If you’ve perused the alternative medicine (i.e., quack) cancer literature as long as I have, you’ll recall seeing certain key narratives recurring. One such narrative, of course, is that “conventional” cancer treatments (often characterized as “cut, burn, poison”) do more harm than good. Another such narrative is that you can almost completely prevent cancer if only you eat the right foods, use the right supplements, and live the right lifestyle. There are others, of course, often based on a germ of truth exaggerated and weaponized to spread fear and suspicion of science-based cancer treatments. For example, it is true that “conventional” treatments of surgery, chemotherapy, and radiation are associated with unpleasant side effects and occasionally life-threatening risks, and diet and lifestyle can reduce your risk of cancer, but not by nearly as much as these narratives claim. (Contrary to one favorite narrative, vegans, for instance, can still get cancer.)
One other key narrative about cancer that is common not just in “alternative” cancer social media, discourse, and publications but also all too often spills over into mainstream media is that we are “losing the war on cancer”, more specifically, that we have not significantly decreased the mortality and suffering from cancer, despite a now nearly 50 year “war on cancer”, This is, of course, a narrative that has been discussed and mostly contested on SBM multiple times, including in 2017, 2018, and 2020 (before the pandemic hit, of course). It’s such a perennial topic that I expected to write a post about it in January, which is when the American Cancer Society traditionally publishes the latest US cancer statistics, but the tsunami of COVID-19 misinformation got in the way. Fortunately, recently the American Cancer Society, Centers for Disease Control and Prevention, National Cancer Institute, and North American Association of Central Cancer Registries issued their Annual Report to the Nation on the Status of Cancer, Part 1: National Cancer Statistics. Before that, in January the American Cancer Society published its 2021 cancer statistics. As in the past, the picture painted, although not simple, is far more optimistic than the narrative of “losing the war on cancer” tends to suggest, although I do expect that, as we get closer to December 23, 2021, the 50th anniversary of President Richard Nixon’s signing the National Cancer Act of 1971, we will start to see “losing the war on cancer” articles appear, as they did ten years ago, and ten years before that.
Let’s dig into the current numbers, though, shall we?
Cancer 2021, by the numbers
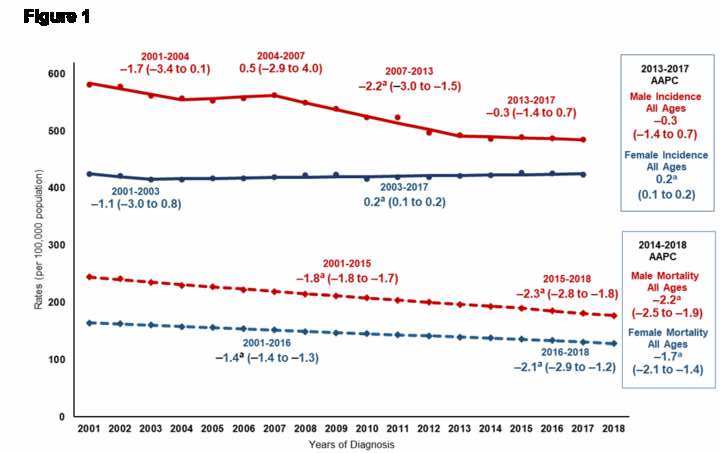
The annual report on cancer published recently looked at incidence data for all cancers from 2001 through 2017 and survival data for melanoma cases diagnosed during 2001-2014 and followed up through 2016 using data obtained from the Centers for Disease Control and Prevention- and National Cancer Institute-funded population-based cancer registry programs compiled by the North American Association of Central Cancer Registries. In addition, cancer mortality data for the years 2001 through 2018 were obtained from the National Center for Health Statistics’ National Vital Statistics System. Using this data, trends in age-standardized incidence and death rates, and 2-year relative survival were estimated, and trends in incidence and mortality were expressed as average annual percent change (AAPC) during the most recent 5 years (2013-2017 for incidence and 2014-2018 for mortality).
