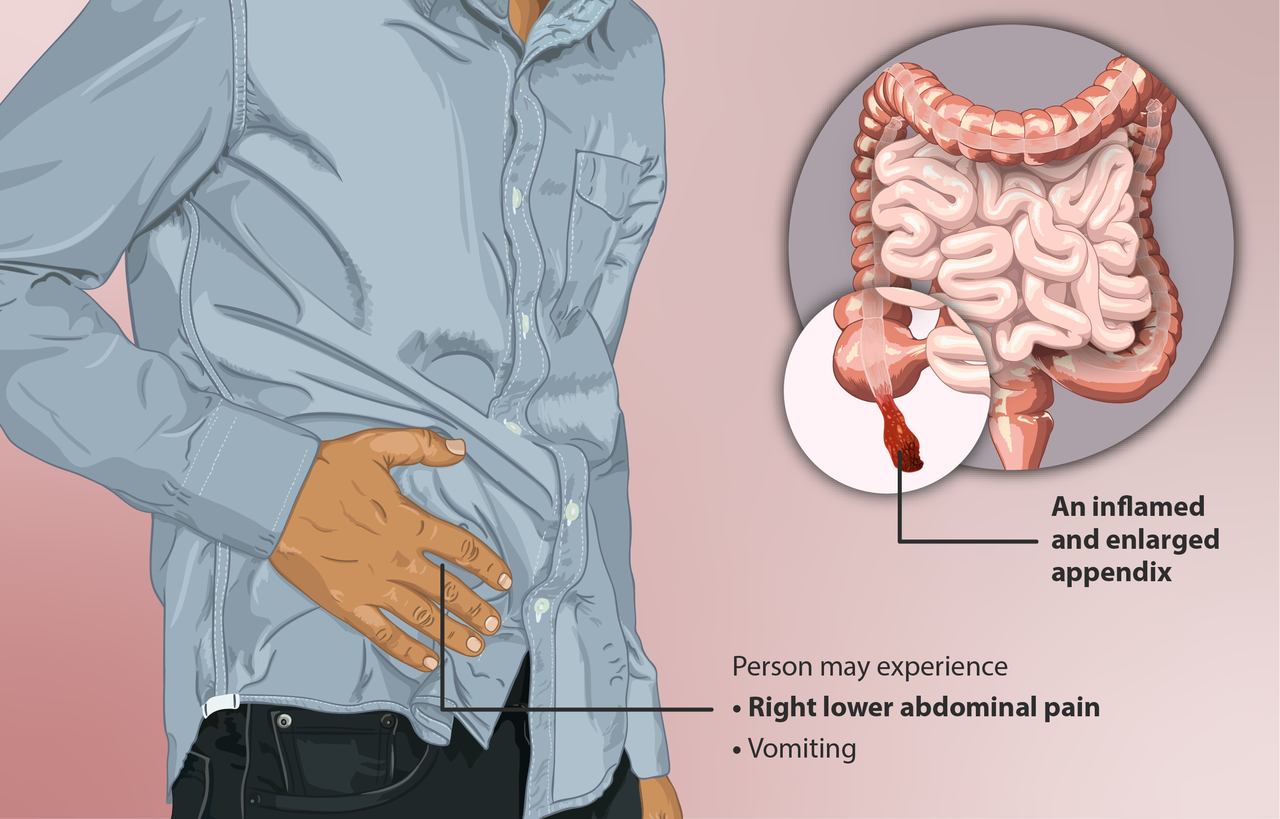
The standard treatment for appendicitis has long been appendectomy, the removal of the appendix. The successful use of antibiotics instead of surgery was first reported in 1956 by Dr. Coldrey in the British Medical Journal, and since then there have been several randomized trials of antibiotics in adults, but they have all suffered from flaws. They excluded important subgroups like patients with appendicoliths (“stones” in the appendix) and the sample sizes were small. Questions remained about applicability to the general population. More than 95% of patients with appendicitis still get an appendectomy. The COVID-19 pandemic has prompted doctors to reconsider many aspects of health care delivery. The CODA trial (Comparison of Outcomes of Antibiotic Drugs and Appendectomy) was reported in The New England Journal of Medicine on November 12, 2020. It included patients with appendicoliths and it recognized that not all patients prioritize the multiple outcomes related to appendicitis care in the same way. This large, pragmatic, non-blinded multicenter randomized comparative effectiveness trial found that antibiotics were noninferior to surgery. But an accompanying editorial advised, “proceed with caution”.
Study design
1,552 American adults with appendicitis were randomly assigned to get either an appendectomy or a 10-day course of antibiotics. Diffuse peritonitis was one of the criteria for exclusion from the study, but evidence of perforation on imaging studies was not, unless complications were observed. Antibiotics were initially given intravenously for 24 hours, followed by oral antibiotics for 10 days. 47% of patients in the antibiotic group were treated as outpatients. The primary outcome was 30-day health status as assessed with the European Quality of Life- 5 Dimensions (EQ-5D) questionnaire. Secondary outcomes were an eventual need for appendectomy in the antibiotic group and complications at 90 days. Outcomes were compared for patients with and without appendicoliths. Decisions about which antibiotics to use or when surgery was needed for a patient in the antibiotic group were left up to the treating doctors.
Results
Some people refused to be randomized; only 39% agreed to randomization. An appendicolith was seen on imaging in 27% of patients. Quality of life: the 30-day EQ-5D results were the same in both groups. At 90 days, 29% of patients in the antibiotic group had required appendectomy. Patients in the antibiotic group who had an appendicolith were more likely to eventually need an appendectomy: 41% compared to 25% who didn’t have an appendicolith. Most appendectomies were performed laparoscopically. Complications were more common in the antibiotic group (8.1 vs. 3.5 per 100 participants); but only in those with an appendicolith (20.2 vs. 3.6 per 100 participants). The rate of serious complications was higher in the antibiotic group than in the surgical group (4.0 vs. 3.0 per 100 participants). More patients in the antibiotic group required hospitalization for any reason, including for appendectomy (24% vs 5%). Patients randomized to surgery missed more days of work (8.73 vs. 5.26). Patients in the antibiotic group had more visits to the Emergency Department and spent more time in the hospital. There were no deaths in either group. Another consideration was the identification of unsuspected neoplasms: nine were found in surgical specimens, but there is no data on whether early detection improved outcomes.
In an accompanying editorial, Dr. Danny Jacobs urges caution. He would recommend surgery for uncomplicated cases and he thinks most providers would agree. But he acknowledges that the advantages of the antibiotic option may be greater during public health emergencies like the COVID-19 pandemic. He mentions the dreadful health care disparities in our society and the adverse impact of social determinants, structural bias, and racism. He recommends that individual characteristics, preferences, and circumstances be taken into consideration. The effects of racial or ethnic group, location, insurance status, and socioeconomic status may affect quality of life and could lead to poorer outcomes.
Conclusion: Much to think about
There were patients with appendicitis long before surgery was feasible and before antibiotics were developed. And not all of them died. Some lucky individuals recovered with no treatment of any kind. Not treating is no longer a serious option for most people except perhaps for the few who believe in faith healing, but which option is best for the individual patient? There are many factors to consider, but at least now we have more information to go on. For one thing, this new study tells us the presence or absence of an appendicolith can make a difference. And we can involve patients in more realistic informed consent.

