Editor’s note: As you can see, the SBM server migration and template upgrade are now complete. We hope you like the new look and are hopeful that the frequent crashes and prolonged down times are a thing of the past. As much as we like it, we also know that the new look will take some getting used to. Realize that it’s a work in progress and will be tweaked over time. Finally, please don’t use the comments after this post to report issues or problems, praise or criticize the new template, or post wish lists. The comment section after our post Friday announcing the server migration is the best place for such topics. And, now, here’s the first new post after the upgrade. Enjoy!
We at SBM write a lot about placebo effects. Of course, part of the reason is that placebo effects are just plain interesting from a scientific perspective. After all, if one can relieve symptoms with inert sugar pills or other ineffective interventions because of the power of expectation, that’s something we want to understand. Also, given the mission of this blog, another major reason is that placebo effects are inextricably bound to the question of whether the alternative medicine modalities that are being “integrated” into medicine through the brand of integrative medicine actually have any useful therapeutic effects or not, aside from placebo effects. Of course, as we’ve discussed time and time again, pretty much all “complementary and alternative medicine” (CAM) or “integrative” medicine modalities that are not herbal medicine, nutrition, or exercise (which can have measurable physiological effects due to understandable physical mechanisms) have no detectable effects above and beyond placebo effects, no matter how much proponents of integrative medicine try to show that they do. There’s a reason why, given the utter implausibility of many of these treatments, such as homeopathy, reiki, and the like, I refer to integrative medicine as “integrating” quackery with real medicine; that is, when integrative medicine is not rebranding perfectly respectable science-based modalities like diet and exercise as somehow “alternative” or “integrative,” so that they can claim at least some efficacious modalities in their armamentarium and thereby imply that the quackery has value too.
That’s why I was so disturbed when a former SBM blogger e-mailed me a link to a credulous article in National Geographic that basically promotes every pseudoscientific trope about acupuncture entitled, “Here’s What Placebos Can Heal—And What They Can’t” by Simon Worrall, with the subtitle “The latest research in biochemistry reveals that your brain can actually self-medicate.” Yes, that’s like waving the proverbial cape in front of the proverbial bull. The article is an interview with Erik Vance about his new book, Suggestible You: The Curious Science of Your Brain’s Ability to Deceive, Transform, and Heal. Its blurb is not encouraging:
This riveting narrative explores the world of placebos, hypnosis, false memories, and neurology to reveal the groundbreaking science of our suggestible minds. Could the secrets to personal health lie within our own brains? Journalist Erik Vance explores the surprising ways our expectations and beliefs influence our bodily responses to pain, disease, and everyday events. Drawing on centuries of research and interviews with leading experts in the field, Vance takes us on a fascinating adventure from Harvard’s research labs to a witch doctor’s office in Catemaco, Mexico, to an alternative medicine school near Beijing (often called “China’s Hogwarts”). Vance’s firsthand dispatches will change the way you think—and feel.
Expectations, beliefs, and self-deception can actively change our bodies and minds. Vance builds a case for our “internal pharmacy”—the very real chemical reactions our brains produce when we think we are experiencing pain or healing, actual or perceived. Supporting this idea is centuries of placebo research in a range of forms, from sugar pills to shock waves; studies of alternative medicine techniques heralded and condemned in different parts of the world (think crystals and chakras); and most recently, major advances in brain mapping technology. Thanks to this technology, we’re learning how we might leverage our suggestibility (or lack thereof) for personalized medicine, and Vance brings us to the front lines of such study.
You know, someone should tell whoever wrote the blurb that being referred to as “Hogwarts” is not a good thing in medicine. Of course, I can’t resist indulging in one of my favorite quips here regarding Hogwarts and alternative medicine: What’s the difference between magic Harry Potter’s world and alternative medicine? In Harry Potter’s world, magic works. Alternative medicine, not so much.