I’ll start with the summary of the results from the abstract, and then look at some key points:
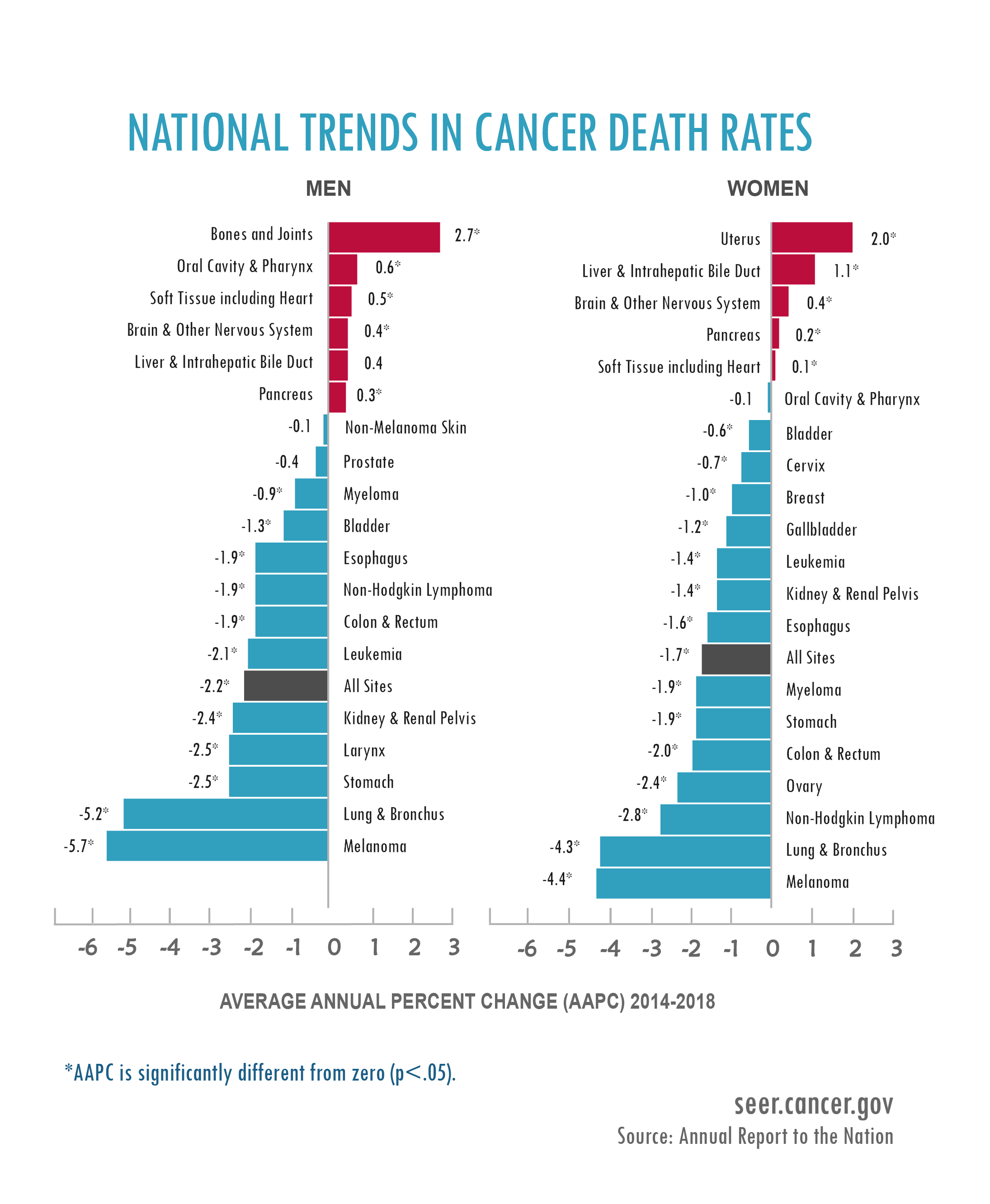
Overall cancer incidence rates (per 100,000 population) for all ages during 2013–2017 were 487.4 among males and 422.4 among females. During this period, incidence rates remained stable among males but slightly increased in females (AAPC = 0.2%; 95% confidence interval [CI] = 0.1% to 0.2%). Overall cancer death rates (per 100,000 population) during 2014–2018 were 185.5 among males and 133.5 among females. During this period, overall death rates decreased in both males (AAPC = −2.2%; 95% CI =−2.5% to − 1.9%) and females (AAPC = −1.7%; 95% CI = −2.1% to − 1.4%); death rates decreased for 11 of the 19 most common cancers among males and for 14 of the 20 most common cancers among females, but increased for 5 cancers in each sex. During 2014–2018, the declines in death rates accelerated for lung cancer and melanoma, slowed down for colorectal and female breast cancers, and leveled off for prostate cancer. Among children younger than age 15 years and adolescents and young adults aged 15–39 years, cancer death rates continued to decrease in contrast to the increasing incidence rates. Two-year relative survival for distant-stage skin melanoma was stable for those diagnosed during 2001–2009 but increased by 3.1% (95% CI = 2.8% to 3.5%) per year for those diagnosed during 2009–2014, with comparable trends among males and females.
