Almost every week there a new story about vitamin D and its relationship with some health outcome. There is a long list of observational studies have linked low vitamin D levels to a range of illnesses. This has driven widespread interest in supplementation, as well as the interest in testing vitamin D levels in the blood, in the hopes that apparent “deficiencies” can be identified and treated. Back in 2016 I summarized a narrative review that looked at vitamin D use for multiple health outcomes. It concluded that the evidence for supplementation was unconvincing for most uses. In that post, I noted that there was little evidence to show supplementation had any meaningful effect in cancer, but better quality evidence was needed. Recently a new paper was published that examined the relationship between vitamin D levels and colorectal cancer risk. Colorectal cancer is a very common cancer (your lifetime risk is about 4.2%) and any intervention to reduce the overall incidence of cancer would offer significant public health benefits. I took a closer look at the new paper to determine if my 2016 assessment required revision. Key questions include (1) the relationship between blood levels of vitamin D and colon cancer incidence, and (2) whether or not vitamin D supplementation has any relationship with colon cancer. As you’ll see these are two very different questions.
The evidence thus far
Vitamin D has for some time been associated with colorectal cancer, in the belief that it can lower colorectal cancer risk via antiproliferative, pro-apoptotic, and anti-angiogenic properties
Back in 2016 I referenced a meta-analysis of existing randomized controlled trials of vitamin D supplements, with or without calcium, which looked at an range of outcomes, including cancer. It looked at seven trials for cancer, involving over 48,000 patients and noted that supplementation “lay within the futility boundary, indicating that vitamin D supplementation does not alter the relative risk of any of these endpoints by 15% or more.” The authors’ conclusion was that “Future trials with similar designs are unlikely to alter these conclusions.” I had also noted that the Cochrane Review had also concluded that there was a lack of evidence to support vitamin D supplementation:
There is currently no firm evidence that vitamin D supplementation decreases or increases cancer occurrence in predominantly elderly community-dwelling women. Vitamin D₃ supplementation decreased cancer mortality and vitamin D supplementation decreased all-cause mortality, but these estimates are at risk of type I errors due to the fact that too few participants were examined, and to risks of attrition bias originating from substantial dropout of participants. Combined vitamin D₃ and calcium supplements increased nephrolithiasis, whereas it remains unclear from the included trials whether vitamin D₃, calcium, or both were responsible for this effect. We need more trials on vitamin D supplementation, assessing the benefits and harms among younger participants, men, and people with low vitamin D status, and assessing longer duration of treatments as well as higher dosages of vitamin D. Follow-up of all participants is necessary to reduce attrition bias.
The new study
This new study, entitled “Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts ” is an analysis of 17 studies that looked at the relationship between circulating vitamin D levels in the blood, and the relationship with colorectal cancer. It was funded by the National Heart, Blood, and Lung Institute and the National Cancer Institute. This was not a study that looked at supplementation. The authors combined data sets to give a final count of 5,706 patients that had developed colorectal cancer, and 7,107 patients that had not. All of the studies had collected blood samples pre-diagnosis, and all tested for 25(OH)D or 25-hydroxyvitamin D in a consistent manner (which allowed pooling) as all were part of the international Circulating Biomarkers and Breast and Colorectal Cancer Consortium. (25(OH)D is the commonly-accepted measure for vitamin D levels in the body.) Those with cancer were matched according to main characteristics (gender, age, etc.) The authors then estimated the risk of cancer by the absolute (pre-cancer) blood concentration of 25(OH)D.
There was voluminous statistical analysis done, and I will leave it to methodologists to appraise. The population studied was mainly white (83.9%), fairly evenly split male/female, and the median age at blood draw was 60 years. The median time from blood draw to cancer diagnosis was 5.5 years. The authors created quintiles of 25(OH)D measurements, using the 3rd quintile as the reference. In a logistical regression model, participants in the lowest quintile had a 23% greater risk of colorectal cancer, and those in the highest quintile had a 21% lower risk of colorectal cancer. This trend was observed even after adjusting for exercise, body mass index (BMI), recognized non-dietary colorectal cancer risk factors, and alcohol consumption. They also adjusted for seasonal variation in vitamin D levels. Figure 1 shows the key observation well, showing risk decreasing as levels are higher. You can also see that the association was stronger in women than in men.
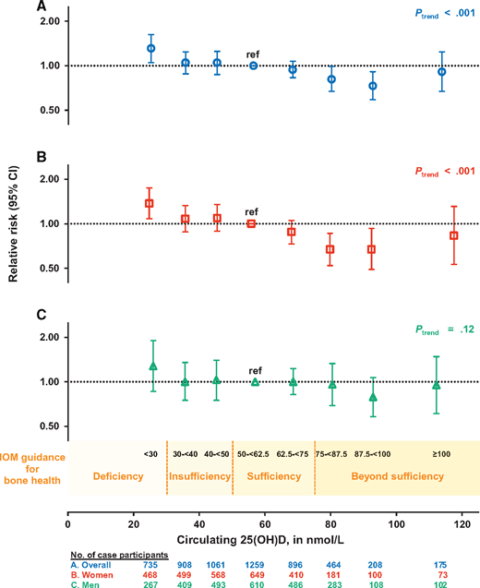
Pooled multivariable relative risks (RRs; indicated by open symbols) and 95% confidence intervals (CIs; indicated by vertical lines) of colorectal cancer according to categories of season-standardized circulating 25-hydroxyvitamin D (25(OH)D) concentrations (A) overall, (B) in women, and (C) in men. 25(OH)D categories correspond to Institute of Medicine (IOM) recommendations for bone health.
The authors found that colorectal cancer risk decreased steadily and significantly with increasing pre-diagnosis 25(OH)D levels, up to 100 nmol/L. Circulating 25(OH)D at levels below 30 nmol/L (considered “deficient” by the IOM) was associated with a 31% greater risk of colorectal cancer compared with 50 to <62.5 nmol/L, the lower range of 25(OH)D considered sufficient for bone health. Interestingly, colorectal cancer risk was lower at 25(OH)D concentrations that are higher than those currently considered sufficient for bone health. What this study doesn’t answer, and can’t answer, is whether or not people with higher vitamin D levels (and lower rates of colorectal cancer) differed in some unobserved way from those with lower levels. This could mean that vitamin D isn’t the causative factor at all.
The bottom line
The evidence for supplementation with vitamin D is not that convincing. However, given the modest benefit, low cost, and relative lack of side effects, vitamin D supplementation at modest doses is safe and is not likely to cause harm. This newest study does not show that there is a benefit to supplementation, however it does show a positive association with higher levels. How those levels may have become higher (diet vs. supplementation vs. sun exposure) was not explored in this study. While this new study shows what appears to be a relationship between vitamin D levels and colorectal cancer, it doesn’t tell us anything about supplementation itself. At this time, there is little support in treatment guidelines for vitamin D supplementation to prevent colon cancer. However, it adds to the body of evidence about vitamin D and cancer. It would seem the safest things to do to avoid colorectal cancer would be to ensure that you’re getting adequate vitamin D in your diet, and, perhaps more importantly, you’re addressing the biggest factors for colorectal cancer prevention. Until better evidence emerges, continuing to take a cautious approach to vitamin D supplementation seems the most reasonable approach.

