COVID-19 discharge diagnosis”.
It would be interesting to examine the 2,082 cases in the CDC report and the 2,430 cases in the study by Preston et al. to see if any children with fractures and such were included in the count. It certainly wouldn’t surprise me if a high percentage were. But even if that were the case, these studies again demonstrate that COVID-19 can take a severe toll on some children. In the study by Preston et al., 31% of hospitalized children had severe COVID-19, which was defined as care “requiring treatment in an intensive care unit or step-down unit, involving use of invasive mechanical ventilation, or resulting in death.” In the CDC study, 17% of children required care in the ICU.
Though there is no single “official” count of all hospitalized children in the US, there are several tallies. The AAP aggregates statewide data and there are two federal datasets. These are all prone to two problems: including incidental SARS-CoV-2 cases and undercounting cases.
The AAP’s tally began with 891 cases on 5/21/2020 (at the tail end of the pandemic’s first wave) with data from 17 states and New York City. It currently collects data from 24 states and New York City. California, where both studies were conducted, is not one of these states. From these state dashboards, it reports that 16,013 children have been hospitalized. Extrapolating from this, one can estimate that between 35,000-40,000 children have been hospitalized in the US. The AAP acknowledges that the state dashboards may include incidental SARS-CoV-2 infections, writing “At this time, states are not providing data related to symptoms”.
Do all of these state dashboards systemically inflate hospitalizations as is implied? While it is entirely plausible that a large number of incidental SARS-CoV-2 infections have been counted in many, perhaps all, states, I’ve not seen anyone level this charge against any particular state. It’s just assumed, without concrete evidence, that because two hospitals in California counted incidental SARS-CoV-2 that infections every other dataset in the entire country is similarly flawed. Perhaps this is so, but that’s a pretty big assumption. I will note that both hospital systems where I work, New York University and the NYC Health and Hospitals Corporation, require clinicians to distinguish symptomatic from asymptomatic cases from the moment the test is ordered:
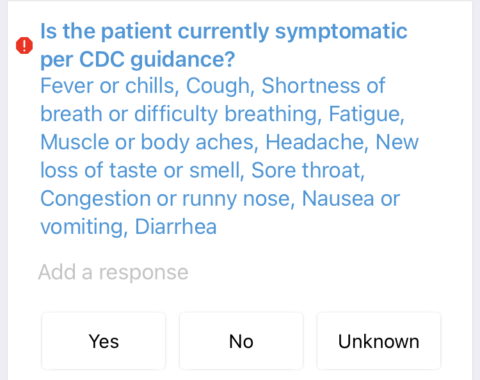
A question I must answer with every COVID-19 test I order.
I always thought this was to give extra information to the person performing the test. I was wrong. Per my discussions with epidemiologists at both hospitals, this is so admissions can be categorized as either “due to COVID” or “COVID positive, admission due to non-COVID reasons”. So, unlike the two California hospitals in this study, other (larger) hospital systems do make an effort to distinguish between incidental and symptomatic SARS-CoV-2 infections. The AAP notes that two states (Arizona and Nebraska) have made downward revisions of cumulative child hospitalizations, indicating that states try to report data accurately and correct errors when discovered. Of course, undercounting is a problem as well. For example, Georgia, where 1,260 children have been hospitalized, notes that their methods do “not capture hospitalizations that occur after a confirmed case was reported and, as such, is likely an underestimation of actual hospitalizations”.
At the federal level, the CDC maintains a dataset called COVID-NET that covers 100 counties in 14 states representing all 10 U.S. Department of Health and Human Services regions. As of 5/15/2021, COVID-NET reports that 2,960 children under 17-years have been hospitalized. As COVID-NET covers about 10% of the US population, this implies that about 30,000 children have been hospitalized throughout the US. Most hospitalized children had no underlying condition.
According to Dr. Christopher A. Taylor, the Deputy Lead at COVID-NET, “COVID-NET includes all children who tested positive for SARS-CoV-2 during hospitalization or up to 14 days prior to admission even if their primary reason for admission was likely not related to COVID-19-associated illness.” As such, this tally almost certainly contains cases of incidental SARS-CoV-2 infection. However, undercounting is a potential problem too. In discussing their numbers, the CDC states “the rates provided are likely to be underestimated as COVID-19-associated hospitalizations can be missed due to test availability and provider or facility testing practices.”