Unfortunately, this article promotes what we at SBM have come to refer to as the “placebo narrative” in apologia for integrative medicine. If what Vance says in his interview reflects what’s in his book (and there’s no reason to think it doesn’t), then the book is basically promoting the same message. Before I look at the interview itself, though, let’s recap what we mean by the “placebo narrative.”
The placebo narrative
I consider it a truism that, as more and more rigorous clinical trials with proper blinding and controls show that popular alternative medicine modalities like acupuncture, reiki, and the like that are furiously being “integrated” into medicine have no detectable specific effects on any disease or condition distinguishable from placebo effects, increasingly integrative medicine proponents have shifted to arguing that that’s OK, that these modalities actually work through the “power of placebo.” Thus was born what Steve Novella has referred to as the “placebo narrative.” I like that term, but I sometimes refer to the placebo narrative as the myth that “thinking makes it so,” which is the basis for the rebranding of integrative medicine as harnessing “the power of placebo” or, alternatively, the power of positive thinking. Never mind that it’s highly questionable whether it’s ever worthwhile to do so and that trying to use placebo effects to intervene in real disease processes could potentially have deadly consequences by making the patient think he feels better without actually affecting the underlying pathology.
That’s not to say that there aren’t still believers out there trying to demonstrate through “bait and switch” studies that, for example, acupuncture is more potent than antidepressants (it’s not); that acupuncture is effective in relieving hot flashes, be they due to menopause or breast cancer chemotherapy or hormonal therapy (no, it doesn’t work for either); or that acupuncture is effective in improving the pregnancy rate in women undergoing in vitro fertilization (it’s not). There are even meta-analyses claiming that acupuncture “works.” One meta-analysis by Andrew Vickers claiming that acupuncture is effective for pain, is cited almost as gospel by acupuncture advocates, even though its methodological deficiencies are significant and the effect “detected” is almost certainly not clinically significant, issues detailed by Steve Novella, Mark Crislip, and, of course, yours truly. I could go on, but you get the idea. In fact, I’d argue that it’s because of how difficult it has been for acupuncture advocates to show that acupuncture and other alternative therapies work for anything that the narrative has shifted to placebos. It’s also why integrative medicine advocates like pragmatic trials so much.
Still, those who still think various highly implausible alternative medicine treatments actually work notwithstanding, increasingly the placebo narrative has become the dominant message among integrative medicine advocates to explain how the woo in integrative medicine “works.” Basically, any time you hear someone referring to the “mind-body” connection, they’re invoking a disguised form of the placebo narrative, wrapped in discredited mind-body dualism to boot.
The problem with the placebo narrative
As you might imagine if you’ve been reading SBM a while, there’s a problem with the placebo narrative—many problems, actually. These fall into two categories, in general: The scientific and the ethical. The ethical problem is easy to understand, and it’s very, very daunting for the promoters of the placebo narrative. Basically, in medicine it is very unethical to lie to patients, and inducing placebo effects requires lying to patients. Period.