This being the age of the pandemic, I can’t help but interject a brief comparison here. COVID-19 killed approximately 375,000 in the US in 2020. That translates to a death rate of approximately 114 per 100,000, which is disturbingly in the same ballpark as cancer deaths among females in the study described above, and the COVID-19 pandemic didn’t really hit the US in a big way until March 2020.
But let’s get back to cancer. As I write every time I discuss cancer survival and mortality statistics, cancer is not one disease. It’s literally dozens, if not hundreds, of diseases. So it’s necessary to unpack these figures and go into more detail. The news is mostly good. I also realize that, to those who have lost loved ones to cancer or who are facing imminent death from cancer, these figures might well represent cold comfort. Cancer does, after all, still remain the number two cause of death in the US, close behind heart disease, at least for now. (Cancer is expected to surpass heart disease as the number one cause of death soon and has already done so in some countries.) That means, for all the progress that’s been made in terms of declining cancer mortality, a lot of people—far too many—still die of a form of cancer and that that will continue for the foreseeable future.
That being said, what are the key takeaway points from this review of US cancer statistics? First, and most importantly, consistent with previous reports, cancer death rates are continuing to decrease. In this overview, overall they decreased 2.2% per year (on average) among males and 1.7% per year (on average) among females. During the same time period, incidence rates among men were stable during 2001-2007, decreased an average of 2.2% per year during 2007-2013, and became stable again during 2013-2017. Among females, overall cancer incidence rates were stable during 2001-2003 and increased slightly during 2003-2017 (APC = 0.2%; 95% CI = 0.1% to 0.2%). What is interesting to me in the curves (below) is how cancer incidence rates for males and females appear to be converging, with men’s cancer incidence declining to be closer to that of women, while women’s incidence rates remain mostly stable. Meanwhile, the downward trend in mortality during that same time period is unmistakable:
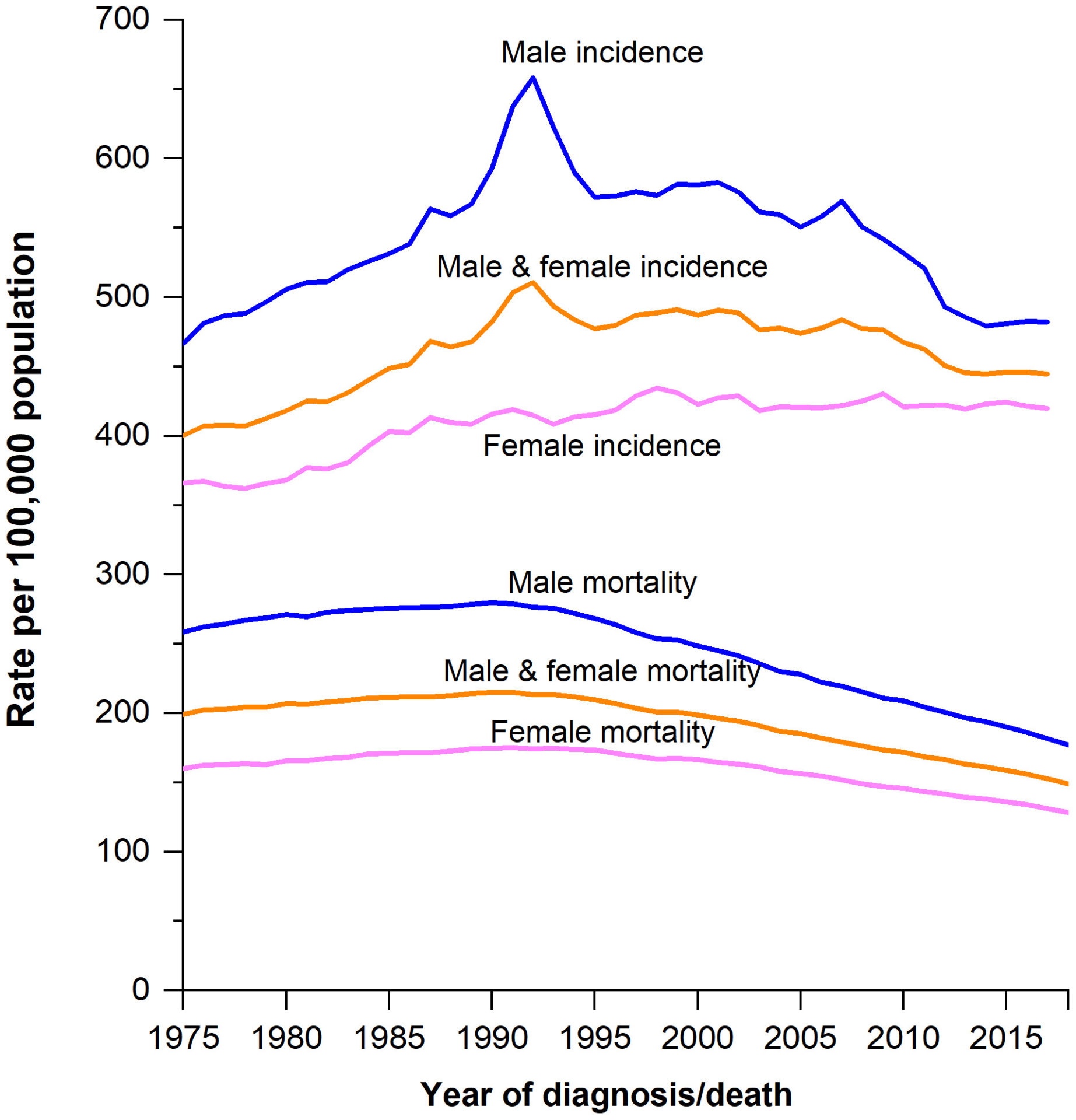
I note that these data are pretty consistent with the ACS publication in January, from which these charts were obtained. I include them because the data presented therein goes back much further, to 1975:
As you can see, cancer incidence and mortality peaked around 1990 in both men and women, with mortality having been on a steady downward trend since around the same time. This observation is likely due primarily to the effect of tobacco, which causes one of the deadliest cancers, lung cancer. Given that there is about a two decade lag between changes in smoking behavior and differences in lung cancer incidence and mortality, it makes sense that we would start to see the effects of the smoking cessation campaigns and declines in tobacco use that began in the 1960s and 1970s start to be reflected at this time.
