As discussed numerous times on the pages of Science-Based Medicine, children are increasingly a target of chiropractors, with some even pushing for recognition as primary care practitioners. Despite a thoroughly inadequate training, and a lack of experience with ill pediatric patients, they believe that they have what it takes to recognize and manage common pediatric conditions or refer to an actual pediatric medical professional when they deem it appropriate. While a significant percentage of pediatric illness is self-limited, and thus might appear to respond to chiropractic manipulation, I have seen many deteriorate quickly and with little warning. The idea of an ill child suffering at the hands of a charlatan is terrifying.
Many chiropractors are of course more than happy to see pediatric patients without acting as their PCP. They love to claim that children are at risk of developing misalignment of the bones of the skull and spine, chiropractic subluxations, and numerous other conditions unique to alternative medical reality, particularly during the first few years of life. They tell caregivers that these insults can be subtle, or even silent for years, and that regular maintenance care is required to prevent severe problems, even going so far as to blame SIDS and “shaken baby syndrome” on these fictional entities.
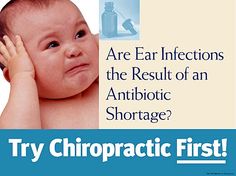
Many chiropractors are also quick to claim that they can prevent or cure some of the most common conditions seen by pediatricians and family healthcare providers, such as viral infections of the upper respiratory tract, asthma, bedwetting, and ear infections to name just a few. By simply improving the function of the nervous system, chiropractors believe that they can “boost” the immune system’s ability to fight infections, improve control over bladder function, and even reduce airway inflammation and bronchoconstriction. If you think that sounds like nonsense, you’re right!
I’d like to focus on ear infections in the pediatric population in this post, and to contrast a science-based understanding and approach to treatment, warts and all, with that of the chiropractic profession. As you’ll see, the chiropractic understanding is overly simplistic, its management makes no sense, and the research base is a house of cards toppled by the slightest breeze of skeptical evaluation.
Ear infections in kids
Infection of the middle ear, commonly referred to as “acute otitis media” or simply as an ear infection by physicians (and some chiropractors), is the most common reason for a parent to seek urgent medical care for their child. In fact, by the age of three years, roughly 90% of children will have had at least one ear infection. Many children suffer through multiple acute episodes with some even developing chronic infections that are managed with long courses of antibiotics and surgical drainage of the middle ear via the tympanic membrane or “ear drum.”
Ear infections are considerably more common in younger children, with the highest incidence in the first two years of life. It isn’t entirely clear why there is such a drop off in incidence after the early school age years. As with most pediatric conditions, it is likely highly multifactorial and the true answer is probably a combination of changes in the anatomy and physiology of the middle ear and its ability to drain, as well as an improved response of the immune system to pathogenic bacteria. Other factors that influence the incidence of ear infections in children are family history, day care attendance, breastfeeding, exposure to cigarette smoke, pacifier use, and numerous other minor items.
Not surprisingly, ear infections are also the most common reason why children receive a prescription for a course of antibiotics. This is problematic for a number of reasons. Historically, doctors have been too quick to diagnose ear infections, which has resulted in large numbers of unnecessary prescriptions for antibiotics. This has almost certainly played a role in the development of resistance to common antibiotics and has caused more harm than benefit considering expense and adverse events like allergic reactions and colitis caused by overgrowth of Clostridium difficile in the gut.
How are ear infections diagnosed and treated?
Physicians diagnose acute otitis media (AOM) based on direct visualization of the tympanic membrane using an otoscope, with some versions even providing a magnified view to aid recognition. In general, we look for the presence of purulent fluid in the middle ear that is causing an outward bulge of the drum. Just as important however, is the clinical assessment of the signs and symptoms of the child’s illness and an understanding of the caregivers’ perception of them.
Ear infections have been misdiagnosed and overtreated for a variety of reasons. Looking at the ear drum of a squirming child with an ear full of wax is extremely difficult. And even with a cooperative child it isn’t always easy to get a great look. Pediatricians are also human and we sometimes see what we want or expect to see, especially when the pressures of time, nervous parents, and a genuine desire to help children get better are added to the mix.
Until 2004, when the AAP released a new set of guidelines for the diagnosis and treatment of AOM, the criteria were fairly subjective and there weren’t strong recommendations for a wait-and-see approach. In 2013, the AAP further refined diagnostic criteria, making them considerably more simple and objective. Unfortunately, evidence from 2010 suggested that pediatricians largely ignored the 2004 update on treating acute otitis media. We continued to give out antibiotics like candy on Halloween and increase our use of newer and broader agents that don’t improve outcomes. I look forward to seeing if the 2013 update leads to better care but I’m not exactly holding my breath.
Don’t get me wrong, I’m not saying that antibiotics don’t play an important role in the treatment of ear infections in kids. When used appropriately, they work amazingly well. They reduce pain associated with ear infections, which can be severe, speed recovery tremendously, and reduce the risk of potentially severe complications such as spread of infection to surrounding tissue of the head and neck, even meningitis.
There is a bit of a myth out there that the vast majority of ear infections will resolve without antibiotics because they are viral in nature. As with most complex medical concepts, this is partially true and partially completely wrong. It’s nuanced. Based on the studies using the latest and most sensitive techniques, only about 5% of ear infections are caused by viruses alone. Most are caused by a combination of viral and bacterial pathogens, which makes sense because most ear infections occur in the setting of a viral upper respiratory infection.
