An important article just came out on Valentine’s Day describing the autopsy results of two people who apparently died of post-vaccine myocarditis. First off, I most certainly think that these two deaths were tragic, and second, I call for calm in light of the publication of this article. I would like to take some time to explain the nature of the analysis presented in this article – which is generally intended for healthcare workers to figure out why COVID vaccine associated myocarditis is happening.
The authors form a collaboration between the Connecticut State Medical Examiner’s office and several universities, and they analyzed two hearts of two teenagers who were found deceased 3 and 4 days after COVID vaccination. The cardiology community would have loved to have these analyses earlier in the rollout of COVID vaccination, but due to the limitations of federal law (HIPAA), the desires of families, the lack of resources, and the actual absence of real pathologists in some medical examiner offices, only very few autopsy reports are available for public viewing. The shortage of board certified pathologists is a very serious issue that deserves its own article, but let us focus on myocarditis here.
What can cause myocarditis?
The causes of myocarditis are quite numerous, and here is a partial list:
- Viruses
- Parasites
- Bacteria
- Fungi
- Protozoa
- Toxins
- Pharmaceutical and illegal drugs
- Immunological issues
What did the authors do?
What the research group in question did was to examine the hearts by eye, by some basic testing, and by microscopy slides. One boy was normal weight and the other was obese, and the heart of the first boy was of normal size and overall appearance. The heart of the second boy was quite large and dilated, which is a red flag to the cardiologist that something happened long before the present time. Why long before? As discussed in the definitive text on heart disease in infants, children, and adolescents, myocarditis is not capable of either causing substantial hypertrophy or dilation in a few days or weeks.
The team reported that the boys had no obvious symptoms and then were found deceased. While there are mechanisms by which this may happen, professional cardiologists know that this statement by itself is not sufficient evidence to guarantee that the myocarditis indeed was the cause of their demise. More information is needed, such as an overnight EKG documenting an arrhythmia. An example of a situation where there is enough proof to definitively state the cause of cardiac arrest, is commotio cordis, where a baseball player is hit by a baseball on his or her chest specifically near the heart, and ventricular fibrillation is documented.

Figure 1. Commotio cordis and its mechanism. Citation: AHA
The next part of the analysis was microscopic, and neither child had evidence of prior COVID infection by PCR. With the first child, there were findings of perivascular inflammation, scarring, and neutrophils with histiocytes. He also received molecular testing revealing two genetic mutations of unknown significance. The second child had similar cellular findings, which did support the cellular diagnosis of myocarditis in both cases. The authors then concluded that a “stress cardiomyopathy” was likely present in these children based upon the specific pattern of injury. They also mentioned that the cellular findings of myocarditis in these cases were unusual if compared to classical biopsy findings of myocarditis.
At this point things get more controversial. The rest of this analysis (up to the action plan) will mostly be my editorializing based upon what I know about cardiology. An optimal use of this report is to perhaps give ideas to future investigators to eventually get us to a molecular mechanism and more definitive answer. The slides presented in the report do not by themselves conclusively identify COVID vaccine myocarditis as the cause of the myocarditis. The bottom line of the next few paragraphs is that I would love for there to be a complete analysis but time and resources sometimes do not permit it.
Takotsubo cardiomyopathy
Stress cardiomyopathy is something readers may have heard of referred to as Takotsubo cardiomyopathy; this word is a reference to the Japanese octopus trap that resembles the shape of the heart in this disorder.
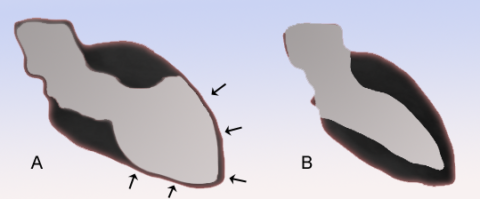
Figure 2: Schematic diagram of a heart suffering from Takotsubo cardiomyopathy (A) and a normal heart (B) from the Wikimedia Commons.
What you see is that the pointy part of the heart’s left ventricle balloons out and contracts poorly; this is classically seen after major life stressors. Takotsubo cardiomyopathy normally occurs in much older adults, and women more than men. While it is possible this is catecholamine-induced, what the general public might not know is that we give catecholamines such as epinephrine to heart surgery patients nearly all the time to support heart function, sometimes for several days, and the recipients do not all go on to develop stress cardiomyopathy. This explanation by itself should not account for the findings shown.