More recently, though, declines in lung cancer mortality reflect improvements in treatment as well. As stated in the Annual Report to the Nation on the Status of Cancer:
Historical declines in cigarette smoking have been followed by declines in incidence and death rates for several smoking-related cancers, including lung, bladder, and larynx. Moreover, as reported in previous studies (27, 28) and observed in this study, lung cancer death rates have declined at a faster pace compared to declines in incidence rates since the mid-2000s, and the difference in the pace of decline has become greater in more recent years. This pattern corresponds to the timing of approval of targeted therapies and other advances in care for the most common subtype of lung cancer, non-small-cell lung cancer (NSCLC), which have resulted in increases in survival and accelerated declines in death rates for this subtype (28). In contrast, declines for small-cell lung cancer, with no approved novel treatments during our study period (29), have been similar to declines in incidence rates, with no improvement in survival rates for this subtype (28).
The first targeted therapy for NSCLC was approved by the FDA in 2003 (30), followed by the approval of several other targeted treatments, recommendations for genetic mutation testing of all individuals with non-squamous NSCLC for relevant genetic targets in 2012 (28), and the approval of 3 immune checkpoint inhibitors for NSCLC in 2015-2016 (31). Increases in the proportion of individuals with NSCLC who receive definitive therapy (32), better understanding of treatment options for older persons with NSCLC (33-35), other recent advances in care for NSCLC, such as adjuvant therapy (36) and maintenance therapy (37), and increased access to care through the Medicaid expansion (38) may also have contributed to the acceleration in declines in lung cancer death rates. Any contribution of earlier detection through lung cancer screening (39) to declines in lung cancer death rates is likely to be modest, given low utilization of screening (4.4% of eligible individuals in 2015) (40). Despite substantial declines in death rates, lung cancer is still the leading cause of cancer death in both sexes, accounting for more than 22% of all cancer deaths in the United States (27), underscoring the need for broader implementation of tobacco control interventions.
In other words, as much as the percentage of the population who smoke and use tobacco products has declined markedly in this country over the last 50 years, tobacco is still the number one cause of cancer deaths. That’s how deadly tobacco addiction is.
While the news about the modifiable cancer risk factor of smoking coupled with more effective treatments of the main cancer caused by smoking is generally good it’s not as good for others. Unfortunately, as you might imagine, obesity-related cancers are on the rise:
In contrast to the rapid decline in incidence rates of smoking-related cancers, incidence rates continued to increase for several cancers, particularly those associated with excess body weight (41), such as cancers of the female breast, corpus uteri, pancreas, kidney, and myeloma (rates rising among females only). The staggering rise of obesity (42, 43) and total sitting time (44) continues among both adults and youth. A parallel rise in death rates occurred for pancreatic and uterine cancers, and the earlier declines in death rates slowed for female breast and colorectal cancers, suggesting that for these cancers, increases in incidence rates are of sufficient magnitude to outweigh improvements in survival. Importantly, a recent study of trends by 5-year age groups showed steeper increases in incidence rates among progressively younger ages and successively younger generations for cancers of the corpus uteri, pancreas, kidney, colorectum, and multiple myeloma (18), foreboding of future burden of these cancers in the decades to come.
Besides all the other adverse health consequences of obesity, there is cancer as well. The obesity epidemic does not bode well for future cancer incidence and mortality.
Overall, though, cancer mortality is declining for most cancers:

I also can’t help but mention my clinical specialty, breast cancer, and cite what the report says about it:
Female breast cancer is the most commonly diagnosed cancer among women and among AYA [adolescents and young adults], and the second leading cause of cancer death among women. The increase of breast cancer incidence is largely driven by hormone-receptor positive cancer (50, 51), which may in part reflect continuing reduction of parity rates (52, 53), advanced age at first birth (53), the obesity epidemic (postmenopausal breast cancer) (52), high levels of physical inactivity, and increase of alcohol consumption (54, 55). As noted in the last year’s report (56), the decline of breast cancer death rates overall has slowed since 2007, and even more so since 2014, and rates have stabilized among young women since 2010, halting the progress achieved through early detection and improved treatments. Moreover, substantial racial disparities persist, as death rates are 40% higher among Black women than White women despite similar incidence rates.