Based on old criteria and the studies using them, it is true that 80-90% of ear infection will resolve on their own however. But this number falls to about 50% when more stringent criteria are in place. In the real world outside of a study, many kids diagnosed with ear infections simply have a cold and perhaps just some fluid behind their ear drums rather than a true infection of the middle ear.
Because of this, it is challenging to determine whether or not a treatment actually works or just appears to work when the outcome being looked at is simply that the patient gets better. When strict objective otoscopic criteria are used to determine resolution of the infection, the number needed to treat drops from the double digits down to 3-4. This doesn’t mean that observation isn’t often a reasonable approach, as delineated in the AAP guidelines, when the patient is older than 6 months and the infection is mild. This group makes up a large percentage of ear infections. But for younger children and kids of any age with significant symptoms, assuming that the newer diagnostic criteria are used, antibiotics are absolutely appropriate.
Vaccines, is there anything they can’t do?
The overall incidence of ear infections does at least appear to be on the decline, perhaps because of attempts by the American Academy of Pediatrics to tighten up the diagnostic criteria but more likely because of the success of the 13-valent penumococcal vaccine (PCV13). Introduced in 2010 as an improvement over PCV7, PCV13 is given during early childhood to prevent infection with the 13 strains of pneumococcus most likely to cause severe illness in kids. Pneumococcus, notorious as a cause of meningitis and severe pneumonia, also happens to be the most common bacterial pathogen associated with ear infections.
For a nice science-based discussion of the diagnosis and management of ear infections in the pediatric population, here is the 2013 updated AAP clinical practice guideline.
What role does chiropractic play in managing ear infections in kids?
Despite numerous claims to the contrary, chiropractic manipulation plays absolutely no role in the management of ear infections in kids. The American Association of Chiropractic disagrees, claiming that adjustments to the back of the skull and the first cervical vertebra can improve drainage of the middle ear. If true, this would be helpful, but it is utter nonsense as no chiropractic manipulation can move the bones of the skull around without causing pain or injury, and there is no proven link between the position of the first cervical vertebra and the drainage of the middle ear.
While many chiropractors believe that their manipulations “boost the immune system,” the bulk of their claims regarding ear infections focus on drainage of the middle ear via the Eustachian tube, and for very good reason. The Eustachian tube connects the middle ear with the back of the throat and allows drainage of normal secretions and potential pathogens, but it is a two way street. When inflammation and swelling, usually caused by a viral upper respiratory infection, interfere with the function of the tube, viruses and bacteria which get into the middle ear have no way of getting out. Infection and accumulation of pus lead to symptoms and eventually diagnosis.
Young children are more at risk for infection of the middle ear partly because of their unique anatomy, specifically that the Eustachian tube is horizontal and thus does not drain efficiently. As we grow, the tube takes on a path closer to vertical. Manipulation of the spine or skull cannot change the orientation of the Eustachian tube. Other factors, such as exposure to cigarette smoke and nasal allergies, can also play a role in poor drainage.
Information from the International Chiropractic Pediatric Association, which offers certification and diplomate programs in pediatric chiropractic, is even worse. They claim that the pneumococcal vaccine is dangerous and ineffective, and that antibiotics and surgery are never necessary. The article also contains several links to articles written by Joseph Mercola, a “friend” of SBM.
Is there any evidence in favor of chiropractic?
Is there evidence that can be held up by chiropractors to support their claims? Of course there is, and lots of it. But it is evidence of the lowest order, primarily anecdotes, case series, and trials that fail to take into account the difficulty in making the diagnosis and the natural course of the infection. A perfect example is the study most commonly cited on chiropractic websites. It is a retrospective nonrandomized study of 46 children treated with adjustments and “the doctor’s own modified applied kinesiology.” 90% of the children got better without antibiotics, which is exactly what would be expected considering the difficulty in diagnosis and the fact that children with severe symptoms more consistent with a true ear infection would be less likely to go to a chiropractor as opposed to a medical doctor. The report even states that children with only isolated ear discomfort were more likely to get better sooner than those with more significant symptoms. As expected, the better-designed the trial, the smaller the effect.
Why are children with isolated ear discomfort even included in a study looking at the treatment of ear infections? More importantly, how are chiropractors even diagnosing ear infections in the first place? Pediatricians with years of training and experience looking in the ears of thousands of children of various ages and sizes find it difficult. How can a chiropractor, whose educational experience typically involves interaction with very few if any ill people, let alone children, hope to become even remotely proficient? It isn’t any wonder why so many of them believe that their intervention works because any intervention, even no intervention, would appear to be effective when the symptoms resolve on their own. These patients are getting better despite the chiropractic, not because of it.
Conclusion: Chiropractors cannot treat ear infections
Ear infections in kids are extremely common and are the leading reason for antibiotic prescriptions in young children. Science-based research has revealed that although they will often resolve without specific treatment, simple observation isn’t always the best approach and there must always be a plan in place if symptoms fail to improve or they worsen. Severe complications, although uncommon, do occur in observed and treated patients although to a lesser degree.
As in their approach to most other medical conditions, chiropractors who treat pediatric patients generally have a simplistic if not an outright inaccurate understanding of the pathophysiology of ear infections. And although it may be somewhat understandable given the difficulty in determining if a treatment actually works for ear infections diagnosed in the real world, it is still inexcusable that they even try. At best the patient gets better on their own, but a delay in appropriate care will unnecessarily prolong a child’s pain and suffering, and increase the likelihood of a complication. Parents who bring their child to a chiropractor will also likely be exposed to other forms of pseudomedical nonsense, bogus nutritional advice, and vaccine misinformation.
And then there’s this.