Next, dilated ventricles and extensive fibrosis do not develop in a few days. These problems are usually the result of weeks or months of the heart trying to heal after being damaged by some previous abnormal process. Fibrosis just means tissue replacement (in this case heart muscle) with scar tissue that cannot contract and therefore cannot help pump blood. That process could be a genetic cardiomyopathy, myocarditis, or some other process entirely such as an inborn error of metabolism. There’s also many viruses that could have been bad actors here. Any of these processes could have caused a fatal heart rhythm problem that ultimately killed these children. None of these processes require vaccinations to take place.
They mention genetic tests of unknown significance. Gene tests are done to see if a mutation in DNA was responsible for a problematic heart; the classic example that most people know about is hypertrophic cardiomyopathy. This means that a gene mutation has caused the heart to become abnormally thick. A gene mutation was picked up on the first teen (whose heart appeared normal) but not the second (whose heart was large and dilated). The gene mutations described in the first teen were present but not well-studied enough to know what they mean, otherwise known as variants of unknown significance. This happens all the time in pediatric cardiology when we are asked to sort out why a child has a large and poorly functioning heart. We do sometimes get normal gene tests in clearly malfunctioning hearts (where more in-depth whole exome sequencing may be needed). Indeed, one of the very common ways that children come to us as pediatric cardiologists for diagnosis is via minding their own business and discovering some potentially heart-related symptoms. The diagnosis may be subtle, and these two decedents have no prior medical records for us to review publicly. It is very common for dilated cardiomyopathy and myocarditis to have minimal symptoms or no symptoms at all in children until the heart starts having trouble meeting daily needs. Genetic testing to figure out why a bad heart is a bad heart is…complicated.
The authors specifically do not mention an analysis of the conduction system; this could have provided valuable insight as to the cause of any potential end-stage heart rhythm disorder.
An immunofluorescence assay paired with some blood analyses of frozen samples could have advanced our understanding of this disorder quite substantially, but they are not reported here. Immunofluorescence is the science of detecting specific cell types and proteins using certain molecules that glow in the dark. Unfortunately, they are rather expensive and only certain hospitals have the capability to run these.
For all these reasons, reporting to the public that these children definitely died of postvaccine myocarditis is not entirely supported by the data. More analysis is necessary. Cardiomyopathies of other types could still have accounted for the pathological findings above. It is not yet possible to make sweeping conclusions based upon this paper alone, rather, this should serve as a stepping stone for other investigators to perform more in-depth analyses.
What should we do next?
Based on the knowledge added by these two deaths, what are our options and recommendations for COVID-19 vaccinations and treatment? Based on medium-to-high certainty evidence, my opinions are:
- It is unwise to withhold vaccination just because one is afraid of the side effects, especially for those who have never been diagnosed with COVID-19; getting entirely unvaccinated people to their first vaccination should be a global priority. In locations that have high SARS-CoV-2 transmission, boosting should also be emphasized. Vaccination gives you a better chance of getting only mild COVID disease. Dying is not the only nasty outcome of COVID (even in kids). People with comorbidities do indeed fare poorly, but even people with minimal comorbidities can get ill, as is being more frequently demonstrated with long COVID.
- Virus-derived immunity in the absence of vaccination is irregular and sometimes not helpful at all. The COVID omicron variant has quite substantial immune escape. At bare minimum, those who are unvaccinated and recovered from COVID should consider the benefits of hybrid immunity (getting vaccinated at least once after SARS-CoV-2 infection).
- Nonpharmaceutical interventions remain important (ventilation, masks, handwashing, etc.).
- Paxlovid is just now starting to be available, but distribution and scarcity remain and issue.
- The highest risk groups for postvaccine myocarditis are older teen boys and young men, especially in the 1st week after each dose. However, it is not necessary to be frightened of myocarditis (and especially no reason to be frightened of pericarditis). Three potential methods for decreasing risk exist:
- spacing out the first two doses by at least 8 weeks
- using Pfizer instead of Moderna for the people younger than 40 (those younger than 5 years and older than 40 have a substantially lower risk of myocarditis)
- use a protein subunit vaccination if your country makes these available (Novavax, Soberana, but the most effective vaccine is the one you can access most easily)
- The symptoms of myocarditis are a mixture or subset of chest pain, dizziness, palpitations, abdominal pain, fatigue, exercise intolerance, fever, and shortness of breath within the first week after vaccination. If a family member has these symptoms they should immediately seek out medical care.
At the point the real cause of postvaccine myocarditis remains unknown, but the immunology community has a few working ideas. While the cause is unknown, the majority of these patients who sustain post-vaccine myocarditis do well, and the treatment regimens for myocarditis have an extremely long track record of safety. Greater collaboration between immunologists, cardiologists, and pathologists could help us get some definitive answers on why this happens and how to decrease the risk in future mRNA vaccination technologies (of which many clinical trials are currently being conducted for other diseases).