A COVID-19 clinical trial gave patients the equivalent of two full bottles of vitamin D (200,000 IU) in a single dose.
Vitamin D has long been thought to play a role in supporting immune function, in addition to effects on muscle and bone. Given many people live where there is inadequate sunlight to support vitamin D synthesis for parts of the year, there has been widespread interest in the possible role of vitamin D supplements to help raise vitamin D levels, and possibly prevent infection or minimize the severity of disease. Last September, Dr. Anthony Fauci noted that he was among the millions of Americans that take vitamin D supplements, elevating interest in this supplement. Now a new randomized controlled trial investigates the effects of a single massive dose of vitamin D in hospitalized COVID-19 patients.
What did we already know about COVID-19 and vitamin D?
Dozens of observational studies published since the pandemic began have examined the relationship between vitamin D and COVID-19 infections. Other publications have tried to make sense of all of these studies. The National Institute for Health and Care Excellence (NICE) published guidelines on vitamin D and COVID-19 in December 2020 which incorporated a comprehensive evidence review. It found little evidence for vitamin D to prevent COVID-19 infections:
The panel discussed the evidence for the association of vitamin D status with COVID‑19. They agreed that low vitamin D status was associated with more severe outcomes from COVID‑19. However, it is not possible to confirm causality because many of the risk factors for severe COVID‑19 outcomes are the same as the risk factors for low vitamin D status. Vitamin D is a negative acute phase reactant, meaning its serum concentration falls during a systemic inflammatory response, which may occur during severe COVID-19 illness. Therefore, it is difficult to know if low vitamin D status causes poorer outcomes or vice versa.
The panel discussed the significant limitations in the retrospective association studies. These included historic and inaccurate vitamin D status measurements, lack of generalisability to UK practice, the likelihood of confounding and general low quality of the evidence.
The panel reviewed only one controlled trial that used vitamin D to treat COVID-19, which used oral calcifediol (the circulating metabolite of vitamin D). While the stated outcome of the trial was positive (reduced need for ICU treatment), the panel noted several concerns with the design and approach, leading to the conclusion there remained insufficient evidence to support routine use. Notwithstanding the evidence for prevention and treatment, the panel noted that vitamin D deficiency is widespread in the United Kingdom, so it recommended the everyone should consider a supplement in the winter months, and some should continue supplementing year-round. It did not recommend vitamin D solely to prevent or treat COVID-19, except as part of a clinical trial.
Another comprehensive summary was published in January 2021 by Alberta Health Services which summarizes 12 studies, selected based on quality criteria. This review noted that most of these studies found a statistically significant difference with greater deficiency in those with COVID-19 or more severe disease. However, vitamin D deficiency may be an indicator of general nutritional deficiency, or overall health status. That is, it is possible that this is an association only, and not a causal relationship:
There is an overlap between groups at high risk of vitamin D deficiency and groups at high risk of severe COVID-19. Examples include people with chronic disease, older age, and people of Black and minority ethnic heritage, which makes assessment of observed associations between low vitamin D and COVID-19 infection challenging. Vitamin D levels may be indicative of co-morbidities that may themselves impact COVID-19 outcomes, so whether low vitamin D levels are a cause of disease or consequence of health disparity has remained a point of debate.
The report also identified three prospective randomized controlled trials assessing vitamin D in hospitalized patients with COVID-19, noting the largest trial showed no benefit.This report also noted that it is important to have adequate vitamin D levels, regardless of any potential effects on COVID-19. It recommended that health care providers and patients follow supplementation guidelines established by Health Canada.
So based on these two reviews from the United Kingdom and Alberta, there is sufficient evidence to support routine supplementation of vitamin D, but insufficient evidence to suggest that vitamin D supplementation can help prevent or treat COVID-19.
What did this new study find?
Recognizing that many people are vitamin D deficient and noting the correlation between low vitamin D status and outcomes of COVID-19, this study measured the effect of vitamin D (as vitamin D3, the version usually sold in stores) on hospital length of stay in patients hospitalized with moderate to severe COVID-19. The study is from Igor H. Murai and colleagues from the University of Sao Paulo in Brazil, and was published February 17, 2021 in The Journal of the American Medical Association.
This was a double-blind, multi-site, randomized, placebo-controlled trial that enrolled 240 patients from June through August, 2020. In order to be included participants had to be at least 18 years old, had a confirmed diagnosis of COVID-19, and clinical signs that suggested moderate to severe COVID-19. People were excluded if they were already taking vitamin D3 supplementation or had a number of other factors.
Participants were randomized to a single oral dose of 200,000 IU of vitamin D (that is 200 tablets if you take 1,000 IU tablets, a dose sold in many stores) or placebo. Rather than tablets, the study used vitamin D dissolved in peanut oil. The 200,000 IU dose was chosen as it is in the recommended range for treating individuals with vitamin D deficiency. The primary outcome measured was length of stay, but they also measured in-hospital mortality, the number of patients admitted to the intensive care unit, the number of patients requiring mechanical ventilation, and serum levels of vitamin D. After randomization the groups were fairly evenly matched, with an average age of 56 years and about 55% males.
