“Blister packs” help people take their medication on the correct schedule.
In order for medication to work, getting a prescription filled isn’t enough. You have to actually take the medication. And that’s where you (the patient) come in. Estimates vary based on the population and the medication, but a reasonable assumption is that 50% of people given a prescription don’t take their medication as prescribed. In pharmacy terminology we usually call this medication compliance, but because that sounds a bit paternalistic, the term medication adherence is also used. People forget doses, deliberately skip doses, and sometimes even take more than directed. Often, the prescription isn’t finished completely. Perhaps not surprisingly, people are less likely to adhere to their prescribed medication schedule when the condition they are treating has no symptoms. All things being equal, you’re more likely to take your pain control medicine than your hypertensive medications: Pain medications have side effects, but should help you feel better right now. Hypertension medications can only make you feel worse. Statins (as a group of medications) are another good example. We treat high cholesterol to lower the risk of heart disease: heart attacks, strokes, and death. It has no obvious benefit now, nor will we ever be able to point to the benefit we received. We’re taking the medication to reduce the risk of something happening in the future. If the drug isn’t taken regularly (or at all) then you’re not going to get the expected benefits of statin therapy. The “value” that treatment delivers is reduced (or eliminated). And if you stop a medication periodically, then restart it, you might get more side effects than you would have if you just took it regularly.
Why proper dosing is important
When medications are licensed and approved for sale, the suggested schedule for use isn’t made up out of thin air. It’s based on the accumulated scientific evidence which showed it to be effective. Bioavailability studies and clinical trials guide decisions about what an appropriate dose should be. If your antibiotic is 500mg twice a day for 10 days, that’s because that specific dosage has been shown to provide the necessary blood or tissue concentrations in order to treat the illness. If your statin medication is 10mg once per day, that dosage has been studied in clinical trials and presumably been shown to produce a benefit (e.g., a reduction in the risk of heart attack or stroke). When a medication isn’t taken as directed, there can be negative consequences. And with more and more medications being introduced that can be taken orally (e.g., about half of the newer cancer drugs are oral, not intravenous), it’s essential to find ways to ensure that people take medications safely and accurately.
Because many people forget to take their medications as directed, and may also be on multiple medications, the idea of a multi-medication compliance pack or “pill organizer” has grown. They are enormously popular among seniors who may be on several medications, each with their own dosing schedule. Some of the benefits include:
- They can automatically manage complicated dosing schedules.
- They streamline medication schedules and reduce the risk of errors (they eliminate the question “Did I take my medications today?”)
- They can reduce wastage of medication
- They can help people stay in their own homes longer, maintaining autonomy and independence
What pill organizers do, really effectively, is they monitor medication use. When an organizer is used properly, any missed doses are obvious. I have worked in many pharmacies and pill organizers are very common – not just for those in long-term care, but for anyone that is on one (or several) chronic medications and needs a tool to simplify use and help them to remember to take their medication. To be frank, I’ve never even considered the thought that they may not always be helpful, as the answer always seemed self-evident.
The study
Given my own assumptions about pill organizers, I was surprised to see recent headlines like “Pill organizers could put seniors at risk” and “Pill organizers could cause adverse effects among elderly.” The story being reported is research by Debi Bhattacharya and colleagues at the University of East Anglia. The title is long and a bit confusing: “The feasibility of determining the effectiveness and cost-effectiveness of medication organisation devices compared with usual care for older people in a community setting: systematic review, stakeholder focus groups and feasibility randomised controlled trial.”
There were multiple components to the study. Initial work looked at the best way to evaluate medication organization devices (MODs), and included a literature search as well as discussions with patients and health care professionals.
This work informed the trial design. They used a “2 × 2 factorial design” to compare MODs with usual prescription drug packaging. They also simultaneously compared providing drugs on a weekly or a monthly basis. Because of the design, there was no blinding possible.
The actual intervention went as follows:
- Potential participants were found in six medical practices. They had to be over the age of 72 and prescribed 3 or more medications.
- One third of the 288 potential participants already used a pill organizer. One quarter were deliberately not taking their medication as prescribed. These patients were excluded. There were several other rules for exclusion.
- Of the remaining 80 patients, about half were inadvertently not taking their medication as prescribed. These were included in the trial, with some exclusions.
- The researchers were left with 29 patients, half of whom were given pill organizers and half to continue as per normal.
The findings were a bit surprising. There’s actually a lack of good evidence showing that MODs improve health outcomes or quality of life. While there’s some evidence showing MODs improve adherence, there’s also some evidence showing they may increase hospitalizations.
Based on an analysis of recruited patients, the prevalence of intentional non-adherence was 24.7%. In the remaining patients, the rate of unintentional non-adherence (pre-study) was 46.1%. This was the group then randomized to pill organizers versus normal prescription packaging.
This comment from the researchers didn’t surprise me at all:
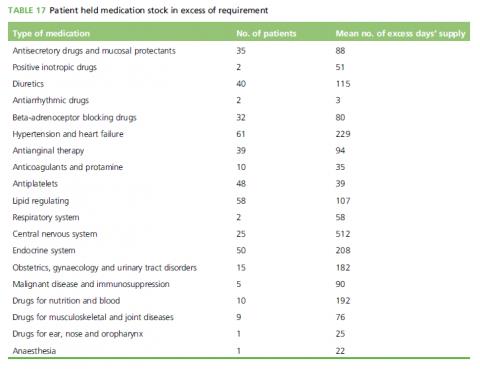
Some medications were neatly presented with the correct blisters in their original packaging in an organised fashion and others appeared to have been randomly tossed into buckets, bags and boxes. One participant, who was subsequently withdrawn from the study, had very poor eyesight and used the colours and sizes of his medicine boxes to distinguish one from another. This participant had incorrect blisters inside boxes. Many patients had medicines surplus to reasonable requirement in their possession, as summarised in Table 17. As an extreme example, one participant presented 17 unused tubes of Ovestin cream and seven unopened boxes of codeine phosphate. Many participants had excessive numbers of surplus prescribed painkillers. No patients reported any discomfort with or declined the removal from use of their old medicine stocks.
Many patients had a large excess of medications on hand:
So what were the results of being randomized to a pill organizer? Overall compliance between all groups was very good. However, in the MOD groups, there were five adverse events, including three falls, one diabetic low blood sugar event, and one event where a patient was so ill they were “trapped in a bathtub for 12 hours”. There were no adverse events in the group that had continued to take their medication as per their normal processes. The difference was calculated to be statistically significant. How could this occur? It was likely because participants were not previously taking their medication exactly as prescribed, so the MOD meant a change (and possibly an increase) in their regular dose. With the sudden changes, some experienced adverse events.
Conclusion: A little surprise
This was a small trial with surprising results, but identified a risk that could be quite real to the hundreds of thousands of people who struggle to manage their medications. While medications are prescribed with certain expectations about usage, the patient experience can be very different. It’s essential for health professionals, physicians and pharmacists alike, to understand our patient’s perspective and their habits. MODs themselves, or any other forms of pill organizers, aren’t harmful or problematic on their own. This research does show, not surprisingly, that changes in medication doses and schedules, brought on by an MOD, could raise the risk of a medication-related adverse event. We see compliance aids as a tool to help improve outcomes and patient satisfaction in the absence of evidence to show they actually do so. What I learned from this study is that any decision to use an MOD requires a collaborative discussion with the patient to carefully understand their perspectives on medication use, and ideally, some documentation of non-compliance with the prescribed schedule. Used properly, an MOD can support independence or autonomy. Used without careful planning, these devices may be inadvertently be causing harm.