An early study based on this data, when 576 children had been reported, involved a complete medical chart review for 208 of them. The study did not mention the discovery of any cases of “incidental” SARS-CoV-2 infection in their chart review, but that doesn’t mean they weren’t there. Consistent with every other study, some of the children were very sick. Sixty-nine (33.2%) were admitted to the ICU, and invasive mechanical ventilation was required by 12 (5.8%). Hispanic and Black children had the highest rates of COVID-19–associated hospitalization, a universal finding in all studies. One child with multiple underlying conditions died.
A dataset maintained by the U.S. Department of Health & Human Services has collected 20,425 pediatric hospitalizations. Given that it relies on “facility-level data for hospital utilization,” it too certainly contains some children with incidental SARS-CoV-2 infection. Either through false negatives, lack of testing capacity or incomplete reporting, many cases of hospitalization due to COVID-19 are surely missed.
Yet other numbers are available. Another CDC report found 11,882 children younger than 17-years had been hospitalized by 12/12/2020, before the pandemic’s peak in January 2021. 7.4% of children in this study needed ICU-level care, a lower rate than other studies. According to data presented by the CDC during the Emergency Use Authorization for the COVID-19 vaccine, 13,000 children between the ages of 12-17 years had been hospitalized. The hospitalization rate for children due to COVID-19 is higher than during the 2009-10 H1N1 influenza pandemic.
As these datasets tally reported hospitalizations to governmental agencies, they are likely a substantial undercount. The CDC has tried to estimate the actual number, writing “Because current surveillance systems do not capture all cases of COVID-19 occurring in the United States, CDC provides these estimates to better reflect the larger burden of COVID-19.” The CDC has a discussion on the limitations of simply counting hospitalizations, noting many ways in which cases could have be missed, especially early in the pandemic when testing was scarce. They created a “simple probabilistic multiplier model” to estimate hospitalizations that is similar to how they have estimated the flu burden for years.
This CDC estimate of hospitalized children is significantly higher than the tallies discussed so far. For the entire population of the United States, the CDC estimates the actual number of hospitalizations is 2.5 times the reported number and pediatric hospitalizations were the most prone to undercounting, writing that “underdetection multipliers…were consistently highest among children.” If this model is correct, then the state and federal tallies are much more likely to underestimate than overestimate pediatric hospitalizations, even if 40% of their dataset is composed of children with incidental SARS-CoV-2 infection. The CDC estimated that by September 2020 65,040 children had been hospitalized with COVID-19. Importantly, they state that “Probable, asymptomatic, and travel-associated cases were excluded from counts of confirmed cases used in this analysis.” Currently, an estimated 192,000 children younger than 17-years have been hospitalized according to the CDC’s Estimated Disease Burden of COVID-19.
Neither Mr. Zwieg nor Drs. Beck and Gandhi discussed these particular datasets, the CDC estimate, or how the new studies might impact these numbers.
What can the studies teach us? Framing matters.
Taken together, the studies reveal two key points. The obvious one is that when all children admitted to the hospital are screened for COVID-19, asymptomatic cases are common. This is an important point, though not a particularly surprising one given that asymptomatic SARS-CoV-2 infection has been known to be common in children since early in the pandemic. Tallies that do not attempt to tease out this difference – and it is clear some do not – could certainly inflate the number of hospitalized children by a significant amount. These studies offer an important warning to future researchers that all hospitalized children with SARS-CoV-2 are not hospitalized because of SARS-CoV-2. As lead author of one of the studies Dr. Roshni Mathew said, “Just knowing that a child is hospitalized and has the virus is not enough information to determine if they are actually sick with COVID-19”.
Second, these studies demonstrate that children admitted with symptomatic COVID-19 are often very sick. Keep in mind one of the studies excluded 10% of children who were diagnosed with MIS-C. Even after this, many children needed ICU-level care, some were intubated, and two died, points that were neglected by many in discussions of these studies.
Perhaps the most interesting lesson is how these studies can be framed in different ways to portray drastically different pictures of how COVID-19 affects children, especially when controversial topics such as school closings are relevant. Stressing the high percentage of incidental COVID-19 cases led to headlines such as Studies Suggest Child Hospitalization Numbers From COVID Are Inflated, Studies Find Hospitalization Data Overstate Kids’ COVID-19 Risk, and The COVID Panic is Over. Let’s Stop Punishing The Innocents – Our Kids.