That’s why integrative medicine believers have made such an effort to provide evidence that it is not actually necessary to lie to patients to induce placebo effects. The big name in integrative medicine who has done the most to promote this narrative of “placebos without deception” is without a doubt Ted Kaptchuk at Harvard. Indeed, Kaptchuk has tried repeatedly to demonstrate that it is possible to trigger placebo effects “without deception,” and three of his clinical trials are the ones often cited to argue that placebo effects don’t require lying to the patient. Unfortunately, it takes very little in the way of a critical reading of all three studies to realize that there was indeed deception in them, as well as selection bias. The advertising and the consent forms for both trials basically served the purpose of the physician telling a patient that the treatment would work. For instance, in one of Kaptchuk’s studies, which tested placebo pills on patients with irritable bowel syndrome (a syndrome very sensitive to placebo effects) emphasized how “placebo pills, something like sugar pills, have been shown in rigorous clinical testing to produce significant mind-body self-healing processes.” Another of his studies, which tested the drug Maxalt versus placebo pills for their effect on migraine headache symptoms, included in its language about the placebo: “Our second goal is to understand why placebo pills can also make you pain-free.” Not to understand why placebo pills might be able to make you pain-free or could possibly make you pain free. “Can make you pain free.” The other study, billed an open-label placebo trial for chronic low back pain, included this language:
After informed consent, all participants were asked if they had heard of the “placebo effect” and explained in an approximately 15-minute a priori script, adopted from an earlier OLP study, the following “4 discussion points”: (1) the placebo effect can be powerful, (2) the body automatically can respond to taking placebo pills like Pavlov dogs who salivated when they heard a bell, (3) a positive attitude can be helpful but is not necessary, and (4) taking the pills faithfully for the 21 days is critical. All participants were also shown a video clip (1 minute 25 seconds) of a television news report, in which participants in an OLP trial of irritable bowel syndrome were interviewed (excerpted from: http://www.nbcnews.com/video/nightly-news/40787382#40787382).
So basically, they used the same talking points from the previous study, plus clips from a news reports about happy study participants to prime the patients that placebo effects can be “powerful.” In pretty much every study of “placebo without deception,” you will find a problem like this.
None of this doesn’t mean that the science of placebo effects isn’t worth studying. The problem is that integrative medicine proponents have taken over much of the research and tried to make it conform to their preferred narrative
Enter Erik Vance
When I encountered Worrall’s interview with Vance on NatGeo, I thought Vance’s name sounded vaguely familiar. A quick search revealed him to be a science writer whose work has appeared in Discover and the New York Times. When I saw how much Vance has written about placebo effects before, I was surprised that, as far as I could tell, neither I nor any of the other SBM bloggers had written about one of his articles before, particularly given that he’s written articles like “Power of the Placebo,” complete with a placebo narrative trope, ‘Once dismissed as a curiosity, the placebo effect is now recognized as the key to the brain’s “inner pharmacy.” If only doctors knew how to open the medicine cabinet.’ Is it? Is it really?
In the introduction to the interview, Worrall informs us a bit about Vance, including that he trained as a biologist but had been raised in a Christian Science household. That’s probably why Worrall’s first question was about whether faith healing actually can work, to which Vance answered:
Wow, that’s tough! I was brought up in Christian Science, which, at its heart, believes that the world, including our bodies, is a reflection of our minds. So, if you change your mind, you can change your body.
Growing up in Christian Science I saw a lot of healings, which piqued and sustained my interest in this subject. I saw people who claimed to be healed of cancer, or a guy who cut off his toe and the toe grew back. But my hope for this book is not to prove or disprove these things I saw as a child. Do placebos and the power of the mind work? What I’ve found is yes, but not with everything. There are rules and conditions in which healing can be incredibly effective. Parkinson’s, chronic pain, irritable bowel syndrome, depression, anxiety, certain types of asthma, and autoimmune deficiencies are all very placebo-responsive. But cancer is not.
Christian Science, homeopathy, or other unproven alternative medicines may make someone feel better, but when it comes to curing a life-threatening tumor, that isn’t an appropriate place to be using these methods.
At least Vance isn’t completely unreasonable. At least he attributes some limitations to placebo medicine. (Would that some others were a bit more circumspect!) He’s also not antivaccine, as we learn when he states that his kids have all their shots and how he understands how vaccines work and therefore has full faith in them. In fact, part of the problem with the placebo narrative is how it’s taken in people who believe themselves to be scientific and who are generally pretty reasonable.
Vance is, however, dead wrong about asthma being particularly placebo-responsive—and my choice of the word “dead” is intentional because placebo medicine could easily lead to the death of asthmatic patients. Indeed it’s worth expanding a bit on a point to state that one of Kaptchuk’s own studies showed just how dangerous using placebo effects in asthma is. The CliffsNotes version is that placebos made asthma patients undergoing an asthma attack feel as though they were breathing better, but the cold, hard evidence from incentive spirometry showed that their breathing function did not improve. As Peter Lipson pointed out, that’s a good way to kill a patient, because that patient could feel less short of breath even though he is on the verge of respiratory collapse.