Effects of Vitamin D supplementation
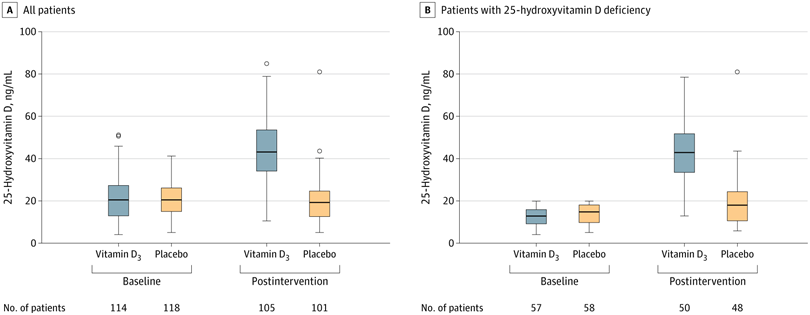
Before we look at the efficacy, let’s take a look at the effects of this massive supplement on serum vitamin D levels. In Figure 3 (below) vitamin D levels are shown on the day of randomization and also on the day of discharge. In all patients, as well as those who were admitted with a vitamin D deficiency, the vitamin D supplement significantly raised vitamin D levels:
Effects on hospitalization
There were no significant differences between the two groups with respect to the primary endpoint. This was consistent for all patients as well as those who had been admitted with a vitamin D deficiency:
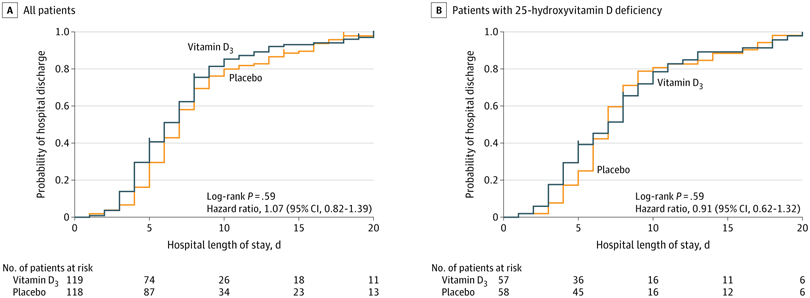 There were no significant differences between the groups for any of the secondary outcomes. No significant adverse events were reported with the exception of one patient who vomited the vitamin D dose.
There were no significant differences between the groups for any of the secondary outcomes. No significant adverse events were reported with the exception of one patient who vomited the vitamin D dose.
A companion editorial raises concerns about several limitations in the trial, which are worth noting:
First, the study was underpowered. The authors state that the number of participants was chosen on the basis of feasibility, and that with 208 participants they would have 80% power to detect a 50% difference in hospital length of stay, which is a highly improbable result. Second, the authors excluded patients who required invasive mechanical ventilation and those admitted to the intensive care unit, and less than 15% of patients required noninvasive ventilation. Accordingly, most of the patient population would be considered moderately ill and the results cannot be generalized to critically ill patients, who were excluded. This is important because the benefit of other anti-inflammatory therapies among patients with COVID-19 (e.g., dexamethasone, tocilizumab) is highly dependent on severity of illness, with moderately ill patients receiving little or no benefit and severely ill patients receiving a substantial benefit.13–15 Third, only 115 study participants (48.3%) had vitamin D deficiency (25[OH]D <20 ng/mL), and only about one-fourth of the patients had severe vitamin D deficiency (25[OH]D <12 ng/mL) (based on Figure 3 in the article12). Fourth, although the authors demonstrated that circulating levels of 25(OH)D increased in the patients who received vitamin D3, they did not measure circulating levels of 1,25-dihydroxyvitamin D, the active form of vitamin D. Accordingly, it is unclear whether patients were able to efficiently convert 25(OH)D to 1,25-dihydroxyvitamin D, because this conversion is inhibited by the osteocyte-derived hormone fibroblast growth factor 23, which is elevated in acutely ill patients.
Vitamin D doesn’t seem to help COVID-19, but supplements may still be advisable
In this randomized controlled trial, a single large dose of vitamin D had no effect on outcomes in hospitalized COVID-19 patients. This was despite the measurable effectiveness of the supplement at significantly raising serum vitamin D levels. Prospective trials with vitamin D in COVID have been relatively rare, and have suffered from poor quality and mixed results. The findings from this large trial gives more strength to the hypothesis that low vitamin D levels may correlate with poor COVID-19 outcomes, but may not be worsening them. Having said that, there is good evidence that many people have vitamin D deficiency, and supplementation may in fact be appropriate. But there is no strong evidence to suggest that supplementation will help protect you from severe COVID-19 infections.