Yet, I can frame these studies in a much more pessimistic way. One study examined 117 hospitalized children who tested positive for SARS-CoV-2, and 55% were hospitalized for symptoms due to COVID-19. Of all children with SARS-CoV-2, 20.5% had severe or critical illness and 26.5% required ICU admission due to COVID-19 or MIS-C. Five required invasive ventilation and one died. The other study examined 163 hospitalized children who tested positive for SARS-CoV-2, and 64% were hospitalized for symptoms due to COVID-19. Of these 163 children, 17 had MIS-C and another 20 were “significantly symptomatic” needing respiratory support or ICU-level care. One child died. A journalist could use these studies (and others with similar findings) to write a perfectly accurate article titled “Severe COVID is Common in Hospitalized Children”.
Even noting that children are frequently asymptomatic carriers of SARS-CoV-2 can be framed in a way that is not reassuring to many people. Older teachers may not feel safe returning to classrooms full of unvaccinated children. Parents of high-risk children (or parents who are high-risk themselves) similarly may not feel comfortable sending their children back to crowded schools after reading these papers. One could easily imagine a journalist using this fact in an article urging that vulnerable teachers and children be kept home. My hypothetical, fearmongering journalist could even reference an article by Dr. Gandhi, who last year authored an article titled Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19.
It is critical that the risks of COVID-19 to children be portrayed accurately
Of course, there is no conflict between these two ways of framing the data. The studies clearly show that asymptomatic SARS-CoV-2 infection is common in children and a small minority will become quite sick, needing ICU-level care. A very small percentage will die. Balanced discussions acknowledge all of these facts. We will never know the exact number of hospitalized children. There are factors that can lead to both an undercounting and overcounting of cases. Balanced discussions acknowledge both of these potential errors.
Even if the final best estimate of hospitalized children turns out to be only 60% of the current best estimate, 60% of a large number is still a large number. If one assumes every hospitalized child was accounted for and that incidental SARS-CoV-2 infections were included in both the COVID-NET and AAP tallies at the 40% rate found in these studies, this means a minimum of 20,000 children have been hospitalized. That’s not nothing, especially when up to 30% are sick enough to go to the ICU. If we instead use the CDC’s estimate of 192,000 children and assume it too is inflated by 40%, this means 115,000 children have been hospitalized.
Drs. Beck and Gandhi write that “via these studies, parents and policy makers should be reassured that pediatric hospitalization for severe COVID-19 disease is indeed rare.” This does not seem to be a valid conclusion from the papers. Just because some children are incidentally found to have SARS-CoV-2 on hospital admission, we cannot then conclude that severe COVID-19 disease is “rare”. Study author Dr. Mathew noted his research doesn’t accurately measure the rate at which kids get sick with COVID-19. Dr. Stefan Baral similarly noted that the hospital datasets used in these studies “were not designed to infer the prevalence and severity of an infectious virus”.
Of course, we also lack a shared definition of “rare”. With polio, 70% of children have no symptoms and less than 1% develop flaccid paralysis. Of the 1% of children with flaccid paralysis only 2-5% died, though this number would certainly be smaller today with modern medical care. Are the harms of polio rare? While I fully agree that the rate of severe COVID-19 is low in children, uncommon outcomes multiplied many millions of times add up. Even reducing the “official estimate” by 40% still means that tens of thousands or even over 100,000 children were hospitalized. This fact was mostly absent from discussions on these studies, and reasonable people might not consider this outcome “rare.”
Additionally, the CDC has documented 3,742 cases of MIS-C. 60-70% of these patients are admitted to intensive care and 1-2% die. During the peak of the pandemic, up to 100 children were hospitalized every week in the UK with MIS-C. Serious conditions such as MIS-C are also prone to undercounts. Recently, Texas Children’s Hospital reported it has cared for more than 150 young patients with MIS-C, even though the official CDC tally for all of Texas is less than 100 cases. As Dr. Lara Shekerdemian, chief of critical care at Texas Children’s said, “If our hospital has seen well over 150, then clearly that number is not accurate”. According to Dr. Shekerdemian, about 75% of children with MIS-C need ICU-level care. Though the death rate is mercifully very low, between 437 and 582 children have died in the US. Again, that’s not nothing, and, excluding infants, COVID-19 will be one of the top 10 killers of children during the pandemic. Beyond these direct harms, tens of thousands of children have been orphaned, and it is a near certainty that some of these deceased parents contracted the disease from their children. The fact that many asymptomatic children screen positive for SARS-CoV-2 on hospital admission doesn’t change any of these numbers.