Vance is not incorrect when he discusses how placebo effects impact Parkinson’s disease:
Parkinson’s is the perfect disease to talk about placebos. It is a chronic deficiency of dopamine, which is one of those brain chemicals that does a lot of jobs in our bodies. One of [dopamine’s] important roles is in reward processing: how we think about good things we might get in the future.
Expectation drives placebos. And dopamine is a chemical that’s very responsive to our expectations. Parkinson’s happens to be a deficiency in the very chemical that’s very important in placebo effects and rewards.
If you look at Alzheimer’s, which does not have a high placebo response, you start to see that there are rules at play when it comes to placebos. It’s not your brain magically doing all these crazy things. There are certain chemicals we have access to and others we don’t.
It is true that clinical trials of Parkinson’s disease do report significant placebo effects. For example, Dr. Christopher Goetz examined 11 clinical trials with 858 patients and found that in drug trials 0-27% of patients experienced improvement in their symptomatology, while in surgical trials the number could be as high as 42%. (More invasive placebos produce more significant placebo effects.) Overall, 16% of patients in the placebo groups of the trials experienced improvement. Of course, I would point out that most patients with a serious disease would not be particularly happy to have only a 16% chance of improving due to a treatment. Yes, there are pharmaceuticals that are that poorly effective, usually against bad diseases, but those are exactly the drugs that integrative medicine proponents often rail against—with some justification. Yet here, Vance likes an intervention that produces such a modest result.
He also doesn’t consider that even that modest result is probably illusory.
The illusion of placebo effects
One thing not mentioned here is that placebo effects can only be quantified in clinical trials, which are, by their nature, highly artificial treatment situations. We at SBM often point out that it’s incorrect to refer to “the placebo effect,” because there is not just one placebo effect. Instead, we refer to placebo effects. Much of what is lumped together as “the placebo effect” include study artifacts that have little or no bearing on real world outcomes and/or modulation of the patient’s perception of his symptoms. Indeed, there are those who question, based on evidence, whether there is even such a thing as placebo effects. For example, in 2001 Hróbjartsson and Gøtzsche published an article in which they asked whether the placebo was powerless based on 214 studies with a total of 8,525 patients in which they concluded:
We found little evidence in general that placebos had powerful clinical effects. Although placebos had no significant effects on objective or binary outcomes, they had possible small benefits in studies with continuous subjective outcomes and for the treatment of pain. Outside the setting of clinical trials, there is no justification for the use of placebos.
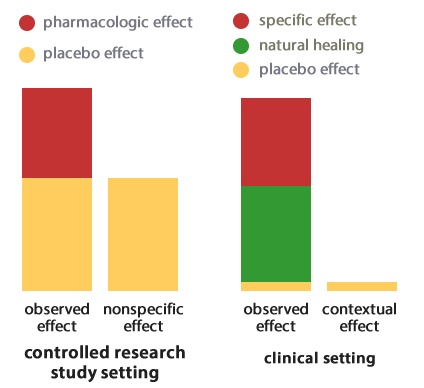
In support of the idea that much of what passes for “placebo effects” is in reality a sum of artifacts of clinical trials, Jean Brissonnet in a French language article translated by Harriet Hall pointed out that clinical trials are different. We measure many more things—and measure them more intensively. Treatments are much more standardized. Brissonnet proposes defining the placebo effect thusly, “Observed effect = specific effect + natural course of healing + a residual effect that we will provisionally call the placebo effect.”