At the risk of blowing my own horn too much, the cancer center where I am faculty, it turns out, is a leader in studying racial disparities in cancer incidence, treatment, and mortality. So I am acutely aware of the racial disparities that exist for breast cancer. (I should do a post about it in the future.). The conclusions in the report above are similar to those reported by the ACS report in January:
Overall cancer incidence in women has ticked up slightly in recent years after stable rates over the past couple of decades.46 This partly reflects a slowing decline for CRC coupled with increasing rates for breast and uterine corpus cancers (Fig. 3). Breast cancer incidence rates continue to increase by about 0.5% per year, which is attributed at least in part to continued declines in the fertility rate and increased body weight.47 These factors may also contribute to the continued increase in uterine corpus cancer incidence of about 1% per year,48 although a recent study indicated that this trend is driven by nonendometrioid subtypes, which are not as strongly associated with obesity as endometrioid carcinoma.49
When it comes to other cancers:
Cancer survival has improved since the mid-1970s for all of the most common cancers except uterine cervix and uterine corpus,64 largely reflecting the absence of major treatment advances for these cancers.65, 66 For cervical cancer, it may also reflect an increasing proportion of adenocarcinoma over time because of widespread cytology screening, which mostly detects squamous precancerous lesions and invasive squamous cell carcinomas.67 Screening also hinders the utility of tracking trends in survival to measure progress against breast and prostate cancers because of lead-time bias and the detection of indolent cancers.68 Gains in survival have been especially rapid for hematopoietic and lymphoid malignancies due to improvements in treatment protocols, including the development of targeted therapies. For example, the 5-year relative survival rate for chronic myeloid leukemia increased from 22% in the mid-1970s to 72% for those diagnosed during 2010 through 2016,6 and most patients treated with tyrosine kinase inhibitors experience near-normal life expectancy.69
I’ve discussed (as have others) many times the issue of overdiagnosis of indolent cancers by screening mammography programs and how difficult it is to demonstrate a definite improvement in breast cancer mortality due to mammography. The same confounding issue is generally true to varying degrees for other cancers for which we screen (especially prostate cancer), namely that it is hard to determine how much of an increase in survival is due to better treatment versus lead-time and length biases of screening, which preferentially picks up slower growing tumors and artificially inflate survival (but not mortality) rates. That is why cancer mortality is generally a better metric than survival rates for diagnosed cancers, at least for cancers for which we screen that are subject to overdiagnosis. For cancers for which we do not screen, such as hematological malignancies, however, increases in survival are generally driven mostly by improvements in treatment.
Another example of this is melanoma:
As noted in the last two annual reports and in other studies, death rates for cutaneous melanoma have declined rapidly in recent years following introduction of new therapies, including targeted and immune checkpoint inhibitors, the first of which was approved by the FDA in early 2011 (15, 56, 91, 92). In this year’s report, we present trends in stage-specific survival from 28 states and find increases in 2-year relative survival beginning in 2009 for distant-stage disease (3.1% per year). An increase in survival for distant-stage melanoma has also been documented in the CONCORD-3 study, in which 1-year net survival for cases diagnosed during 2001-2010 in the United States was stable at 43%, but it started to increase from 2010, reaching 56.6% for cases diagnosed in 2013 (93). The increase in late-stage melanoma survival in the United States slightly preceded the FDA approval of new therapies, likely because of the administration of these therapies through clinical trials and the FDA expanded access programs prior to the approval (93).