The toll COVID-19 has taken on children equals or exceeds that of several other vaccine-preventable diseases prior to vaccines being discovered, even with much of normal life suspended. Drs. Beck and Gandhi also write that the risk of COVID-19 to children should be “contextualized in comparison to other common respiratory illnesses (i.e. influenza and RSV)”. In the past three years, with society open and normal, the flu killed an average of 176 children per year. During the 2020-2021 flu season, with COVID-19 restrictions in place, the CDC recorded just a single pediatric death. Clearly, COVID-19 is much more dangerous to children than the flu. (I was unable to find data for RSV this year).
Additionally, we still have much to learn. Admissions where SARS-CoV-2 infection was deemed “incidental” in these studies, such as seizures, diabetic ketoacidosis, and even appendicitis might not turn out to be incidental after all, a possibility acknowledged by Kushner et al. Moreover, the potential long-term effects of COVID-19, if any, won’t be known for years. Some children, even those who weren’t sick enough to be hospitalized, may not fully recover. Some children have not regained their sense of smell and taste. At least five American hospitals have opened “long-haul clinics” for pediatric patients. Some children, even those without symptoms, meet criteria for thrombotic microangiopathy, which causes small clots in blood vessels. The long-term significance of this, if any, is unknown. The study author, Dr. David Teachey said, “The biggest take-home message for me is we still have lots to learn about SARS-CoV-2 in children and adults. We should not make guesses about the short- and long-term impact of infection in children.” I agree.
Even among the vast majority of children who do fully recover, some were nonetheless quite sick for a period. Estimates from the UK are “that 12.9% of UK children aged 2 to 11, and 14.5% of children aged 12 to 16, still have symptoms five weeks after their first infection”. According to another study, less than 2% of children had symptoms lasting longer than 8-weeks, a fact celebrated on Twitter by Drs. Gandhi and Beck as “good news” and “great to know”. However, as the CDC estimates that over 26 million American children have had COVID-19, this means that about 500,000 children had symptoms for 8-weeks or longer.
From recent research, 98% of kids with Covid recover in 8 weeks or less.
From recent research, about 500,00 American children have Covid symptoms 8 weeks or more.
Both of these are saying the same thing.
Pay attention to how data is framed. pic.twitter.com/ijGFmO9Xx6
— Jonathan Howard MD (@19joho) May 31, 2021
Reasonable people many not consider this number to be “good news”. Many of these affected children don’t show up in any statistics currently. It will take years before researchers are able to adequately quantify how COVID-19 affects children.
I believe that those writing about COVID-19 and children should present these basic facts and raw numbers so readers can decide for themselves if they feel the harms to children are “rare” or not. Reasonable people may look at how COVID-19 has harmed some children and conclude these harms are not “rare.”
To be clear, I am very optimistic for the US and other countries fortunate enough to have access to vaccines. Barring a nasty variant, the worst is over for America and its children. Cases and deaths are falling. It’s beautiful. Thanks to vaccines and the virus itself, there’s enough immunity that COVID-19 will never overwhelm an American city again, and there are hopeful signs that this immunity will persist for years. I fully hope and expect that schools will be able to open safely this fall and was very happy to learn schools will be open for my children. However, COVID-19 is not gone, and it probably never will be. Vaccine uptake remains depressingly low in large swaths of the country. Millions of children have been vaccinated, but most are not and many never will be. COVID-19 remains nearly as dangerous as ever for the unvaccinated.
These studies have made an important contribution, and everyone should welcome the notion that COVID-19 has hospitalized fewer children than initially thought. Drs. Gandhi and Beck wrote eloquently on the harms of school closures and social isolation. These harms are real and they must be part of the conversation, though we are just learning about these as well. There some hopeful signs the harms of school closures may not be as great as initially feared.
Conclusion: COVID still hurts kids
Millions of children have contracted COVID-19. Millions more remain vulnerable. Discussions on COVID-19 and children should acknowledge the totality of how it affects them. No one benefits when the risks are sensationalized or completely glossed over. This is true for both the harms of the virus and the restrictions enacted to contain it. The vast majority of children who get COVID-19 will be fine, but not all. Preventing children from getting and spreading COVID-19 is good. This shouldn’t be controversial. As Drs. Gandhi and Beck write “It is critical that the risks of COVID-19 to children be portrayed accurately”.
Indeed.
ADDENDUM: Seen yesterday on Twitter:
Tomorrow's @CDCMMWR will have details on "troubling data regarding the hospitalizations of adolescents with COVID-19," @CDCDirector said at today's @WHCOVIDResponse briefing https://t.co/zult2HNXya pic.twitter.com/7Kbcqrmxb9
— Alexander Tin (@Alexander_Tin) June 3, 2021
It might well be necessary to update this post after this study is released.