I’m going to steal a couple of illustrations to illustrate Brissonnet point, but do read the whole article if you want the details:
Brissonnet also notes that this “placebo effect” is made up of multiple elements:
But isn’t this new “placebo effect” in turn composed of different elements? First among these are measurement errors made during the course of the trial. There are many such potential errors depending on the type of study. The best known are the phenomenon of regression to the mean, the Hawthorne effect, the Simpson paradox, the Will Rogers phenomenon, etc. (see box, below). Others come to mind: for example, an inaccuracy in the inclusion of subjects in the trial or the fact that patients tend to seek help when their symptoms are at their peak.
If all these measuring errors are subtracted, what remains can be called the “true placebo effect,” a term proposed by Ernst (1995), to distinguish it from the “false” placebo effect as traditionally conceived (figure 3).
Graphed thusly:
When you look at placebo effects this way, they become a lot less impressive than proponents like Vance portray them. I’m not sure I’m quite ready to go as far as Mark Crislip in rejecting the idea that placebo effects are even a real thing, but I have been convinced that, if placebo effects are real apart from artifacts in clinical trial construction, measurement biases, and the like, they are quite modest at best and, in the case of alternative medicine, not worth lying to the patient.
None of this is to say that placebo effects might not be useful, because it is certainly possible that doctors can enhance the perceived effectiveness of evidence- and science-based treatment by using strategies that enhance placebo effects, in particular the doctor-patient relationship. One of my favorite studies was another Kaptchuk study that actually told us something interesting about placebos. Basically, Kaptchuk randomized patients with irritable bowel disease into three groups. Subjects in Group 1 were in the wait list control and received no intervention. Subjects in Group 2 received placebo acupuncture treatments from an acupuncturist showing no empathy. Subjects in Group 3 received the same acupuncture treatments as patients in group 2 under the same conditions and in the same room, except that the practitioners interacted with them extensively. The difference was that subjects experienced an “augmented” patient interaction (45 minutes) at the first visit in which detailed questions about their symptoms were asked, including how their IBS symptoms affected their lifestyles and relationships. The interviewers asked if subjects understood the “cause” and “meaning” of their conditions and at each visit incorporated at least five primary behaviors, including a warm, friendly manner; active listening (repeating the patient’s words and asking for clarifications); empathy; 20 seconds of thoughtful silence while feeling the patient’s pulse or contemplating a treatment plan; and communication of confidence and positive expectation. At each visit, the acupuncturist would place the placebo needles and then leave the subject in a quiet room for 20 minutes. When the practitioner came back to remove the needles, he or she also made sure to exchange some words of encouragement.
The results? At the end of six weeks, Kaptchuk observed an improvement of 28%, 44%, and 62% in groups 1, 2, and 3, respectively, concluding, “Non-specific effects can produce statistically and clinically significant outcomes and the patient-practitioner relationship is the most robust component.” Basically, what we used to call a good bedside manner matters.
Even Vance seems to realize that the trappings of medicine and the practitioner-patient relationship are very important, as he says:
I also traveled to Catemaco, a town in Vera Cruz famous for its witch doctors. I met with one of the leading witch doctors there to try and understand what we call the theater of medicine—all the trappings that go into the healing practice, like the stethoscope and white lab coat. In different cultural contexts, those things change. What was interesting in Catemaco is that many of the traditional healers have adopted the theater of modern medicine. They wear lab coats, cut their hair short, and use long words, which gives them the “flavor” of what we recognize as conventional medicine.
And:
The message for doctors is the importance of being more empathetic and taking more time. You may be throwing away 30 percent of your cure just by having a poor bedside manner. If you do, you can’t be surprised if people go looking for other means of healing. The witch doctors, traditional Chinese medicine practitioners, and homeopaths I spoke to all understand this.
Of course, the proper response to this is to point out that, yes, bedside manner matters. That’s why training physicians to be more empathetic is a far better course than to embrace witchcraft like homeopathy, acupuncture, and other forms of magic that make up much of the alternative medicine being “integrated” into medicine through integrative medicine.