Again, melanoma is a cancer type that is not routinely screened for, at least not in the systematic way that breast, prostate, and, increasingly, lung cancer are screened for. In any event, I remember well when I was a resident in the 1990s. Although localized melanoma had a very good prognosis, metastatic melanoma was in essence a death sentence. It laughed at chemotherapy, and the only immune therapies were drugs like interferon, often at high doses that were quite toxic and didn’t have a lot of effect. However, melanoma death rates started a significant decline in 2013 among males (5.7% per year) and in 2012 among females (4.4% per year) after a period of stable trends. Finally, after decades of not a lot of progress in melanoma, science-based medicine is starting to come through. Interferon is still an important component, but newer immunotherapy drugs and targeted drugs are making a difference.
Another observation in the annual report is that cancer death rates decreased an average of 0.9% per year among adolescents and young adults (AYA), and an average of 1.4% per year among children between 2014 and 2018. I like to say that childhood cancer is an excellent example of what science-based medicine can do. Back in the 1950s and 1960s, childhood cancer was generally a death sentence. Since then, survival rates for most childhood cancers have reached the 80% range and higher.
We are not losing the war on cancer
Any strategy to combat cancer rests on three legs: Prevention, diagnosis, and treatment. Changes in diagnostic modalities can increase the apparent incidence of cancer through overdiagnosis, as well as the five year survival through lead-time bias, but they can also result in a decrease in mortality due to the cancer being screened for. As I have pointed out on a number of occasions before, there are many tradeoffs.
There is also little doubt that improvements in treatment have likely played a significant role in the declines in mortality from some cancers and improved five year survivals, but, although the overall arc is towards declining mortality and improved survival, progress is uneven. Indeed, the report concludes:
Cancer death rates in the United States continue to decline overall and for many cancer types. Furthermore, declines in death rates have accelerated for lung cancer and melanoma, likely owing to advances in treatment. However, earlier progress has slowed for several common cancers, death rates are increasing for several other cancers, and incidence rates are increasing slightly among females and in younger ages. These results inform ongoing and future efforts in prevention, early detection, and treatment and broad implementation of effective interventions, especially among under-resourced populations.
Critics of oncology and some quacks, not infrequently argue that we’re “losing the war on cancer”. (Again, just Google the phrase “losing the war on cancer”.) Arguably, we’re slowly winning, at least if you insist on using that metaphor. Mortality from cancer is declining, and for some cancers the decline has been quite dramatic just within my lifetime. For breast cancer, it’s been incredibly dramatic within my professional lifetime. I graduated from medical school over 30 years ago, and in that time mortality from breast cancer has declined by 40%, as shown in the ACS report from January. That is, quite simply, incredible to me.
Of course, it’s a painfully simplistic question, as is another question I keep hearing and have written about at least a couple of times, “Why haven’t we cured cancer yet?” (Mainly because it’s complicated.) What the evidence has shown clearly (and based on the cancer report is continuing to show) is that overall death rates from cancer are steadily falling, driven by declines in death rates from most of the common cancers. Meanwhile, five year survival rates are climbing for most cancers, even for more advanced disease.
I’ve always thought that it was hubris to think that progress would be anything other than slow against such a deadly, complex, multifactorial set of diseases that go under the label of cancer. Conquering all cancers is a project that will take more than decades. It will take generations. I also understand that the dramatic progress made is cold comfort to those who’ve lost loved ones to cancer or who are facing imminent death themselves from cancer. After all, I lost my mother-in-law to breast cancer 13 years ago, and by then the decline in breast cancer mortality since my youth had already reached dramatic levels. My wife lost her aunt to it in January, after the decline in breast cancer mortality had become truly impressive.
Even if you think that progress against cancer has been too slow, the latest cancer statistics data demonstrate conclusively that the narrative regular SBM readers hear from various proponents of “alternative cancer cures”, that cancer is killing more than ever, that big pharma doesn’t want to cure cancer, is not only incorrect but detached from reality. The actual situation is far more optimistic, albeit not universally so.