The seductiveness of the placebo narrative
Paul Ingraham summed up placebo effects well:
Placebo gets more love than it deserves. I am interested in the biology and psychology of placebo, but it is not a magical mind-over-matter phenomenon, or even a good consolation prize when treatment is otherwise ineffective. Many medical problems are entirely immune to positive thinking and expectation (try treating tuberculosis with a sugar pill and see how many Nobel Prizes you pick up for that innovation). The power of belief is strictly limited and accounts for only some of what we think of as “the” placebo effect. There are no mentally-mediated healing miracles. But there is an awful lot of ideologically motivated hype about placebo…
There’s a reason for this hype, though. The placebo narrative is very seductive, as I’ve pointed out many times before, for reasons that are not hard to guess. First and foremost, it taps into a deep, longstanding aspect of humans. Specifically, the placebo narrative offers the patient—and, truth be told, the physician as well—an illusion of control. What is the reward for the physician? That’s simple. These days medicine is a collaboration between doctor and patient, and, although the doctor still holds most of the power, the patient must be involved in the decision-making process. However, part of the appeal of being a physician is actually rooted in paternalism (these days, disguised under the term “patient-centered care,” where we are the nearly all-knowing physician who does what is necessary to heal the sick and the patient simply accepts whatever we deem necessary. We don’t have to tell them everything, and they don’t expect to be told everything. There is also a very real appeal to being a “shaman-healer,” who takes care of the “whole patient” spiritually as well as physically. Being able to perceive oneself as teaching a patient to “heal himself” could thus be very tempting, and there’s a reason why anthropologists are attracted to alternative medicine.
As for patients, placebo medicine literally tells them that their mind—and therefore they—can relieve their symptoms and “heal” their bodies just by unleashing some innate power within oneself to heal the body. You don’t have to have chronic pain or a serious illness to understand how appealing such an idea is. Patients love it, for much the same way that people love The Secret. It tells you that you attract what you want to yourself and that, basically, if you only want something bad enough, including healing, the universe will provide.
It’s not for nothing that I coined the term “the central dogma of alternative medicine” and concluded that that central dogma is: Wishing makes it so. The placebo narrative fits perfectly with that and is of a piece with previous religious healing traditions in which the ill pray for healing and, if that healing comes, God did it. The main difference here is that we’re told that, instead of the universe providing through a god or spirit, the universe provides through your mind—as though the mind and the body were separate things.
The reality of course, is much more prosaic and much less “sexy,” as even Vance seems to realize. Late in the interview he notes that he’s “tried a lot of alternative medicines and haven’t stuck with any of them.” Why not? If placebo effects are so powerful, you’d think Vance would have found an alternative medicine modality that he liked enough to stick with.
He also cautions:
The message for the patient is that [alternative medicine] can be effective. But I do lay out some rules for when to do it and when not to.
One is, don’t hurt yourself. If you have a life-threatening disease, that’s not the time to play with expectations.
Don’t go broke. I’ve talked to many people who’ve spent their life’s fortune chasing after healings that were never going to happen.
The last one is, don’t harm the environment. If your placebo involves endangered animals, it might be a good idea to pick a different one.
Within those rules and within certain diseases, there’s a lot you can do. Just because it’s a placebo doesn’t mean it won’t work. This has been shown again and again in laboratories.
Except that it hasn’t “been shown again and again in laboratories” that placebos “work.” It’s still not even clear that placebo effects are anything but artifacts of clinical trials.
Placebo research can be valuable, but it has, unfortunately, been largely hijacked by integrative medicine, whose adherents want to demonstrate that alternative medicine works and that placebo medicine is efficacious and therefore worthwhile. (Would that it were true!) What placebo research has shown us is not that alternative medicine works, nor has it shown us that the brain is the body’s “pharmacy” that can be tapped at will to heal all manner of ailments. Rather, what it has done is to reinforce something known since ancient times, the importance of empathy and a trusting practitioner-patient relationship. That’s more than good enough.